Abstract
Purpose
This study tested the hypothesis that a reduction of pulmonary congestion achieved by a reduction of mitral regurgitation (MR) severity in heart failure (HF) patients is associated with reduced event lengths of sleep-disordered breathing (SDB).
Methods
We prospectively enrolled 20 consecutive HF patients who underwent MitraClip implantation. Patients underwent cardiorespiratory polygraphic recording prior to and after percutaneous mitral valve repair (PMVR). Beyond routinely established indicators of apneas and hypopneas per hour (respiratory event index), we manually analyzed apnea event lengths.
Results
MitraClip implantation led to marked reduction of MR severity and a reduction in left atrial pressure. These hemodynamic changes were accompanied by changes in SDB: the subtype of SDB switched from CSA to OSA in 4 patients. Likewise, quantitative indicators of SDB were altered in both forms of SDB with a reduction in circulatory delay (CSA 38 ± 14 vs. 33 ± 15 s.; p = 0.002 and OSA 34 ± 9 vs. 28 ± 6 s.; p = 0.02) and a corresponding reduction in ventilation lengths in CSA patients (42 ± 15 vs. 37 ± 13 s.; p = 0.05).
Conclusion
A reduction of pulmonary congestion as achieved by a decrease of left atrial pressure through successful MitraClip implantation is associated with a reduction in respiratory event lengths, further pointing towards a relation between SDB and HF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sleep-disordered breathing (SDB) that comprises central sleep apnea (CSA) and obstructive sleep apnea (OSA) is a common comorbidity in heart failure (HF) [1, 2]. Observational studies suggested a link between CSA and surrogate markers of HF severity and several smaller studies suggested favorable effects of CSA treatment on surrogate markers of HF severity [3,4,5,6,7]. In fact for CSA, a close link has been shown between severity of CSA and pulmonary congestion (as a direct consequence of backward failure) due to HF [8]. This is particularly evident when respiratory event lengths are measured quantitatively instead of the traditionally applied number of apneas and hypopneas per hour [8]. A prolonged circulation time (circulatory delay) may directly modify respiratory feedback mechanisms (as a key element in the pathophysiology of CSA) and cause an increase in the duration of CSA with longer cycle lengths, ventilation lengths, apnea lengths and time to peak ventilation [8]. Untreated OSA represents an independent risk factor for the occurrence of malignant arrhythmias and increased cardiac mortality [9]. More recently, a correlation between cycle lengths and signs of HF was also suggested to be involved in OSA [6].
Therefore, the aim of the current study was (1) to unmask potential correlations between signs of HF and respiratory event lengths in both OSA and CSA and (2) to show that reductions in filling pressures as achieved by successful percutaneous mitral valve repair (PMVR) in HF patients with symptomatic mitral regurgitation (MR) lead to reductions in respiratory event lengths with a particular focus on circulatory delay as this has been shown to be uniquely interrelated to cardiac function [6, 8].
Methods
Study population
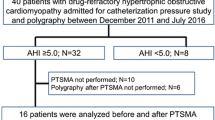
We prospectively included 23 consecutive patients with clinically relevant MR who underwent PMVR with the MitraClip system between December 2016 and June 2017. Three patients did not complete the examinations (with the reason being intolerance of the polygraphic recording system) and were excluded. Thus, our final patient group consisted of 20 patients who underwent PMVR completing all examinations. All patients were classified inoperable or at high-risk for surgery by our interdisciplinary heart team and gave written informed consent for data acquisition and analysis. The study was approved by the local Ethics Committee of the University of Düsseldorf and carried out in accordance with the Declaration of Helsinki. All data were included in a registry, which is registered at www.clinicaltrials.gov (NCT02033811).
Study protocol
Patients underwent cardiorespiratory polygraphic recording (PG) within 5 days prior to and after MitraClip implantation. All patients were supposed to show at least mild sleep apnea (respiratory event index (REI) > 5 events/h) on the initial PG. A comprehensive echocardiographic examination was performed prior to and after MitraClip implantation. Hemodynamic measures were retrieved from right heart catheterization prior MitraClip implantation and from the procedure itself. Therein, the interventionists (R.W. and P.H.) carried out left atrial (LA) pressure measurements prior to and after MitraClip implantation whenever technically feasible.
Echocardiographic measurements
Echocardiographic examinations were performed using a GE Vivid S6/E9, or a Philips iE33. All echocardiographic data were obtained in digital format and then stored on a workstation for offline analysis (Xcelera Cardiology Information Management, Philips). Left ventricular volumes and ejection fraction (LVEF) were calculated using the Simpson biplane method. Right ventricular dysfunction was considered present when the tricuspid annular plane systolic excursion (TAPSE) was ≤ 14 mm. Assessment of MR was performed according to current guidelines [7]. MR was graded as mild, moderate or severe according to the guidelines of the European Society of Cardiology (ESC) [7, 10].
Measurement of sleep-disordered breathing patterns
Cardiorespiratory polygraphy recordings were performed as described earlier using a six-channel device (MiniScreen plus, FA Löwenstein medical, Germany) [6]. Nasal airflow, chest and abdominal efforts, finger pulse oximetry (averaging time 4 s; sampling frequency 3 Hz), ECG, snoring, and body position were recorded continuously. The transient loss of one channel, except nasal airflow, was deemed acceptable. Recordings were analyzed and reviewed by two sleep specialists (J.S. and S.K.) who were adequately trained within the Institute for Sleep Medicine and Neuromuscular Disorders at the University Hospital of Muenster by an attending in sleep medicine (M.B.). Respiratory event scoring followed the guidelines of the American Academy of Sleep Medicine (AASM) [11,12,13]. Apnea was defined as a reduction in nasal airflow by > 90% of baseline for > 90% of the event’s duration and > 10 s. Apneas were classified as obstructive if there was a continued or increased inspiratory effort throughout the entire period of absent airflow. If this was not the case apneas were classified as central. Hypopnea was defined as 30% fall from baseline in airflow signal for 90% of the event’s duration of at least 10 s and 3% desaturation from pre-event baseline. Patients were classified as having OSA if > 50% of all apneas were obstructive in origin, while they were classified as having CSA if > 50% of all apneas were central. Cycle lengths were measured as previously described by our group [8]. In short, cycle length was defined as the time from the beginning of an apnea to the end of the following ventilation; therefore, cycle lengths represent the sum of apnea length and the following ventilation lengths. Time from resumption of airflow to the following peak in airflow was defined as TTPV. Circulatory delay was the time from the first breath after apnea to the following nadir of oxygen saturation. Data on respiratory event lengths shown represent an average of up to 24 separate (up to 6 apnea events per time window of 2 h from 10 p.m. to 6 a.m.)—manually and carefully selected—apnea measurements obtained throughout the night. In patients classified as having predominantly OSA, obstructive apneas events were measured whereas in CSA patients central apnea events were measured. Figure 1 shows a scheme of central and obstructive apnea respiratory event lengths measurements.
Scheme of obstructive (left) and central (right) respiratory apnea event lengths (a) nasal airflow, (b) peripheral oxygen saturation, (c) chest effort, and (d) abdominal effort in sleep apnea in heart failure patients. CD, circulatory delay; CL, cycle length; AL, apnea length; VL, ventilation length; TTPV, time to peak ventilation
Statistical analysis
All analyses were performed using Sigma Plot software (Version 13.0, Systat Software Ltd). Results are expressed as mean ± standard deviation for continuous variables or percentages for categorical variables unless otherwise specified. Before analysis, normality distribution was tested with Kolmogorov-Smirnov test. The differences between two groups were compared for significance with a two-tailed paired t test. Pearson product moment correlation was used for correlation analysis. A value of p < 0.05 was considered statistically significant.
Results
The demographic and clinical data of the cohort are summarized in Table 1. Mean age was 80 ± 6 years. The majority of patients (85%) presented with New York Heart Association (NYHA) functional class III or IV and reduced LVEF (38 ± 9%). Mean NT-proBNP was 4893 (1256–5271) pg/ml. Seven patients (35%) presented with degenerative MR, while 13 patients (65%) had functional MR. MitraClip implantation was associated with a significant reduction in MR severity (80 vs. 10% MR grade 3+; p < 0.001) as well as LA pressure (16 ± 6 vs. 12 ± 5 mmHg; p = 0.006) and systolic pulmonary artery pressure (49 ± 17 vs. 44 ± 9 mmHg; p = 0.04).
Association between sleep-disordered breathing and heart failure at baseline
All patients showed at least mild SDB (apnea-hypopnea index > 5 events/h) on the initial PG with the majority of them (11/20 patients) presenting with predominant OSA (Table 2 and Fig. 2). At baseline, positive correlations were found between respiratory event length and cardiac function in both CSA and OSA patients: In CSA patients, apnea length (r = − 0.08; p = 0.03; Fig. 3a) and ventilation length (r = − 0.08; p = 0.04; Fig. 3b) increased with worsening cardiac index. However, no correlations were found between echocardiographic parameters of HF severity and respiratory event length.
Correlations between apnea lengths and cardiac index (a) and ventilation length and cardiac index in 9 CSA patients (b). Correlations between cycle lengths and left ventricular ejection fraction (c) and cylce length and right ventricular end-diastolic diameter as a sign of right ventricular overload in 11 OSA patients (d). Each data point represents an average of up to 24 separate–manually and carefully selected–apnea measurements obtained throughout the night
In OSA patients, there was no correlation between cardiac index and respiratory event length. Instead, cycle length increased with reduced LVEF (r = − 0.6; p = 0.04; Fig. 3c). Furthermore, cycle length increased with signs of right ventricular overload (increased right ventricular end-diastolic diameter (RVEDD)) (r = 0.7; p = 0.03; Fig. 3d). In addition, ventilation length increased with worsening LVEF (r = − 0.6; p = 0.05).
In contrast to these findings, no correlations between cardiac function and severity of OSA or CSA were found when traditionally used markers of SDB severity (event counts/h) were applied. Moreover, we did not detect a direct association between parameters of MR severity and SDB.
Changes in sleep-disordered breathing after MitraClip implantation
Echocardiographic, hemodynamic and respiratory changes associated with MitraClip implantation are summarized in Table 2. Successful reduction in MR was associated with a change in the subtype of SDB with fewer patients presenting with predominantly CSA after PMVR (Table 2 and Fig. 2). Again, no significant changes in severity of SDB were found when standard metrics of SDB severity, as defined by event counts per hour, were analyzed. However, when we conducted in-depth quantitative analysis of apnea event lengths, we deciphered alterations in circulatory delay in both, central apneas (38 ± 14 vs. 33 ± 15 s.; p = 0.002; Fig. 4a) and obstructive apneas (34 ± 9 vs. 28 ± 6 s.; p = 0.02; Fig. 4b) following PMVR. In patients with central apneas, ventilation length was also shorter after MitraClip implantation (42 ± 15 vs. 37 ± 13 s.; p = 0.05).
Differences in circulatory delay between pre and post MitraClip implantation in patients with predominantly OSA (a) (n = 11) and patients with predominantly CSA (b) at baseline (n = 9). Each data point represents an average of up to 24 separate–manually and carefully selected–apnea measurements obtained throughout the night
Discussion
In the present study, we evaluated the association between HF severity and SDB and the effect of PMVR on SDB in patients with clinically relevant MR undergoing PMVR with the MitraClip. We demonstrate that in HF patients with symptomatic MR, both obstructive and central respiratory event lengths are related to hemodynamic and echocardiographic parameters of right- and left ventricular function (in contrast to respiratory events/h). Furthermore, we show that a reduction of filling pressures achieved by a reduction in MR severity through PMVR is associated with a reduction of respiratory event lengths, further underscoring the interrelation between SDB and HF.
Association between sleep-disordered breathing and heart failure at baseline
The phenomenon of a correlation between HF severity and respiratory event lengths in both OSA and CSA has been studied before. Wedewardt et al. demonstrated an association of central apnea event lengths with left ventricular systolic function which is in line with our findings [8]. In fact, the Academy of Sleep Medicine (AASM) acknowledges the superiority of cycle lengths over REI in reflecting severity of CSA in HF in its current guidelines [12]. Central respiratory event lengths lengthen along with deteriorating left ventricular systolic function [12]. The pathophysiology of CSA in HF is complex and still incompletely understood. Pulmonary congestion is thought to lead to increased central respiratory drive entering into a vicious circle of hyperventilation with subsequent central apneas in response to small increases in carbon dioxide at night [3, 14]. J-receptors sense pulmonary congestion, clinically indicated by increased post-capillary wedge pressure and foster central respiratory drive [3]. Circulatory delay might explain best why respiratory cycle lengths (as opposed to the REI) correlate with HF severity in CSA. As left ventricular function deteriorates, circulatory delay increases leading to a less efficient feedback system of any respiratory changes. Of note, a previous cross-sectional study has shown that there is substantial inter-correlation between circulatory delay and apnea length and ventilation length owing to the fact that a less efficient feedback system with longer circulatory delay may lead to longer overall cycle lengths too [8].
In contrast to CSA, the association of OSA severity with HF severity is less clear [1]. In this regard, Efken et al. and Ryan et al. studied obstructive apnea event lengths in HF and demonstrated a robust correlation between obstructive apnea event lengths and pulmonary congestion with the main reason for this correlation being increased circulatory delay [6, 15]. In this regard, our findings of a correlation between right ventricular overload and circulatory delay along with a correlation between left ventricular function and cycle lengths supports the hypothesis that that a longer circulation time leads to delayed report of gas tensions and this does also contribute to longer cycle lengths in OSA. This would only explain why OSA ventilation lengths correlate with HF severity. In this regard, a correlation with HF severity as invasively measured by pulmonary congestion has only been demonstrated for cycle length and ventilation lengths and not for apnea lengths [6]. This finding is in line with our results and underlines that, in contrast to CSA where both apnea lengths and ventilation lengths were found to correlate with HF severity, in OSA, apnea lengths depend on complex regulatory pathways that determine upper airway stability [8]. Despite the fluid shift theory that strengthens the thesis that HF severity directly contributes to upper airway instability and hence prolonged apnea lengths, even in OSA this theory alone does not explain apnea lengths in OSA [16].
Changes in sleep-disordered breathing after MitraClip implantation
Successful MitraClip implantation led to a reduction of MR severity as shown by echocardiography and invasive measurement of LA pressure as well as a reduction of systolic pulmonary artery pressure. Figure 5 displays a representative case of a patient’s finding on PG recording and invasive hemodynamics as well as echocardiographic severity of MR before and after successful PMVR. The fact that MitraClip implantation was associated with a change in the subtype of SDB in 4 patients from CSA to OSA is in line with previous reports, showing that improvements in cardiac function can lead to lesser CSA, thereby unmasking pre-existing OSA. This was shown by Fox et al. in patients with improved cardiac function following successful cardioversion of atrial fibrillation and atrial flutter [17]. Likewise, resolution from CSA was demonstrated in patients following implantation of left ventricular assist device, cardiac transplantation, successful diuretic therapy for acute decompensated HF, and more recently, after treatment of HF with sacubitril/valsartan [18,19,20,21]. This was also demonstrated after valvuloplasty in patients with mitral stenosis albeit with the limitation that respiratory event lengths were not quantified [22, 23]. Our finding of a significant change in both cycle lengths and circulatory delay and not apnea lengths in central respiratory event lengths following reduction in MR severity along with a decrease in LA pressure (indicating pulmonary decongestion) is of importance: First, it provides further evidence that in CSA, ventilation lengths and hence central respiratory drive is influenced by the degree of pulmonary congestion (LA pressure) with shorter ventilation lengths as pulmonary congestion decreases due to a reduction of MR. Second, we demonstrate that this holds true for ventilation lengths but not for apnea lengths. In this regard, apnea lengths were found to be relatively consistent at approximately 20 s in previous cross-sectional studies of CSA cycle lengths in HF and to be less dependent from HF severity than ventilation lengths, which is in line with our results [24]. The significant change in circulatory delay in CSA event lengths with shorter circulatory delays following PMVR is likely to be the direct consequence of reduced MR, lower LA pressure and consecutively improved cardiac function with faster response to changes in gas tensions. This might also be one of the mechanisms behind the significantly shorter ventilation lengths following PMVR. Faster response to any changes in gas tensions through improved cardiac function with shorter circulatory delay through less MR could explain shorter ventilation lengths in CSA patients after MitraClip implantation. In patients with predominately OSA, we detected shorter circulatory delays without any significant changes in ventilation lengths or apnea lengths following MitraClip implantation. This could be caused by an improved cardiac function after PMVR leading to shorter circulatory delays also in obstructive events. However, ventilation lengths and apnea lengths might not be solely influenced by cardiac function as they depend on complex regulatory pathways that determine upper airway stability and that also include fluid shift from the legs to the neck at night [16]. In this regard, we strengthen the findings of Efken et al. by demonstrating that the correlations were also found in longitudinal design and not only in cross-sectional studies [6].
Representative data of a patient with severe MR, increased left atrial pressure (LAP) and long CSA cycle lengths before PMVR with the MitraClip system (right) and only mild MR, lower LA pressure and shorter CSA cycle lengths after successful MitraClip implantation (left). From top to down polygraphic data show the following signals: (a) nasal airflow, (b) peripheral oxygen saturation, (c) chest effort, and (d) abdominal effort. CD, circulatory delay; CL, cycle length; AL, apnea length; VL, ventilation length; TTPV, time to peak ventilation; LAP, left atrial pressure; PMVR, percutaneous mitral valve repair
Limitations
There are several limitations of this study. We applied multi-channel cardiorespiratory polygraphy recordings instead of polysomnography. Therefore, data on sleep, sleep quality, and arousals are not available. This implies that total REI could be underestimated because total sleep time might be shorter than total recording time. Despite this, for the purpose of measuring obstructive and central respiratory patterns, high-quality polygraphy recordings provide all the important information required. The small sample size is a further limiting factor. Final inclusion of 20 patients implies that multivariate analysis is impossible; thus, analysis of potential confounding factors is beyond the scope of this manuscript. However, this study is the first to assess cycle lengths in OSA in patients with symptomatic MR along the course of successful treatment by PMVR.
Conclusion
In HF patients with symptomatic MR, both obstructive and central respiratory event lengths (in contrast to respiratory events counts per hour) are related to left ventricular function. A reduction of pulmonary congestion as indicated by a reduction in LA pressure following successful PMVR is associated with a reduction in respiratory event lengths, further pointing towards a relation between SDB and HF.
Abbreviations
- REI:
-
Respiratory event index
- AL:
-
Apnea length
- CD:
-
Circulatory delay
- CL:
-
Cycle length
- CSA:
-
Central sleep apnea
- CSR:
-
Cheyne-Stokes respiration
- EROA:
-
Effective regurgitant orifice area
- HF:
-
Heart failure
- LVEF:
-
Left ventricular ejection fraction
- MR:
-
Mitral regurgitation
- NYHA:
-
New York Heart Association
- OSA:
-
Obstructive sleep apnea
- PISA:
-
Proximal isovelocity surface area
- PG:
-
Polygraphic recording
- PMVR:
-
Percutaneous mitral valve repair
- RV:
-
Regurgitation volume
- SDB:
-
Sleep-disordered breathing
- RVEDD:
-
Right ventricular end-diastolic diameter
- TTPV:
-
Time-to-peak-ventilation
- VL:
-
Ventilation length
References
Kasai T, Floras JS, Bradley TD (2012) Sleep apnea and cardiovascular disease: a bidirectional relationship. Circulation 126:1495–1510. https://doi.org/10.1161/CIRCULATIONAHA.111.070813
Oldenburg O, Lamp B, Faber L, Teschler H, Horstkotte D, Töpfer V (2007) Sleep-disordered breathing in patients with symptomatic heart failure. A contemporary study of prevalence in and characteristics of 700 patients. Eur J Heart Fail 9:251–257. https://doi.org/10.1016/j.ejheart.2006.08.003
Bradley TD, Floras JS (2003) Sleep apnea and heart failure—part II: central sleep apnea. Circulation 107:1822–1826. https://doi.org/10.1161/01.CIR.0000061758.05044.64
Harada D, Joho S, Oda Y, Hirai T, Asanoi H, Inoue H (2011) Autonomic neuroscience : basic and clinical short term effect of adaptive servo-ventilation on muscle sympathetic nerve activity in patients with heart failure. Auton Neurosci Basic Clin 161:95–102. https://doi.org/10.1016/j.autneu.2010.12.001
Cowie MR, Woehrle H, Wegscheider K, Angermann C, d'Ortho MP, Erdmann E, Levy P, Simonds A, Somers VK, Zannad F, Teschler H (2013) Rationale and design of the SERVE-HF study: treatment of sleep-disordered breathing with predominant central sleep apnoea with adaptive servo-ventilation in patients with chronic heart failure. Eur J Heart Fail 15:937–943. https://doi.org/10.1093/eurjhf/hft051
Efken C, Bitter T, Prib N, Horstkotte D, Oldenburg O (2013) Obstructive sleep apnoea: longer respiratory event lengths in patients with heart failure. Eur Respir J 41:1340–1346. https://doi.org/10.1183/09031936.00082212
Baumgartner H, Falk V, Bax JJ, de Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Muñoz D, Rosenhek R, Sjögren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL, ESC Scientific Document Group, Roffi M, Alfieri O, Agewall S, Ahlsson A, Barbato E, Bueno H, Collet JP, Coman IM, Czerny M, Delgado V, Fitzsimons D, Folliguet T, Gaemperli O, Habib G, Harringer W, Haude M, Hindricks G, Katus HA, Knuuti J, Kolh P, Leclercq C, McDonagh TA, Piepoli MF, Pierard LA, Ponikowski P, Rosano GMC, Ruschitzka F, Shlyakhto E, Simpson IA, Sousa-Uva M, Stepinska J, Tarantini G, Tchétché D, Aboyans V, Windecker S, Aboyans V, Agewall S, Barbato E, Bueno H, Coca A, Collet JP, Coman IM, Dean V, Delgado V, Fitzsimons D, Gaemperli O, Hindricks G, Iung B, Jüni P, Katus HA, Knuuti J, Lancellotti P, Leclercq C, McDonagh T, Piepoli MF, Ponikowski P, Richter DJ, Roffi M, Shlyakhto E, Simpson IA, Zamorano JL, Kzhdryan HK, Mascherbauer J, Samadov F, Shumavets V, Camp GV, Lončar D, Lovric D, Georgiou GM, Linhartova K, Ihlemann N, Abdelhamid M, Pern T, Turpeinen A, Srbinovska-Kostovska E, Cohen A, Bakhutashvili Z, Ince H, Vavuranakis M, Temesvári A, Gudnason T, Mylotte D, Kuperstein R, Indolfi C, Pya Y, Bajraktari G, Kerimkulova A, Rudzitis A, Mizariene V, Lebrun F, Demarco DC, Oukerraj L, Bouma BJ, Steigen TK, Komar M, de Moura Branco LM, Popescu BA, Uspenskiy V, Foscoli M, Jovovic L, Simkova I, Bunc M, de Prada JAV, Stagmo M, Kaufmann BA, Mahdhaoui A, Bozkurt E, Nesukay E, Brecker SJD (2017) 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J 38:2739–2786. https://doi.org/10.1093/eurheartj/ehx391
Wedewardt J, Bitter T, Prinz C, Faber L, Horstkotte D, Oldenburg O (2010) Cheyne-Stokes respiration in heart failure: cycle length is dependent on left ventricular ejection fraction. Sleep Med 11:137–142. https://doi.org/10.1016/j.sleep.2009.09.004
Bradley TD, Floras JS (2009) Obstructive sleep apnoea and its cardiovascular consequences. Lancet 373:82–93. https://doi.org/10.1016/S0140-6736(08)61622-0
Lang RM, Badano LP, Mor-avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults : an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1–39.e14. https://doi.org/10.1016/j.echo.2014.10.003
Berry RB, Brooks R, Gamaldo CE et al (2013) The AASM manual for the scoring of sleep and associated events. Am Acad Sleep Med 53:1689–1699. https://doi.org/10.1017/CBO9781107415324.004
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Ward SLD, Tangredi MM (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. J Clin Sleep Med. https://doi.org/10.5664/jcsm.2172
Collop NA, Tracy SL, Kapur V, Mehra R, Kuhlmann D, Fleishman SA, Ojile JM (2011) Obstructive sleep apnea devices for out-of-center (OOC) testing: technology evaluation. J Clin Sleep Med 7(5):531–548
Muza RT (2015) Central sleep apnoea—a clinical review. J Thorac Dis 7:930–937. https://doi.org/10.3978/j.issn.2072-1439.2015.04.45
Ryan CM, Bradley TD (2005) Periodicity of obstructive sleep apnea in patients with and without heart failure. Chest 127(2):536–542
Kasai T, Motwani SS, Yumino D, Mak S, Newton GE, Bradley TD (2012) Differing relationship of nocturnal fluid shifts to sleep apnea in men and women with heart failure. Circ Hear Fail 5:467–474. https://doi.org/10.1161/CIRCHEARTFAILURE.111.965814
Fox H, Bitter T, Horstkotte D, Oldenburg O (2016) Cardioversion of atrial fibrillation or atrial flutter into sinus rhythm reduces nocturnal central respiratory events and unmasks obstructive sleep apnoea. Clin Res Cardiol 105:451–459. https://doi.org/10.1007/s00392-015-0940-2
Bitter T, Horstkotte D, Basic K et al (2016) Improvements of central respiratory events , Cheyne e Stokes respiration and oxygenation in patients hospitalized for acute decompensated heart failure. Sleep Med 28:15–19. https://doi.org/10.1016/j.sleep.2016.10.006
Vazir A, Hastings PC, Morrell MJ, Pepper J, Henein MY, Westaby S, Poole-Wilson PA, Cowie MR, Simonds AK (2010) Resolution of central sleep apnoea following implantation of a left ventricular assist device. Int J Cardiol 138:317–319. https://doi.org/10.1016/j.ijcard.2008.06.072
Fox H, Bitter T, Horstkotte D, Oldenburg O (2017) Resolution of cheyne-stokes respiration after treatment of heart failure with sacubitril/valsartan: a first case report. Cardiol 137:96–99. https://doi.org/10.1159/000455118
Fox H, Puehler T, Schulz U, Bitter T, Horstkotte D, Oldenburg O (2014) Delayed recovery from Cheyne-Stokes respiration in heart failure after successful cardiac transplantation: a case report. Transplant Proc 46:2462–2463. https://doi.org/10.1016/j.transproceed.2014.06.063
Takahashi M, Kasai T, Dohi T, Maeno KI, Kasagi S, Kawana F, Ishiwata S, Narui K (2011) Conversion from predominant central sleep apnea to obstructive sleep apnea following valvuloplasty in a patient with mitral regurgitation. J Clin Sleep Med 7:523–525. https://doi.org/10.5664/JCSM.1324
Yasuma F, Hayashi H, Noda S et al (1995) A case of mitral regurgitation whose nocturnal periodic breathing was improved after mitral valve replacement. Jpn Heart J 36:267–272
Lorenzi-Filho G, Dajani HR, Leung RS, Floras JS, Bradley TD (1999) Entrainment of blood pressure and heart rate oscillations by periodic breathing. Am J Respir Crit Care Med 159(4 Pt 1):1147–1154
Acknowledgements
We gratefully acknowledge Miss Cettolines’ technical help in collecting our data and Mister Perez’ help in analyzing the sleep studies.
Funding
JS has been supported by the ‘Else-Kröner-Fresenius Stiftung’ (Grant A109) and by ‘Kommission für Innovative Medizinische Forschung an der Medizinischen Fakultät Muenster’ (IMF Grant SP 11 18 15) outside this work. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. This does not alter our adherence to Journal policies on sharing data and materials.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JS has been supported by the ‘Else-Kröner-Fresenius Stiftung’ (Grant A109) and by ‘Kommission für Innovative Medizinische Forschung an der Medizinischen Fakultät Muenster’ (IMF Grant SP 11 18 15) outside this work.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the local Ethics Committee of the University of Düsseldorf.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Spiesshoefer, J., Spieker, M., Klose, S. et al. Reduction of sleep-disordered breathing following effective percutaneous mitral valve repair with the MitraClip system. Sleep Breath 23, 815–824 (2019). https://doi.org/10.1007/s11325-018-1764-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-018-1764-x