Abstract
The coexistence of sleep-disordered breathing (SDB) and hypertrophic obstructive cardiomyopathy (HOCM) has widely been recognized; however, the impact of percutaneous transluminal septal myocardial ablation (PTSMA) for HOCM on SDB remains unknown. Herein, we examine cardiorespiratory polygraph parameters in patients with drug-refractory HOCM before and after PTSMA. Forty consecutive drug-refractory HOCM patients, admitted to Keio University Hospital, and who underwent cardiorespiratory polygraphy were retrospectively analyzed. Cardiorespiratory polygraphy was performed before and after PTSMA if patients underwent PTSMA. Patients with an apnea-hypopnea index (AHI) ≥5/h were considered to have SDB. The total number of central sleep apneas, obstructive sleep apneas, and hypopnea events was evaluated. Thirty-two out of 40 patients (80%) with drug-refractory HOCM had SDB. All patients experienced relief of heart failure-associated symptoms after PTSMA. The severity of SDB was found to be correlated with left atrial diameter. The AHI decreased after PTSMA [before 15.4 (range 10.9–23.5)/h vs. after 13.1 (8.3–17.8)/h, P = 0.02]. Especially, the hypopnea index decreased after PTSMA. The average and lowest arterial oxygen saturation also increased after PTSMA (94.2 ± 1.9–95.7 ± 1.6%, P = 0.009; 81.3 ± 5.7–85.8 ± 4.8%, P = 0.012, respectively). In patients with drug-refractory HOCM, PTSMA decreased the AHI and improved arterial oxygen saturation measures. Thus, invasive treatment of the left ventricular obstruction ameliorates the severity of SDB, in addition to improving heart failure status.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hypertrophic cardiomyopathy (HCM) is a cause of heart failure, and patients with heart failure often present with sleep-disordered breathing (SDB), which is associated with increased mortality [1, 2]. The coexistence of HCM and SDB has been commonly observed [3] and the presence of SDB among patients with HCM is independently associated with worse structural and functional impairment of the heart, including atrial and aorta enlargement, worse New York Heart Association (NYHA) functional class, and worse quality of life [4]. Percutaneous transluminal septal myocardial ablation (PTSMA) is a septal reduction therapy that relieves symptoms related to heart failure in patients with drug-refractory hypertrophic obstructive cardiomyopathy (HOCM) [5,6,7,8]. Although a high prevalence of SDB in HCM patients has been widely recognized, the therapeutic effect of PTSMA for HOCM on SDB remains unknown. Therefore, we aimed to examine SDB measures in patients with drug-refractory HOCM before and after PTSMA, and evaluated the effect of PTSMA on the severity of SDB.
Methods
Ethics statement
This study was approved by the Institutional Review Board at Keio University and was conducted in accordance with the guidelines of the Declaration of Helsinki. All participants provided written informed consent.
Study design
Forty consecutive drug-refractory HOCM patients, admitted to Keio University Hospital between December 2011 and July 2016 underwent cardiorespiratory polygraphy. Patients were categorized into 2 groups based on the apnea–hypopnea index per hour (AHI/h). We compared the characteristics of patients in AHI/h ≥5 and AHI/h <5 group. Patients treated with PTSMA also underwent cardiorespiratory polygraphy after PTSMA when the apnea–hypopnea index per hour (AHI/h) was ≥5 (Fig. 1). We also compared the SDB measures before and after PTSMA.
Cardiorespiratory polygraphy
Cardiorespiratory polygraphy was performed using an unattended system (SAS-3200®; Teijin, Tokyo, Japan) which monitored the electrocardiogram, chest and abdominal respiratory effort, nasal airflow via pressure transducer, and arterial oxyhemoglobin saturation via pulse oximetry. Apneas and hypopneas were scored according to the American Academy of Sleep Medicine manual [9]. The median AHI/h was determined. SDB was diagnosed if the AHI was at least 5/h [9, 10]. The median duration between the PTSMA and post-procedural polygraphy was 7 days (interquartile range 6–9 days).
PTSMA indication and procedure
The indication for PTSMA was the presence of severe drug-refractory symptoms (NYHA class III/IV), Canadian Cardiovascular Society class III/IV or NYHA class II symptoms with recurrent exercise-induced syncope, in combination with left ventricular outflow tract (LVOT) obstruction pressure gradients ≥30 mmHg at rest or ≥50 mmHg during the Valsalva maneuver or exercise provocation. The PTSMA procedure was offered to patients referred to our HOCM clinic with refractory symptoms despite being on maximally tolerated medical therapy (beta-blockers, calcium-channel blockers, and cibenzoline or disopyramide) and were not considered candidates for surgical myectomy, owing to either comorbidities or patient preference [7]. PTSMA was performed according to a previously reported protocol [7, 11]. In brief, all patients without a previously implanted permanent pacemaker had a prophylactic temporary pacemaker inserted before the procedure. A 6 Fr femoral arterial sheath was inserted for the guide catheter system, and a 5 Fr radial sheath was inserted for a pigtail catheter placement into the left ventricular cavity. Continuous invasive peak-to-peak gradients were measured across the LVOT by comparing the peak left ventricular and aortic pressures. A septal perforating artery supplying the obstructing part of the septum was identified using coronary angiogram and cardiac multidetector computed tomography, and was chosen as the target vessel. After the occlusion of the septal target branch by an over-the-wire balloon, the perfused septal area was visualized using echocardiography after the injection of 1–2 ml of an echocardiography contrast medium. After all patients received morphine chloride intravenously for pain control, absolute ethanol was slowly injected into the target vessel through the balloon catheter. The occlusion of the target vessel was verified angiographically at the end of the procedure. Creatine phosphokinase (CK) was monitored at 8 h intervals for the first 24 h and daily thereafter for 2 days.
Echocardiography
Echocardiograms were performed at the Keio University Hospital. Conventional echocardiographic analyses including two-dimensional and Doppler were performed by technicians blinded to the patients’ clinical information.
Clinical demographic data
Patient demographic data included the prevalence of concomitant diseases, history of invasive therapies, and procedural data. Examined in-hospital events included all-cause death, sustained ventricular tachycardia or ventricular fibrillation, complete atrioventricular (AV) block, new implantable cardioverter defibrillator (ICD) or permanent pacemaker implantation, stroke, and cardiac tamponade.
Statistical analyses
Continuous data are presented as means and standard deviations (SD) or medians and interquartile ranges (IQR). Categorical variables are expressed as absolute values and percentages. To compare groups regarding baseline continuous data, we used Student’s t test or the Mann–Whitney U test for normally or not normally distributed data, respectively. Paired t tests were used to analyze the change of NYHA, left atrial (LA) diameter, average arterial oxygen saturation, and lowest arterial oxygen saturation. Wilcoxon rank-sum tests were used to evaluate the change of serum BNP level, LVOT pressure gradient, E/e′, AHI, obstructive apnea index, central apnea index, mixed apnea index, and hypopnea index. Linear regression analyses were used to explore correlations between AHI and LA diameter, and correlations between delta-AHI and AHI before PTSMA, the severity of HOCM before PTSMA, and the change of severity of HOCM before and after PTSMA. Associations of the percent change of AHI with echocardiographic and clinical indexes were assessed by Spearman’s correlation coefficient. All P values were two-sided and results were considered statistically significant at a P value <0.05. All analyses were performed using IBM SPSS Statistics 23 (IBM, Armonk, NY).
Results
Baseline characteristics
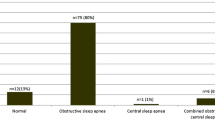
Of 40 patients with drug-refractory HOCM who underwent cardiopolygraphy, 32 (80%) had SDB. Baseline patient characteristics are summarized in Table 1. The mean age was similar between SDB and non-SDB groups. Body mass index was greater in patients with SDB than without SDB (P < 0.001). The prevalence of hypertension was greater in patients with SDB than without SDB (P = 0.047). Given that all included patients were “drug-refractory”, beta-blockers were used in almost all patients and cibenzoline or disopyramide was used in more than 65% of all patients. There was no significant difference in the prevalence of PTSMA between patients with and without SDB (69 vs. 75%, P = 0.55). Cardiac index was greater in patients without SDB than with SDB (Table 2).
Cardiorespiratory polygraphy results
The median AHI and hypopnea index in all SDB patients was 14.7 (5.8–21.6) and 6.7 (2.9–10.2) times/h. In a linear regression analysis, the severity of SDB as evaluated using the AHI was significantly correlated with LA diameter in patients had SDB (Fig. 2).
The result from a linear regression analysis examining the association between the apnea-hypopnea index and left atrial diameter in patients with drug-refractory hypertrophic obstructive cardiomyopathy complicated with sleep-disordered breathing as assessed prior to percutaneous transluminal septal myocardial ablation. AHI apnea–hypopnea index
PTSMA procedure and outcome
All patients experienced relief from heart failure-associated symptoms after PTSMA. The number of injected septal branches, total amount of ethanol, and peak CK levels were 2.5 ± 1.2, 4.0 ± 1.8 ml, and 1592.0 ± 598.4 IU/l, respectively. The incidences of complete AV block and new permanent pacemaker implantation were 17.8 and 3.6%, respectively (Table 3). Significant improvements were observed in the NYHA class, plasma BNP level, LVOT pressure gradient, and LA diameter following PTSMA as compared to pre-PTSMA assessments (Table 4).
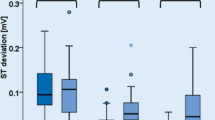
Differences in polygraph parameters before and after PTSMA
Of 22 patients treated with PTSMA, 16 patients underwent cardiorespiratory polygraphy after PTSMA. Significant improvements were observed in the AHI, central apnea index, and hypopnea index following PTSMA as compared to pre-PTSMA assessments (Table 5). The average and lowest arterial oxygen saturation also increased following PTSMA as compared to pre-PTSMA assessments (94.2 ± 1.9–95.7 ± 1.6%, P = 0.009; 81.3 ± 5.7–85.8 ± 4.8, P = 0.012, respectively). Figure 3 depicts the individual changes in the AHI following PTSMA. Delta-AHI was significantly correlated with AHI before PTSMA. However, delta-AHI was not correlated with the severity of HOCM before PTSMA, and delta-AHI or percent change of AHI was not correlated with the change in the severity of HOCM before and after PTSMA.
Discussion
The present study is the first to show that PTSMA is effective in decreasing the AHI and hypopnea index, and in increasing the average and lowest arterial oxygen saturation.
These beneficial effects could be explained mainly by a PTSMA related reduction in the LVOT pressure gradient. Septal reduction therapy, including PTSMA, confers a reduction in mitral regurgitation due to systolic anterior motion, a decrease in left ventricular end-diastolic pressure, and improvement in left ventricular diastolic dysfunction. These may, in turn, result in reduced pulmonary congestion as a triggering factor of the reflex mechanisms responsible for respiration [10]. SDB appears to be associated with an increase in sympathetic activity, which is likely to be harmful—leading to additional peripheral vasoconstriction, tachycardia, and renin–angiotensin–aldosterone system stimulation with salt and water retention [12,13,14,15]. Heart failure also results in the activation of the sympathetic nervous, and neurohormonal systems. SDB and heart failure have been a cause-and-result relationship. Radiofrequency catheter ablation of atrial fibrillation or cardiac resynchronization therapy leads not only improvement in heart failure symptoms but also a decrease in the AHI [16, 17]. Similarly, the present study demonstrated that PTSMA, one of the most effective invasive therapies for drug-refractory HOCM, led to a decrease in the AHI and the hypopnea index.
Patients with HOCM often have enlarged left atrium resulting from mitral valve regurgitation and diastolic dysfunction, and the size is closely associated with occurrence of atrial fibrillation and thromboembolic risk [18]. In our study, the AHI was significantly correlated with LA diameter. This indicates that the severity of SDB may be associated with the severity of heart failure in HOCM.
Rigopoulos et al. [19] suggested that the progression of histological changes affects the hemodynamic response after PTSMA, which occurs in 3 separate phases: perioperative, early postoperative, and late postoperative. The first phase is characterized by akinesia of the ablated septum with significant LVOT gradient decrease. In the second phase, the probable edematous expansion of the necrotic area of the septum causes an increase in the LVOT gradient in approximately half of the patients, which is evident for approximately 7–10 days without any clinical worsening, however [19]. As we evaluated the change of severity of HOCM 7 days after PTSMA, that is the second phase, that might be the reason our data was not able to show the association between the improvement of AHI and the change of severity of HOCM before and after PTSMA.
Patients with heart failure and SDB do not tend to complain of daytime somnolence, possibly related to the high sympathetic tone in heart failure. The present study demonstrated a high prevalence of SDB, and almost none of the patients complained of daytime sleepiness (data not shown). Thus, screening questionnaires that include questions about daytime sleepiness (such as the Epworth Sleepiness Scale which is used to screen for obstructive sleep apnea in non-heart failure populations) are not useful [20]. Therefore, thorough screening for SDB in HCM should be performed during treatment for heart failure.
In the present study, a decrease in the AHI following PTSMA was observed, and this was due to a decrease in the hypopnea. Optimizing the treatment for heart failure improves hemodynamics and reduces peripheral edema, presumably minimizing rostral fluid shift and pharyngeal edema. However, how the optimization of heart failure therapy impacts the AHI is not well understood [10]. Angiotensin-converting enzyme inhibitors or beta-blockers have been widely recognized as standard therapy for heart failure, and each drug is effective in reducing the severity of SDB [21,22,23]. In drug-refractory HOCM patients, septal reduction therapy is the only available method to relieve heart failure-associated symptoms, which means that the invasive therapy optimizes the treatment for heart failure and the present study demonstrates that PTSMA is also effective in reducing the severity of SDB.
Study limitations
The study population was of limited size, as drug-refractory HOCM patients are relatively few. In addition, the study used a cross-sectional, observational design, which is subject to the attendant limitations. Nevertheless, the present study represents a single-center experience with a well-defined cohort of patients with drug-refractory HOCM who underwent uniform evaluation. As median duration from PTSMA to the second cardiorespiratory polygraphy was 7 days, the present study showed only the acute effects of PTSMA on SDB. Therefore, whether the beneficial effect of PTSMA on SDB remains for a long time is still unknown.
Conclusions
To the best of our knowledge, this is the first demonstration of the effectiveness of PTSMA in decreasing the AHI. PTSMA is effective in ameliorating the severity of SDB in addition to improving heart failure status.
References
Young T, Finn L, Peppard PE, Szklo-Coxe M, Austin D, Nieto FJ, Stubbs R, Hla KM (2008) Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 31:1071–1078
Jilek C, Krenn M, Sebah D, Obermeier R, Braune A, Kehl V, Schroll S, Montalvan S, Riegger GA, Pfeifer M, Arzt M (2011) Prognostic impact of sleep disordered breathing and its treatment in heart failure: an observational study. Eur J Heart Fail 13:68–75
Eleid MF, Konecny T, Orban M, Sengupta PP, Somers VK, Parish JM, Mookadam F, Brady PA, Sullivan BL, Khandheria BK, Ommen SR, Tajik AJ (2009) High prevalence of abnormal nocturnal oximetry in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 54:1805–1809
Nerbass FB, Pedrosa RP, Danzi-Soares NJ, Drager LF, Arteaga-Fernandez E, Lorenzi-Filho G (2013) Obstructive sleep apnea and hypertrophic cardiomyopathy: a common and potential harmful combination. Sleep Med Rev 17:201–206
Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, Hagege AA, Lafont A, Limongelli G, Mahrholdt H, McKenna WJ, Mogensen J, Nihoyannopoulos P, Nistri S, Pieper PG, Pieske B, Rapezzi C, Rutten FH, Tillmanns C, Watkins H (2014) 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J 35:2733–2779
Seggewiss H, Rigopoulos A, Welge D, Ziemssen P, Faber L (2007) Long-term follow-up after percutaneous septal ablation in hypertrophic obstructive cardiomyopathy. Clin Res Cardiol 96:856–863
Maekawa Y, Akita K, Tsuruta H, Yamada Y, Hayashida K, Yuasa S, Murata M, Jinzaki M, Fukuda K (2016) Significant reduction of left atrial volume concomitant with clinical improvement after percutaneous transluminal septal myocardial ablation for drug-refractory hypertrophic obstructive cardiomyopathy, and its precise detection with multidetector CT. Open Heart 3:e000359
Maekawa Y, Jinzaki M, Tsuruta H, Yamada Y, Kishino Y, Kawakami T, Hayashida K, Yuasa S, Murata M, Kawamura A, Sano M, Kuribayashi S, Fukuda K (2014) Multidetector computed tomography-guided percutaneous transluminal septal myocardial ablation in a Noonan syndrome patient with hypertrophic obstructive cardiomyopathy. Int J Cardiol 172:e79–e81
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM, American Academy of Sleep Medicine (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8:597–619
Pearse SG, Cowie MR (2016) Sleep-disordered breathing in heart failure. Eur J Heart Fail 18:353–361
Maekawa Y, Jinzaki M, Anzai A, Matsumura K, Tsuruta H, Kawakami T, Hayashida K, Yuasa S, Murata M, Suzuki M, Kuribayashi S, Fukuda K (2014) Utility of the reverse wire technique in multidetector computed tomography-guided percutaneous transluminal septal myocardial ablation. Int J Cardiol 173:e33–e34
Spaak J, Egri ZJ, Kubo T, Yu E, Ando S, Kaneko Y, Usui K, Bradley TD, Floras JS (2005) Muscle sympathetic nerve activity during wakefulness in heart failure patients with and without sleep apnea. Hypertension 46:1327–1332
Dimsdale JE, Coy T, Ziegler MG, Ancoli-Israel S, Clausen J (1995) The effect of sleep apnea on plasma and urinary catecholamines. Sleep 18:377–381
Kaitani K, Kondo H, Hanazawa K, Onishi N, Hayama Y, Tsujimura A, Kuroda M, Nishimura S, Yoshikawa Y, Takahashi Y, Amano M, Imamura S, Tamaki Y, Enomoto S, Miyake M, Tamura T, Motooka M, Izumi C, Nakagawa Y (2016) Relationship between diastolic ventricular dysfunction and subclinical sleep-disordered breathing in atrial fibrillation ablation candidates. Heart Vessels 31:1140–1147
Miyata M, Yoshihisa A, Yamauchi H, Owada T, Sato T, Suzuki S, Sugimoto K, Yamaki T, Kunii H, Nakazato K, Suzuki H, Saitoh S, Takeishi Y (2015) Impact of sleep-disordered breathing on myocardial damage and metabolism in patients with chronic heart failure. Heart Vessels 30:318–324
Sinha AM, Skobel EC, Breithardt OA, Norra C, Markus KU, Breuer C, Hanrath P, Stellbrink C (2004) Cardiac resynchronization therapy improves central sleep apnea and Cheyne–Stokes respiration in patients with chronic heart failure. J Am Coll Cardiol 44:68–71
Naruse Y, Tada H, Satoh M, Yanagihara M, Tsuneoka H, Hirata Y, Machino T, Yamasaki H, Igarashi M, Kuroki K, Ito Y, Sekiguchi Y, Aonuma K (2012) Radiofrequency catheter ablation of persistent atrial fibrillation decreases a sleep-disordered breathing parameter during a short follow-up period. Circ J 76:2096–2103
Guttmann OP, Rahman MS, O’Mahony C, Anastasakis A, Elliott PM (2014) Atrial fibrillation and thromboembolism in patients with hypertrophic cardiomyopathy: systematic review. Heart 100:465–472
Rigopoulos AG, Seggewiss H (2011) A decade of percutaneous septal ablation in hypertrophic cardiomyopathy. Circ J 75:28–37
Taranto Montemurro L, Floras JS, Millar PJ, Kasai T, Gabriel JM, Spaak J, Coelho FM, Bradley TD (2012) Inverse relationship of subjective daytime sleepiness to sympathetic activity in patients with heart failure and obstructive sleep apnea. Chest 142:1222–1228
Tamura A, Kawano Y, Naono S, Kotoku M, Kadota J (2007) Relationship between beta-blocker treatment and the severity of central sleep apnea in chronic heart failure. Chest 131:130–135
Tamura A, Kawano Y, Kadota J (2009) Carvedilol reduces the severity of central sleep apnea in chronic heart failure. Circ J 73:295–298
Walsh JT, Andrews R, Starling R, Cowley AJ, Johnston ID, Kinnear WJ (1995) Effects of captopril and oxygen on sleep apnoea in patients with mild to moderate congestive cardiac failure. Br Heart J 73:237–241
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
The authors have no conflicts of interest to report.
Rights and permissions
About this article
Cite this article
Akita, K., Maekawa, Y., Kohno, T. et al. Ameliorating the severity of sleep-disordered breathing concomitant with heart failure status after percutaneous transluminal septal myocardial ablation for drug-refractory hypertrophic obstructive cardiomyopathy. Heart Vessels 32, 1320–1326 (2017). https://doi.org/10.1007/s00380-017-0997-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-017-0997-0