Abstract
Compared with the bare metal stent (BMS), suppression of neointimal growth in the sirolimus-eluting stent (SES) reduced restenosis at the cost of more exposed struts that could impose the risk of stent thrombosis. The present study was conducted to analyze neointimal coverage patterns of stents at a strut-level after implantation of BMS or SES with the use of optical coherence tomography (OCT). We enrolled 35 patients and analyzed neointimal coverage of every strut from 41 stents (BMS: n = 8, SES: n = 33) by using OCT at follow-up of the stent implantation. All of the 371 struts from eight BMSs were covered with ≥100 μm of neointima, while 19.8 and 3.5 % of 3,478 struts from 33 SESs were uncovered (neointimal thickness of <10 μm) and malapposed, respectively. The histogram of neointimal thickness showed basically normal distribution in BMS but skewed in SES. No regional difference in neointimal thickness was observed in BMS (proximal, 535.7 ± 25.2 μm; body, 532.4 ± 17.0 μm; distal, 485.8 ± 27.0 μm). In SES, however, the body segment showed thinner neointima [median 40 μm (interquartile range (IQR) 10–90 μm)] than proximal [60 μm (IQR 10–140 μm), p < 0.001] or distal [50 μm (IQR 10–110 μm), p < 0.001] segment, while uncovered and malapposed struts were more frequent in the proximal and body segments. In conclusion, SES, compared with BMS, showed more suppressed neointimal growth with regional variation: neointimal thickness was the least in the body part while the ratio of exposed and malapposed struts was minimal in the distal segment. OCT was useful for a strut-level analysis of neointimal coverage over the whole stent.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The advent of Sirolimus-eluting stents (SES) greatly reduced the rate of restenosis in comparison to bare metal stents (BMS) [1]. The process of neointimal coverage of SES, however, has not been well elucidated, leaving a new problem of stent thrombosis caused by delayed or incomplete neointimal stent strut coverage [2, 3]. Recent availability in the clinical practice of optical coherence tomography (OCT), which has a resolution of 12–15 μm [4], has enabled detailed measurement of neointimal thickness over stent struts [5, 6], but the way of analysis over the entire stent has not been established. We conducted OCT-based measurement of neointimal thickness over the stents at the chronic stage of their implantation, and here report a difference in longitudinal patterns of neointimal coverage between SES and BMS.
Materials and methods
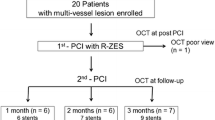
Between September 2005 and February 2008, 259 patients underwent follow-up coronary angiography at the chronic stage after the placement of BMS or SES in our hospital. Because of availability of catheterization laboratory schedule and personnel, we could conduct OCT examination once a week on a specified weekday, which made 107 patients as study candidates. After excluding patients with an ostial lesion of left or right coronary artery for technical difficulty of OCT image acquisition and requesting submission of written informed consent for the OCT examination, 35 patients agreed for enrollment in this study. This study was approved by the Ethics Committee of Kinki University Faculty of Medicine.
The OCT images were obtained with the Model M2 Cardiology Imaging System (LightLab Imaging Inc., Westford, MA, USA) and ImageWire (LightLab Imaging Inc.). Using a guiding catheter of 6 Fr or larger, a guidewire was inserted through a target stent beyond its distal margin, which was followed by an occlusion balloon to be advanced through the target stent. After the guidewire was replaced with the ImageWire, the occlusion balloon was pulled back proximal to the stent, where it was inflated to 0.4–0.6 atm to cut off the blood supply. Under infusion of lactated Ringer’s solution at a rate of 0.5–1.0 ml/s, OCT images were acquired for the entire length of the stent with an automated pullback at a rate of 1.0 mm/s.
Placement of two stents at a single lesion, with their edges overlapped, was counted as a single stent with its length and diameter substituted with the sum and the average of these two stents, respectively. Cross-sectional OCT images were analyzed every 2-mm from a distal end of stents. When the quality of image was poor, replacement with a nearby image of sufficient quality that was apart <1 mm from the original section was allowed. We assigned three sections located within 7 mm from the proximal and distal edges of the stent as image data of proximal and distal parts of the stent, respectively, and all the other sections as image data of the body part of the stent. In our analysis, we defined neointima as tissue material that was clearly distinguished from the stent as well as was located over the entire width of each strut (Fig. 1). The measurement of neointimal thickness, which was defined as a distance from the neointimal surface to the center reflection of a stent strut surface, was performed on an OCT screen that has the smallest measurement resolution of 10 μm.
According to overlying neointimal thickness and to its apposition to the vessel wall, each stent strut, except those over side branches, was classified into one of four categories (Fig. 2): THK (a group of thick covering), the neointimal thickness was ≥100 μm; THN (a group of thin covering), the neointimal thickness was between 10 μm and 100 μm; NON (a group of incomplete covering), the neointima was too thin to be detected (<10 μm); MAL (a group of malapposition), the strut was not attached to a vessel wall regardless of its neointimal thickness, with the distance between inner surface reflection of the strut and the vessel wall being ≥160 μm [5]. THK and THN were discriminated as a lesion that can be detected both by OCT and by IVUS (THK), or a lesion that can be detected by OCT but not by IVUS (THN).
Representative images of neointimal thickness patterns. THN, THK, NON, and MAL are described in the “Materials and methods” section
The results of coronary angiography were categorized for each stent according to the following criteria: when X-ray non-transparency of ≥2 mm in length was recognized at the stented segment before implantation, it was classified as calcification-positive; when a branch with a diameter of ≥2.0 mm arouse from the stented segment, it was regarded as side-branch positive; stent restenosis was defined when >50 % of stenosis, in comparison to mean of diameters of vessels proximal to and distal to the stent, was confirmed in coronary angiography.
The statistical analysis was carried out using R version 2.13.1 [7]. Categorical data was presented as counts and percentages, and compared by the Fisher’s exact test. Continuous variables were expressed as mean ± standard deviation (SD) or median [interquartile range (IQR): first quartile–third quartile], as indicated. Overall group comparisons of paired and unpaired continuous variables among three groups that were not normally distributed were analyzed with the Friedman test and the Kruskal–Wallis test, respectively. Their between-group comparisons were assessed by the Steel–Dwass test [8]. The other continuous variables in two-group comparisons were tested with Student’s t test or the Mann–Whitney test, as appropriate. All reported p values are two-sided.
Results
Groups of BMS and SES consisted of eight stents from seven patients and 33 stents from 28 patients, respectively. The clinical features of enrolled patients are shown in Table 1. There were no significant differences in patient background between the two groups as for age, gender, and coronary risk factors. The patient ratio of acute coronary syndrome (ACS) as clinical diagnosis at stent implantation was 71.4 % (5/7) and 7.1 % (2/28) in the BMS and SES groups, respectively (p = 0.002). All patients in both groups were under dual antiplatelet therapy of aspirin as well as ticlopidine or clopidogrel, and no significant group difference was observed in statin or angiotensin-converting enzyme inhibitor (ACEI)/angiotensin II receptor blocker (ARB) medications.
The procedural and stented-lesion characteristics are shown in Table 2. The interval from stent placement to OCT was 244.6 ± 50.6 days in the SES group, which was significantly longer than the 192.9 ± 28.4 days in the BMS group (p = 0.010). The stent diameter was larger in the BMS group than in the SES group (3.28 ± 0.42 vs. 2.77 ± 0.37 μm, p = 0.003), but there was no statistical group difference in stent length. Overlapping placement of stents were performed in 2 patients in the BMS group while no case was observed in the SES group (p = 0.035). A lack of malapposition was confirmed in all the cases where IVUS was used after the stent placement procedure. No occluded stent was observed in either group at follow-up coronary angiography, but angiographic restenosis was found significantly more in the BMS group (p = 0.019).
Median neointimal thickness in the SES group was 50 μm (IQR 10–110 μm), which was significantly thinner than 490 μm (IQR 335–660 μm) in the BMS group (p < 0.001). The distribution of neointimal thickness over stent struts for proximal, body and distal segments are presented in Fig. 3. In the BMS group, the Kolmogorov–Smirnov test confirmed the normality in data sets of any portions of the stents, but the Shapiro–Wilk test detected deviation from normality only in the data set of the body portion. Analysis with Bartlett’s test showed equality of variances among three data sets. Therefore, the Kruskal–Wallis test for nonparametric data as well as one-way ANOVA for parametric data was conducted to compare them. Neither statistical method detected any significant difference in neointimal thickness among 3 portions of the BMS. In the SES group, histograms of the overall distributions of neointimal thickness in each stent portion were consistently upward-skewed and indicated the need of nonparametric testing for comparison. The Kruskal–Wallis test showed significant differences in neointimal thickness among three portions of stents, and multiple testing by the Steel–Dwass method demonstrated that neointimal thickness at the body of the stent [40 μm (IQR 10–90 μm)] was significantly thinner than those of proximal [60 μm (IQR 10–140 μm), p < 0.001] and distal [50 μm (IQR 10–110 μm), p < 0.001] parts.
Distribution of neointimal thickness over each strut among three stent segments of BMS (a) and SES (b). No statistical difference was observed in BMS. In SES, however, the struts in the body part had thinner neointima than those in the proximal or distal parts. BMS bare metal stent, SES sirolimus-eluting stent
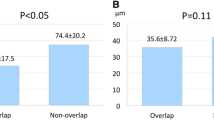
In a strut-level analysis, the ratio of neointimal thickness pattern over struts in the SES group was as follows: THK 24.9 %, THN 51.8 %, NON 19.8 %, and MAL 3.5 %. In the BMS group, the ratios of THK and THN were 97.8 and 2.2 %, respectively, while no strut was classified as NON or MAL (Fig. 4). In a stent-level analysis of the SES group, covering of all the struts were observed only in two out of 33 stents (6.1 %), <5 % of NON struts were found in five stents (15.2 %), and ≥5 % of NON struts were found in 26 stents (78.8 %). Because malapposed as well as uncovered struts were considered to be risk factors for stent thrombosis [9], the distribution of NON and MAL strut ratio in three segments of each stent is compared and presented in Fig. 5. It showed clear difference that was statistically significant with the Friedman test. Multiple testing by the Steel–Dwass method showed that the distal segment [median 4.3 % (IQR 0.0–19.0 %)] had a significantly lower ratio of NON + MAL struts compared with the proximal [median 14.3 % (IQR 5.6–34.3 %), p = 0.002] and the body [median 18.4 % (IQR 5.9–33.3 %), p = 0.003] segments.
Distribution of strut ratio of neointimal thickness patterns in BMS and SES. BMS bare metal stent, SES sirolimus-eluting stent. THN, THK, NON, and MAL are described in the “Materials and methods” section
Distribution of NON + MAL strut ratio calculated in three segments of individual SES. The distal segment had significantly lower ratio of NON + MAL struts than proximal or body parts. SES sirolimus-eluting stent. NON and MAL are described in the “Materials and methods” section
Discussion
The rate of restenosis, the unresolved problem in percutaneous coronary intervention treatment, was greatly reduced by the advent of drug-eluting stent [1]. On the other hand, the risk of stent thrombosis caused by incomplete neointimal coverage of stent struts has emerged as a new problem [10, 11]. Previous reports, which observed neointima formation over the BMS with angioscopy, showed that no covering occurred in 2–4 weeks, but most of the stents were buried under a white neointima in 3 months [12]. This neointimal coverage is considered to prevent stent thrombosis by keeping blood from the metal of stent as well as from vulnerable plaques under the stent.
Several intravascular ultrasound (IVUS) studies of stent struts revealed that neointimal thickness over drug-eluting stent at the chronic stage was mostly too thin to be measured with IVUS because of its resolution of about 100 μm [13]. However, OCT, which has ten-times higher resolution than IVUS [14], could enable such analysis [15]. In our study, we could detect neointimal coverage of <100 μm in 51.8 % of stent struts in the SES group, which could not have been identified by IVUS. Our result is consistent with a report by Matsumoto et al. [5] where the OCT analysis revealed that 64 % of neointimal thickness was <100 μm after 6 months of SES placement.
Comparison of neointimal thickness between SES and BMS groups showed that the thickness in the SES group was significantly thinner than that in the BMS group. Takano et al. [16] reported that neointimal thickness after 3 months of SES placement was 29 ± 41 μm, and Goto et al. [17] reported that it was 80 ± 30 μm after 8 months. Our data was consistent with the latter study where mean ± SD of SES neointimal thickness was 77.5 ± 99.5 μm in the mean observation period from stent placement to OCT examination of 263.2 ± 93.0 days, that is, about 8.8 months.
In the present study, we succeeded in measuring and classifying neointimal coverage over each stent strut, and in analyzing the difference between BMS and SES as well as among the proximal, body, and distal segments. After the application of OCT in clinical practice, several studies classified struts according to existence or non-existence of vessel wall-attachment and neointimal coverage [5, 6, 16, 17], but there seems no consensus for expressing the status of neointimal stent coverage. Grouping of widely varied neointimal thickness among struts into a single entity of neointimal coverage would not correctly represent the stent status.
Therefore, we started with histographic expression of neointimal thickness data at a strut-level with subgrouping into proximal, body and distal segments of stent. BMS and SES showed clear contrast in measured values of neointimal thickness and their distribution: neointimal thickness of BMS was several hundred micrometers thick and basically normally distributed, while that of SES showed skewed distribution with 0 μm as the most frequent measurement value. Neointimal thickness showed no regional difference in BMS, while it was thinner in the body part in SES. The lack of NON or MAL struts was another characteristic of BMS. Analysis of the ratio of NON and MAL struts in each segment of SES revealed a lower ratio of those struts in the distal portion. Therefore, the SES group showed not only thinner mean neointimal thickness but also wider regional variability in the neointimal coverage pattern than the BMS group.
Takano et al. [16], in their neointima analysis using OCT 3 months after the SES placement, reported that 15 % of struts had no covering and its ratio was higher in patients with a diagnosis of ACS at the stent placement (ACS 18 % vs. non-ACS 13 %). Goto et al. [17] reported that 16 % of struts had no covering in their OCT examination 6–10 months after the SES placement. Compared with those reports, our result (19.8 %) showed a higher ratio of incompletely covered struts in the SES group, which consisted mostly of non-ACS patients. One possible explanation would be in our definition of neointimal coverage: complete covering of a strut with continuity from a vessel wall was required. Even if an amount of tissue image was recognized over a strut, a lack of continuity from the vessel wall on either side was judged as incomplete covering and classified as NON.
Currently, OCT assessment of neointimal stent coverage has no universal criteria for the amount of tissue over a strut or for the % ratio of covered struts in each stent to judge the stent as sufficiently covered by neointima. As observed, NON and MAL struts were not observed in the BMS group and the ratio of those struts in a single stent varied in the SES group. The proper definition of sufficient neointimal coverage of a strut and a stent would await further discussion.
In an analysis of neointimal stent strut coverage pattern among different parts within stents, no significant regional difference in the neointimal thickness was observed in the BMS group while an interesting finding was observed in the SES group. Thicker neointimal thickness in the proximal and distal parts than in the body part was consistent with the previous report [18], which demonstrated that the in-stent restenosis pattern of focal margin restenosis was more frequent in the SES-treated than in the BMS-treated patients with restenosis. Higher and lower ratio of NON + MAL struts in the body part with thinner neointima and in the distal part with thicker neointima, respectively, of SES were also self-explanatory. However, higher ratio of NON + MAL struts in the proximal part of SES with thicker neointima was a counter-intuitive finding. In the previous report [18], 61.3 % of the SES patients who developed restenosis had the intimal hyperplasia localized to the margin of the stent despite the actually larger edge lumen dimensions at follow-up in the SES-treated patients. In addition, comparison of regional differences in the rate of restenosis between SES and BMS showed that significantly lower rate of restenosis was observed within and at the distal edge of SES than those of BMS, while no difference was observed in the proximal edge [18]. Our finding of unexpected higher ratio of NON + MAL struts despite thicker neointima may explain the less favorable result in the proximal edge of SES-treated lesion [18–20].
This study had several limitations. First, the number of enrolled stents in the BMS group was small (n = 8). Second, the ratio of ACS was different, 71.4 % in the BMS group vs. 7.1 % in the SES group. In the approval by the Ministry of Health, Labor and Welfare in Japan, the use of SES had been contraindicated until 2012 in AMI patients within 72 h from its onset and in patients where critical thrombus was detected at the target coronary lesion. On the other hand, the restenosis rate was much less with SES than with BMS [1]. This made us choose BMS and SES preferentially in ACS and non-ACS patients, respectively, which resulted in the small sample size of the BMS group. Third, the stent diameter was larger in the BMS than in the SES group. Expected lower rate of restenosis with SES made us preferentially select SES for a lesion with smaller diameter in non-ACS patients. Despite this limitation, we think that our data was worth being presented as representing data of more actual cases in clinical practice. Finally, the follow-up period was significantly different between the BMS and SES groups. Readmission schedule of repeat coronary angiography was on discretion of attending physicians, and they followed the evidence that neointimal tissue volume peaks at 6 months after BMS implantation [21]. For SES implantation, no such evidence existed but they shared the idea that the peak of restenosis would be delayed for up to 60 days for the period sirolimus is released [22, 23]. In that sense, our study lacked rigor for proving the difference between BMS and SES. However, statistically significant neointimal regression in BMS was detected from 6 months to 3 years, but not from 6 months to 1 year, after stent implantation [21], suggesting that the effect of 2 months’ difference between 6 months and 1 year after stent implantation in our analyzed data would be minimal. Therefore, we think that our data still had value in showing different behavior of neointimal formation according to the types of stents, with special emphasis on regional difference within SES-treated lesion.
Compared with extensive analysis on clinical outcome with different types of drug-eluting stents [24, 25], quantitative regional analysis of neointimal thickness at a strut-level has been quite limited [26]. Despite the discontinuation of SES production announced in 2011, we believe that our approach, combining strut-level and stent regional analyses with vigorous application of non-parametric statistical methods, could be effective to unravel specific characteristics of neointimal formation in other types of drug-eluting stents.
In conclusion, SES showed more heterogeneity than BMS in neointimal stent coverage: strut-level neointimal coverage patterns; distribution of neointimal thickness along stent regions (proximal, body, and distal parts); occurrence rates of NON and MAL struts in each stent. Therefore, in the assessment of neointimal coverage of SES, neither evaluation of a part of stent, nor a single value of mean neointimal thickness would sufficiently represent the neointimal coverage status of a whole stent. Instead, a better index based on measurements at multiple sites and their integration for each stent would be required, and we hope that our approach would serve as one solution.
References
Moses JW, Leon MB, Popma JJ, Fitzgerald PJ, Holmes DR, O’Shaughnessy C, Caputo RP, Kereiakes DJ, Williams DO, Teirstein PS, Jaeger JL, Kuntz RE (2003) Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med 349:1315–1323
Oyabu J, Ueda Y, Ogasawara N, Okada K, Hirayama A, Kodama K (2006) Angioscopic evaluation of neointima coverage: sirolimus drug-eluting stent versus bare metal stent. Am Heart J 152:1168–1174
Finn AV, Joner M, Nakazawa G, Kolodgie F, Newell J, John MC, Gold HK, Virmani R (2007) Pathological correlates of late drug-eluting stent thrombosis: strut coverage as a marker of endothelialization. Circulation 115:2435–2441
Regar E, Ligthart J, Bruining N, van Soest G (2011) The diagnostic value of intracoronary optical coherence tomography. Herz 36:417–429
Matsumoto D, Shite J, Shinke T, Otake H, Tanino Y, Ogasawara D, Sawada T, Paredes OL, Hirata K, Yokoyama M (2007) Neointimal coverage of sirolimus-eluting stents at 6-month follow-up: evaluated by optical coherence tomography. Eur Heart J 28:961–967
Miyoshi N, Shite J, Shinke T, Otake H, Tanino Y, Ogasawara D, Sawada T, Kawamori H, Kato H, Yoshino N, Kozuki A, Hirata K (2010) Comparison by optical coherence tomography of paclitaxel-eluting stents with sirolimus-eluting stents implanted in one coronary artery in one procedure—6-month follow-up. Circ J 74:903–908
R Development Core Team (2011) R: a language and environment for statistical computing R Foundation for Statistical Computing, Vienna, ISBN 3-900051-07-0. http://www.R-project.org/
Hollander M, Wolfe DA (1999) Distribution-free two-sided all-treatments multiple comparisons based on pairwise rankings—general configuration (Dwass, Steel, Critchlow–Fligner). In: Nonparametric statistical methods. 2nd ed. Wiley, New York, pp 240–249
Chen BX, Ma FY, Luo W, Ruan JH, Xie WL, Zhao XZ, Sun SH, Guo XM, Wang F, Tian T, Chu XW (2008) Neointimal coverage of bare-metal and sirolimus-eluting stents evaluated with optical coherence tomography. Heart 94:566–570
McFadden EP, Stabile E, Regar E, Cheneau E, Ong AT, Kinnaird T, Suddath WO, Weissman NJ, Torguson R, Kent KM, Pichard AD, Satler LF, Waksman R, Serruys PW (2004) Late thrombosis in drug-eluting coronary stents after discontinuation of antiplatelet therapy. Lancet 364:1519–1521
Pfisterer M, Brunner-La Rocca HP, Buser PT, Rickenbacher P, Hunziker P, Mueller C, Jeger R, Bader F, Osswald S, Kaiser C (2006) Late clinical events after clopidogrel discontinuation may limit the benefit of drug-eluting stents: an observational study of drug-eluting versus bare-metal stents. J Am Coll Cardiol 48:2584–2591
Asakura M, Ueda Y, Nanto S, Hirayama A, Adachi T, Kitakaze M, Hori M, Kodama K (1998) Remodeling of in-stent neointima, which became thinner and transparent over 3 years: serial angiographic and angioscopic follow-up. Circulation 97:2003–2006
Mintz GS (2007) Features and parameters of drug-eluting stent deployment discoverable by intravascular ultrasound. Am J Cardiol 100:26M–35M
Guagliumi G, Sirbu V (2008) Optical coherence tomography: high resolution intravascular imaging to evaluate vascular healing after coronary stenting. Catheter Cardiovasc Interv 72:237–247
Kim JS, Jang IK, Fan C, Kim TH, Kim JS, Park SM, Choi EY, Lee SH, Ko YG, Choi D, Hong MK, Jang Y (2009) Evaluation in 3 months duration of neointimal coverage after zotarolimus-eluting stent implantation by optical coherence tomography: the ENDEAVOR OCT trial. JACC Cardiovasc Interv 2:1240–1247
Takano M, Inami S, Jang IK, Yamamoto M, Murakami D, Seimiya K, Ohba T, Mizuno K (2007) Evaluation by optical coherence tomography of neointimal coverage of sirolimus-eluting stent three months after implantation. Am J Cardiol 99:1033–1038
Goto I, Itoh T, Kimura T, Fusazaki T, Matsui H, Sugawara S, Komuro K, Nakamura M (2011) Morphological and quantitative analysis of vascular wall and neointimal hyperplasia after coronary stenting: comparison of bare-metal and sirolimus-eluting stents using optical coherence tomography. Circ J 75:1633–1640
Popma JJ, Leon MB, Moses JW, Holmes DR Jr, Cox N, Fitzpatrick M, Douglas J, Lambert C, Mooney M, Yakubov S, Kuntz RE (2004) Quantitative assessment of angiographic restenosis after sirolimus-eluting stent implantation in native coronary arteries. Circulation 110:3773–3780
Lemos PA, Saia F, Ligthart JM, Arampatzis CA, Sianos G, Tanabe K, Hoye A, Degertekin M, Daemen J, McFadden E, Hofma S, Smits PC, de Feyter P, van der Giessen WJ, van Domburg RT, Serruys PW (2003) Coronary restenosis after sirolimus-eluting stent implantation: morphological description and mechanistic analysis from a consecutive series of cases. Circulation 108:257–260
Corbett SJ, Cosgrave J, Melzi G, Babic R, Biondi-Zoccai GG, Godino C, Morici N, Airoldi F, Michev I, Montorfano M, Sangiorgi GM, Bonizzoni E, Colombo A (2006) Patterns of restenosis after drug-eluting stent implantation: insights from a contemporary and comparative analysis of sirolimus- and paclitaxel-eluting stents. Eur Heart J 27:2330–2337
Kimura T, Yokoi H, Nakagawa Y, Tamura T, Kaburagi S, Sawada Y, Sato Y, Yokoi H, Hamasaki N, Nosaka H, Nobuyoshi M (1996) Three-year follow-up after implantation of metallic coronary-artery stents. N Engl J Med 334:561–566
Kipshidze N, Leon MB, Tsapenko M, Falotico R, Kopia GA, Moses J (2004) Update on sirolimus drug-eluting stents. Curr Pharm Des 10:337–348
Wessely R, Schomig A, Kastrati A (2006) Sirolimus and paclitaxel on polymer-based drug-eluting stents: similar but different. J Am Coll Cardiol 47:708–714
Higashitani M, Mori F, Yamada N, Arashi H, Kojika A, Hoshi H, Minami Y, Yamaguchi J, Yamauchi T, Takagi A, Ogawa H, Hagiwara N (2011) Efficacy of paclitaxel-eluting stent implantation in hemodialysis patients. Heart Vessels 26:582–589
Buja P, Lanzellotti D, Isabella G, Napodano M, Panfili M, Favaretto E, Iliceto S, Tarantini G (2012) Comparison between sirolimus- and paclitaxel-eluting stents for the treatment of older patients affected by coronary artery disease: results from a single-center allcomers registry. Heart Vessels 27:553–558
Guagliumi G, Musumeci G, Sirbu V, Bezerra HG, Suzuki N, Fiocca L, Matiashvili A, Lortkipanidze N, Trivisonno A, Valsecchi O, Biondi-Zoccai G, Costa MA (2010) Optical coherence tomography assessment of in vivo vascular response after implantation of overlapping bare-metal and drug-eluting stents. JACC Cardiovasc Interv 3:531–539
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ikuta, S., Kobuke, K., Iwanaga, Y. et al. Difference in neointimal coverage at chronic stage between bare metal stent and sirolimus-eluting stent evaluated at stent-strut level by optical coherence tomography. Heart Vessels 29, 320–327 (2014). https://doi.org/10.1007/s00380-013-0376-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-013-0376-4