Abstract
Sleep-disordered breathing (SDB) has a critical association with mortality and morbidity of patients with chronic heart failure (CHF). Troponin T is a marker of ongoing myocardial damage and predicts adverse clinical outcomes in patients with CHF. Carnitine plays an important role in the utilization of fatty acids in the myocardium. It has been reported that myocardial carnitine levels decrease in the failing heart. We hypothesized that plasma troponin T and carnitine are increased due to the leakage from damaged cardiomyocytes or the alteration of myocardial metabolism in CHF patients with SDB. We examined the relation of plasma troponin T and carnitine levels with severity of SDB in CHF. We used portable sleep monitor and measured the apnea–hypopnea index (AHI), plasma levels of high-sensitive troponin T and carnitine in 131 CHF patients. These patients were divided into three groups based on AHI: group A (None–mild SDB AHI < 15/h, n = 45), group B (Moderate SDB 15 ≤ AHI < 30/h, n = 32) and group C (Severe SDB AHI ≥ 30/h, n = 54). Levels of high-sensitive troponin T and plasm total carnitine were significantly higher in group C than in groups A and B [high-sensitive troponin T; group A 0.009 (0.005–0.016), group B 0.012 (0.006–0.021), group C 0.021 (0.011–0.039) ng/ml, total carnitine; group A 61.0 ± 15.1, group B 65.0 ± 13.5, group C 73.3 ± 17.5 μmol/l, P < 0.01 vs. group A and P < 0.05 vs. group B, respectively]. Furthermore, in the multiple regression analysis, the independent factors to determine plasma levels of log (high-sensitive troponin T) were high-sensitive C-reactive protein and AHI, and the independent factors to determine plasma levels of carnitine were glomerular filtration rate and AHI. The present study suggests that SDB is associated with latent myocardial damage and alteration of myocardial carnitine metabolism in patients with CHF, presented by higher circulating troponin T and carnitine levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic heart failure (CHF) is the major cause of death in elderly in many countries. Sleep-disordered breathing (SDB) mutually accelerates inflammation and sympathetic nervous activity in CHF, and is associated with adverse outcomes in patients with CHF [1–3]. Troponin T is a marker of ongoing myocardial damage and predicts adverse clinical outcomes in patients with CHF [4–7]. Carnitine is an essential cofactor for fatty acid oxidative metabolism, the predominant source of ATP in the normal aerobic heart [8]. Additionally, carnitine is the requisite carrier for the transport of fatty acids from the cytosol across the mitochondrial membrane for beta oxidation [9]. Previous studies have indicated that decreased myocardial free carnitine concentration, and increased plasma acylcarnitine and urinary free carnitine excretion were evident in patients with CHF [10]. These results suggest that myocardial damage and mechanical cardiac overload may affect on myocardial carnitine metabolism in patients with CHF.
However, ongoing myocardial damage and carnitine metabolism in CHF with SDB are not fully understood. Therefore, we sought to clarify the relationship of the severity of SDB with increased myocardial damage and alteration of myocardial carnitine metabolism in patients with CHF. We examined circulating levels of plasma high-sensitive troponin T, free carnitine, and acyl carnitine in CHF with SDB.
Methods
The study subjects consisted of 131 consecutive patients (95 men, mean age 61 ± 14 years) with CHF who were referred for overnight polygraphy at Fukushima Medical University between January 2012 and June 2012. Inclusion criteria were (1) the presence of symptomatic CHF, which was defined as New York Heart Association class > II; (2) prescribed with standard pharmacotherapy (including angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, β blockers, diuretics, etc.); and (3) having a stable clinical status, defined as receiving medical therapy with no worsening of CHF for at least 3 months prior to study enrollment. The exclusion criteria were the presence of receiving hemodialysis and SDB therapy. Patients were divided into three groups based on the apnea–hypopnea index (AHI) value: group A (none-mild SDB 0 ≤ AHI < 15/h, n = 45), group B (moderate SDB 15 ≤ AHI < 30/h, n = 52), and group C (severe SDB AHI ≥ 30/h, n = 34). We compared clinical characteristics, echocardiographic parameters, and laboratory data, including plasma levels of high-sensitive troponin T and carnitine between the three groups. Written informed consent was obtained from all study subjects. The study protocol was approved by the ethics committee of Fukushima Medical University.
All subjects underwent overnight polygraphy with the use of standard techniques, as previously reported in another literature [11]. Overnight polygraphy was performed using a portable sleep monitoring system (LS-300, Fukuda Denshi, Tokyo, Japan) that consisted of the monitoring of the electrocardiogram, thoracoabdominal motion, nasal airflow by an airflow pressure transducer, and arterial oxyhemoglobin saturation (SpO2) by pulse oximetry. Apnea was defined as an absence of airflow for more than 10 s. Hypopnea was defined as a >30% reduction in monitored airflow for ≥10 s accompanied by a decrease in SpO2 > 3%. Obstructive apnea was defined as the absence of airflow for ≥10 s associated with ribcage and abdominal motion. Central apnea was defined as the absence of airflow for >10 s associated without ribcage and abdominal motion. The major polygraphic parameters investigated were AHI, central apnea index (CAI), obstructive apnea index (OAI), lowest pulse oxygen saturation (lowest SpO2), and mean pulse oxygen saturation (mean SpO2).
Blood samples were obtained the next morning after the polygraphy, while the patient was in a supine position under fasting state. We measured the plasma concentrations of high-sensitive troponin T, acyl carnitine, free carnitine, serum creatinine, high-sensitive C-reactive protein (CRP) and plasma B-type natriuretic peptide (BNP). The eGFRs were calculated by the Modification of Diet in Renal Disease formula. The Plasma BNP levels were measured using a specific immunoradiometric assay (Shionoria BNP kit, Shionogi, Osaka, Japan), and the high-sensitive troponin T levels were measured using electrochemiluminescence immunoassay (Elecsys Troponin T hs, Roche Diagnostics Ltd., Rotkreuz, Switzerland). Plasma carnitine profiles (free carnitine, acyl carnitine and total carnitine) were determined by an enzymatic cycling method with carnitine dehydrogenase (Kinos Co., Tokyo, Japan).
Echocardiography was performed using the standard techniques by an experienced echocardiographer at the echo laboratory in our hospital during daytime. Two-dimensional echocardiographic images were acquired from the parasternal long and short axis, and apical four chamber views. The major echocardiographic parameters investigated were left ventricular ejection fraction (LVEF), left ventricular mass index (LVMI), the ratio of left ventricular inflow E wave to A wave peak velocity (E/A), and the ratio of transmitral early left ventricular filling velocity to early diastolic Doppler tissue imaging of the mitral annulus (E/e′). All recordings were performed with ultrasound systems (Philips Medical Systems, Andover, MA, USA).
A Shapiro–Wilk test was used for assessment of the normal distribution. Normally distributed data are presented as mean ± SD, and non-normally distributed data are presented as median (inter-quartile range). Categorical variables are expressed as frequencies and relative frequencies. We used the one-way analysis of variance (ANOVA) followed by Tukey’s post-hoc test. Non-normally distributed data were analyzed by the Kruskal-Wallis test. Correlation between high-sensitive troponin T and total carnitine was assessed using Spearman correlation analysis. Multivariable regression analysis was used to determine plasma levels of high-sensitive troponin T and total carnitine. Because of non-normally distribution of high-sensitive troponin T value, we made log transformation for high-sensitive troponin T. To prepare for potential confounding, we introduced the following factors, known to affect the plasma high-sensitive troponin T and the plasma carnitine levels, and variables which were significantly different among three groups into models: age, gender, body mass index, BNP, eGFR, high-sensitive CRP, LVEF, and AHI. Parameters with statistical significance in the univariable analysis (P < 0.10) were included in the multivariable analysis. A value of P < 0.05 was considered significant for all comparisons. All analyses were performed using a statistical software package (SPSS ver. 21.0, IBM, Armonk, NY, USA).
Results
The clinical characteristics and polygraphic data of the study subjects are shown in Table 1. Age and body mass index were significantly higher in group C than in groups A and B. There were no significant differences in comorbidity and etiology. AHI, CAI and OAI were significantly higher in group C than in groups A and B. In addition, AHI, CAI and OAI were significantly higher in group B than in group A. The laboratory and echocardiographic data are shown in Table 2. There were no significant differences in BNP, high-sensitive CRP, PaO2 and PaCO2 among the 3 groups. Estimated GFR was significantly lower in group C than in groups A and B. There were no significant differences in any echocardiographic parameters. Moreover, there was a positive correlation between high-sensitive troponin T and total carnitine (R = 0.255, P < 0.05).
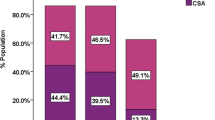
Figure 1 demonstrates comparisons of plasma levels of high-sensitive troponin T. Plasma levels of high-sensitive troponin T were significantly higher in group C than in groups A and B. Figure 2a–c demonstrates comparisons of plasma levels of free carnitine, acylcarnitine and total carnitine among 3 groups, respectively. Plasma levels of free and acyl carnitine were significantly higher in group C than in group A. Moreover, plasma levels of total carnitine were significantly higher in group C than in groups A and B.
In the multiple regression analysis (Tables 3 and 4), the independent factors to determine the plasma levels of log (high-sensitive troponin T) were high-sensitive CRP and AHI. In addition, the independent factors to determine the plasma levels of carnitine were eGFR and AHI.
From the receiver operating characteristic curve (ROC) analysis, high-sensitive troponin T (a cut-off value of 0.011 ng/ml) identified severe SDB with sensitivity 78 %, specificity 51 %, and area under the curve 0.72. Similarly, total carnitine (a cut-off value of 62.9 μmol/l) identified severe SDB with sensitivity 67%, specificity 52 %, and area under the curve 0.65.
Discussion
In this study, plasma high-sensitive troponin T and total carnitine levels were significantly higher in CHF patients with severe SDB than in CHF without severe SDB. Furthermore, AHI is an independent factor to determine plasma levels of high-sensitive troponin T and carnitine. To the best of our knowledge, this is the first study to show the relationship of the severity of SDB in patients with CHF and increased ongoing myocardial damage and impact on myocardial carnitine metabolism.
Persistent release of myocardial troponins might reflect ongoing cardiac myocyte cell death. In the case of very low troponin levels, cardiac damage is assumed to be independent of an ischemic origin of the myocardium. The mechanism possibly responsible for releasing myocardial troponin is considered to be stretch of cardio myocytes and transient loss of cell membrane integrity. This reversible damage may contribute to the increase of circulating troponin T caused by irreversible injury of cardiomyocytes [4–7]. Several factors, including ischemic myocardial damage, activation of sympathetic nerve function, inflammatory processes, and autophagic degeneration, have been implicated in myocyte injury and death. All these pathways converge on myocardial damage and death by progressive necrosis or apoptosis. It has been reported that patients with ongoing myocardial damage showed higher reaction of CRP than those without ongoing myocardial damage, and there were significant correlations between the serum levels of troponin T and monocyte proinflammatory cytokine, such as tumor necrosis factor-alpha and interleukin 6 [12]. Indeed, elevated troponin T levels have been found to predict adverse outcomes in patients with CHF [4–7]. Recently, it has been reported that severity of SDB is associated with increased CRP [13] and troponin T [14] levels in patients without cardiovascular disease.
Long-chain fatty acids constitute a basic substrate for oxidative energy metabolism in the myocardium. The primary function of carnitine is to permit the entry of esterified fatty acids (the source of ATP synthesis) into the mitochondrial matrix, where β oxidation occurs. The intracellular homeostasis of carnitine is controlled by different membrane transporters—the organic cation transporters (OCTNs), which operate on the intestinal absorption and renal reabsorption of carnitine, and play a major role in tissue distribution and variations in transport rates [15]. The downregulated left ventricular OCTN2 expression may be associated with decreased left ventricular free carnitine levels [16]. Recent experimental studies have demonstrated that carnitine protects the myocardium against ischemic injury, angina, diastolic dysfunction and heart failure [15, 17, 18]. It has been reported that plasma concentrations of carnitine are (1) increased in patients with cardiomyopathy, [19] (2) have negative correlations with LVEF, [19] and (3) associated with increase of urinary carnitine excretion [20]. Furthermore, levels of plasma carnitine are thought to be affected by dietary intake, renal reabsorption and liver synthesis [21].
SDB accelerates inflammation, sympathetic nervous activity, the renin angiotensin aldosterone system [22], intermittent hypoxia [23], transient hypertension [24], and glomerular over-filtration [25], and causes renal dysfunction [26], left ventricular hypertrophy [27], as well as cardiac biventricular systolic and diastolic dysfunction. These mechanisms may cause ongoing myocardial damage expressed by troponin T. Furthermore, focusing on carnitine, the OCTN2 expression was strongly reduced in the myocardium with significant inflammation (52 % compared with no inflammation), whereas the expression in the presence of a minor inflammation was unaltered compared to the myocardium with no inflammation [28]. Inflammation and subsequent myocardial damage may increase the levels of plasma carnitine. Recently, plasma acylcarnitine has been proposed to be a biomarker of insulin resistance and metabolic inflexibility in adults [29, 30]. The severity of SDB (as measured by AHI) was reportedly associated with insulin resistance. These findings, therefore, support our hypothesis that SDB may increase the risk for cardio-metabolic disease [31]. It has been reported that the leakage from damaged cardiomyocytes or deficient carnitine transport into cells may influence on increasing levels of plasma carnitine [21]. The mechanism behind higher carnitine levels in CHF patients with severe SDB still remains unclear; however, it may be due to increased cardiomyocyte damage and decreased carnitine transport into cardiac cells, or other reasons.
In the present study, we demonstrated that latent low-grade myocardial damage and altered carnitine metabolism were present among severe SDB patients in CHF, and these data may provide us novel mechanistic and therapeutic insights to understand the clinical impacts of SDB on CHF patients. Thus, cardiomyocyte protective approach by treatment of SDB has clinically important implications to improve prognosis of patients with CHF.
Study limitations
In our study, there were some study limitations. First, the gold standard for the diagnostic test of SDB is a full-channel polysomnography, which provides detailed information on the complete differentiation of the types of apnea [32]. In this study, our differentiation of SDB by portable sleep monitor might be less reliable than that by full polysomnography. Second, the number of study subjects was small, since this study was performed in a single institution. Hence, further investigation by full polysomnography may lead to the entire clarification of the mechanisms of myocardial damage and myocardial metabolism in CHF patients with SDB.
Conclusions
In conclusion, the present study suggests that SDB is associated with myocardial damage and alteration of myocardial carnitine metabolism in CHF patients.
References
Javaheri S, Shukla R, Zeigler H, Wexler L (2007) Central sleep apnea, right ventricular dysfunction, and low diastolic blood pressure are predictors of mortality in systolic heart failure. J Am Coll Cardiol 49:2028–2034
Wang H, Parker JD, Newton GE, Floras JS, Mak S, Chiu KL, Ruttanaumpawan P, Tomlinson G, Bradley TD (2007) Influence of obstructive sleep apnea on mortality in patients with heart failure. J Am Coll Cardiol 49:1625–1631
Bitter T, Westerheide N, Prinz C, Hossain MS, Vogt J, Langer C, Horstkotte D, Oldenburg O (2011) Cheyne-Stokes respiration and obstructive sleep apnoea are independent risk factors for malignant ventricular arrhythmias requiring appropriate cardioverter-defibrillator therapies in patients with congestive heart failure. Eur Heart J 32:61–74
Latini R, Masson S, Anand IS, Missov E, Carlson M, Vago T, Angelici L, Barlera S, Parrinello G, Maggioni AP, Tognoni G, Cohn JN (2007) Prognostic value of very low plasma concentrations of troponin T in patients with stable chronic heart failure. Circulation 116:1242–1249
Ather S, Hira RS, Shenoy M, Fatemi O, Deswal A, Aguilar D, Ramasubbu K, Bolos M, Chan W, Bozkurt B (2013) Recurrent low-level Troponin I elevation is a worse prognostic indicator than occasional injury pattern in patients hospitalized with heart failure. Int J Cardiol 166:394–398
Masson S, Anand I, Favero C, Barlera S, Vago T, Bertocchi F, Maggioni AP, Tavazzi L, Tognoni G, Cohn JN, Latini R (2012) Serial measurement of cardiac troponin T using a highly sensitive assay in patients with chronic heart failure: data from 2 large randomized clinical trials. Circulation 125:280–288
Nakamura Y, Yoshihisa A, Takiguchi M, Shimizu T, Yamauchi H, Iwaya S, Owada T, Miyata M, Abe S, Sato T, Suzuki S, Oikawa M, Kobayashi A, Yamaki T, Sugimoto K, Kunii H, Nakazato K, Suzuki H, Saitoh S, Takeishi Y (2013) High-sensitivity cardiac troponin T predicts non-cardiac mortality in heart failure. Circ J
Tripp ME, Katcher ML, Peters HA, Gilbert EF, Arya S, Hodach RJ, Shug AL (1981) Systemic carnitine deficiency presenting as familial endocardial fibroelastosis: a treatable cardiomyopathy. N Engl J Med 305:385–390
Waber LJ, Valle D, Neill C, DiMauro S, Shug A (1982) Carnitine deficiency presenting as familial cardiomyopathy: a treatable defect in carnitine transport. J Pediatr 101:700–705
Masumura Y, Kobayashi A, Yamazaki N (1990) Myocardial free carnitine and fatty acylcarnitine levels in patients with chronic heart failure. Jpn Circ J 54:1471–1476
Yamada S, Suzuki H, Kamioka M, Suzuki S, Kamiyama Y, Yoshihisa A, Saitoh S, Takeishi Y (2013) Sleep-disordered breathing increases risk for fatal ventricular arrhythmias in patients with chronic heart failure. Circ J 77:1466–1473
Nakagomi A, Seino Y, Endoh Y, Kusama Y, Atarashi H, Mizuno K (2010) Upregulation of monocyte proinflammatory cytokine production by C-reactive protein is significantly related to ongoing myocardial damage and future cardiac events in patients with chronic heart failure. J Card Fail 16:562–571
Guven SF, Turkkani MH, Ciftci B, Ciftci TU, Erdogan Y (2012) The relationship between high-sensitivity C-reactive protein levels and the severity of obstructive sleep apnea. Sleep Breath 16:217–221
Randby A, Namtvedt SK, Einvik G, Hrubos-Strom H, Hagve TA, Somers VK, Omland T (2012) Obstructive sleep apnea is associated with increased high-sensitivity cardiac troponin T levels. Chest 142:639–646
Pekala J, Patkowska-Sokola B, Bodkowski R, Jamroz D, Nowakowski P, Lochynski S, Librowski T (2011) l-carnitine-metabolic functions and meaning in humans life. Curr Drug Metab 12:667–678
Omori Y, Ohtani T, Sakata Y, Mano T, Takeda Y, Tamaki S, Tsukamoto Y, Kamimura D, Aizawa Y, Miwa T, Komuro I, Soga T, Yamamoto K (2012) l-Carnitine prevents the development of ventricular fibrosis and heart failure with preserved ejection fraction in hypertensive heart disease. J Hypertens 30:1834–1844
Pauly DF, Pepine CJ (2003) The role of carnitine in myocardial dysfunction. Am J Kidney Dis 41:S35–S43
Serati AR, Motamedi MR, Emami S, Varedi P, Movahed MR (2010) l-carnitine treatment in patients with mild diastolic heart failure is associated with improvement in diastolic function and symptoms. Cardiology 116:178–182
Regitz V, Shug AL, Fleck E (1990) Defective myocardial carnitine metabolism in congestive heart failure secondary to dilated cardiomyopathy and to coronary, hypertensive and valvular heart diseases. Am J Cardiol 65:755–760
Matsui S, Sugita T, Matoba M, Murakami E, Takekoshi N, Shinka T, Matsumoto I (1994) Urinary carnitine excretion in patients with heart failure. Clin Cardiol 17:301–305
Vescovo G, Ravara B, Gobbo V, Dalla Libera L (2005) Inflammation and perturbation of the l-carnitine system in heart failure. Eur J Heart Fail 7:997–1002
Moller DS, Lind P, Strunge B, Pedersen EB (2003) Abnormal vasoactive hormones and 24-hour blood pressure in obstructive sleep apnea. Am J Hypertens 16:274–280
Zoccali C, Mallamaci F, Tripepi G (2002) Nocturnal hypoxemia predicts incident cardiovascular complications in dialysis patients. J Am Soc Nephrol 13:729–733
Foley RN, Parfrey PS, Sarnak MJ (1998) Epidemiology of cardiovascular disease in chronic renal disease. J Am Soc Nephrol 9:S16–S23
Sklar AH, Chaudhary BA, Harp R (1989) Nocturnal urinary protein excretion rates in patients with sleep apnea. Nephron 51:35–38
Kanbay A, Buyukoglan H, Ozdogan N, Kaya E, Oymak FS, Gulmez I, Demir R, Kokturk O, Covic A (2012) Obstructive sleep apnea syndrome is related to the progression of chronic kidney disease. Int Urol Nephrol 44:535–539
Dursunoglu D, Dursunoglu N, Evrengul H, Ozkurt S, Kuru O, Kilic M, Fisekci F (2005) Impact of obstructive sleep apnoea on left ventricular mass and global function. Eur Respir J 26:283–288
Grube M, Ameling S, Noutsias M, Kock K, Triebel I, Bonitz K, Meissner K, Jedlitschky G, Herda LR, Reinthaler M, Rohde M, Hoffmann W, Kuhl U, Schultheiss HP, Volker U, Felix SB, Klingel K, Kandolf R, Kroemer HK (2011) Selective regulation of cardiac organic cation transporter novel type 2 (OCTN2) in dilated cardiomyopathy. Am J Pathol 178:2547–2559
Adams SH, Hoppel CL, Lok KH, Zhao L, Wong SW, Minkler PE, Hwang DH, Newman JW, Garvey WT (2009) Plasma acylcarnitine profiles suggest incomplete long-chain fatty acid beta-oxidation and altered tricarboxylic acid cycle activity in type 2 diabetic African–American women. J Nutr 139:1073–1081
Mihalik SJ, Goodpaster BH, Kelley DE, Chace DH, Vockley J, Toledo FG, DeLany JP (2010) Increased levels of plasma acylcarnitines in obesity and type 2 diabetes and identification of a marker of glucolipotoxicity. Obesity (Silver Spring) 18:1695–1700
Hannon TS, Lee S, Chakravorty S, Lin Y, Arslanian SA (2011) Sleep-disordered breathing in obese adolescents is associated with visceral adiposity and markers of insulin resistance. Int J Pediatr Obes 6:157–160
Flemons WW, Littner MR, Rowley JA, Gay P, Anderson WM, Hudgel DW, McEvoy RD, Loube DI (2003) Home diagnosis of sleep apnea: a systematic review of the literature. An evidence review cosponsored by the American Academy of Sleep Medicine, the American College of Chest Physicians, and the American Thoracic Society. Chest 124:1543–1579
Acknowledgments
The authors acknowledge Yuko Niimura and Emiko Kaneda for their outstanding technical assistance, and Dr. Hajime Iwasa (Department of Public Health, Fukushima Medical University) for valuable advices on medical statistics. This study was supported in part by a Grant-in-Aid for Scientific Research (No. 25461061) from the Japan Society for the Promotion of Science.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miyata, M., Yoshihisa, A., Yamauchi, H. et al. Impact of sleep-disordered breathing on myocardial damage and metabolism in patients with chronic heart failure. Heart Vessels 30, 318–324 (2015). https://doi.org/10.1007/s00380-014-0479-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-014-0479-6