Abstract
Purpose
The primary aim of this study to comparison of reusable and disposable flexible ureterorenoscope (fURS) efficiency in lower pole renal stone disease management. In addition, the secondary goal of this study was to evaluate the factors affecting stone-free rates (SFR) in lower pole stones.
Materials and methods
A prospective case–control study utilizing data from 122 consecutive ureteroscopic cases. The patients were divided into two groups according to the ureterorenoscope employed in the surgical intervention as disposable fURS (Group1, n:52) and reusable fURS (Group 2, n:70). Demographic characteristics, stone size, infundibulopelvic angle (IPA), SFR, hospitalization time, intraoperative complication rate (CR), operative time, preoperative or postoperative JJ stenting, and postoperative CR were analyzed.
Results
There was no statistical difference between the demographic and renal stone-related data between the groups. Likewise, no difference is observed in term of intraoperative and postoperative outcomes such as fluoroscopy time, CR, and hospitalization time between the groups. Although SFR was higher in the disposable fURS group, there was no difference statistically. However, the operative time was longer in reusable fURS Group (47.02 ± 9.91 min in Group 1, and it was 57.97 ± 14.28 in Group 2) (p: 0.001). The multivariate regression analysis result to evaluate the factors of effect to operative time; the use of disposable fURS was associated with a 10.95-min decrease in procedure duration (p < 0.001).
Conclusions
Disposable fURS and reusable fURS have similar clinical efficiency and complication rates in the treatment of lower calyceal stones with RIRS. Nevertheless, disposable fURS is a useful treatment option for increased stone volume due to the advantages such as shorter operative time.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Flexible ureterorenoscopy is currently common treatment modality for kidney stone disease [1]. Its use in treatment of stone disease has been gradually increasing, due to the growing nephrolithiasis prevalence [1]. In addition to these advancements, with the development of the holmium laser, retrograde intrarenal surgery (RIRS) has taken its place as an important option in kidney stone treatment [2]. According to EAU guidelines, RIRS and shock wave lithotripsy (SWL) are recommended as first-line treatment choice for renal stones less than 20 mm [1]. They have also become second-line treatment choice for stones > 20 mm. In the presence ofunfavorable factors for SWL in 10–20 mm lower pole stones, the first recommended treatment modality is RIRS [1]. The success of SWL in lower pole stones varies between 25 and 95% and several factors affect this success [3,4,5]. In recent years, in meta-analysis comparisons of RIRS and SWL, the needle is turning in favor of RIRS every day due to its stone-free rate and various advantages [4, 5]. Therefore, the use of RIRS in these stones has increased significantly in recent years [1].
New generation fURS has exceptional qualities such as high digital imaging quality, or high passive and active flexion ability [6]. Despite that evolution of fURS, the instruments are still fragile and prone to damage. The fragility of fURS and associated maintenance–repair costs are still important financial and logistic challenges for endourology centers. In the light of frequently usage of RIRS, the single use fURS was developed and started to be used [7, 8]. The tests between disposable and reusable fURS yielded comparable results [9, 10]. However, its impact in the lower calyx stones remains uncertain.
The primary aim of the present study is to compare the efficacy of reusable and disposable fURS in lower pole renal stone disease. A secondary aim is to evaluate the factors affecting the stone-free rates (SFR) of lower pole stones.
Materials and methods
All RIRS procedures conducted in a tertiary referral center in Konya, Turkey between January 2018 and May 2020 were evaluated in this prospective case–control study. Patients aged 18 and above with lower pole stones were included in the present study. Patients with isolated lower calyceal stones and patients who were unsuitable or unwilling for SWL and PNL treatment were included the present study. Each session of surgery for patients with multiple sessions of RIRS was evaluated as a separate surgical procedure. Patients under 18 years of age, patients without stones in the isolated lower calyx, patients who had previous open surgery and kidney anomalies were excluded from the study. Consequently 122 patients and renal units were determined to meet the inclusion criteria. Non-contrast abdomen computed tomography (CT) was used as the preoperative imaging method. The majority of procedures were performed under general anesthesia. Twenty-two patients who could not be performed general anesthesia were performed spinal anesthesia (9 patients in Group 1, and 13 patients in Group 2). All procedures were performed in lithotomy position by the same surgeons. All surgery sessions performed routinely in two operation rooms. One digital disposable fURS (9.5 Fr, Uscope 3022®, Zhuhai Pusen Medical Technology Co, Ltda., Zhuhai, China) was used between March 2018 and December 2019, and one digital reusable fURS (7.5 Fr, Flex-X2S®, Karl Storz, Tuttlingen, Germany) was used between December 2019 to May 2020 randomly during all surgical sessions.
In all cases, a safety guidewire was placed under fluoroscopic guidance. Semi-rigid ureteroscopy (URS) (8 Fr Karl Storz, Tuttlingen, Germany) was performed to evaluate the ureteral pathologies. Afterwards, retrograde pyelography was performed for to observe renal and ureteral anatomy. In Group two, 9.5/11 Fr ureteral access sheath (UAS) was placed via the second guidewire guidance. If the UAS did not pass through the distal ureter, a fURS was sent on the guidewire immediately and the stone was fragmented. In Group one, the UAS was not used due to its large diameter (12/14 Fr) not to increase ureteral complications. After semi-rigid URS, fURS was placed via the second guidewire under fluoroscopy. If semi-rigid URS could not be performed in both groups or fURS could not be placed into the ureter, JJ stent was inserted to ureter and the operation was postponed for 2 weeks later.
For laser lithotripsy, a 30-Watts holmium laser (Medilas H Solvo®, Dornier MedTech Europe GmbH, Wessling, Germany) with 270-micron fibers was used in all cases. All procedures were performed uniformly, using intracorporeal lithotripsy laser parameters in dusting or fragmentation mode depending on the characteristics of the stone.
At the end of each surgical intervention, JJ stent was inserted according to the clinical experience of the surgeon, ureteral edema, residual stone presence, and hemorrhage. Other patients were followed up without the insertion of JJ stent.
The patients were divided into two groups as disposable fURS (Group1) and reusable fURS (Group 2).
Analyzed parameters included demographic characteristics, stone size, infundibulopelvic angle (IPA), SFR, hospitalization time, intraoperative complication rate (CR), operative time, preoperative or postoperative JJ stenting, and postoperative CR. At the time of the surgery, the measurements of the anatomical characteristics of the lower pole (infundibular length, infundibular width and IPA) were obtained using a radioscopic retrograde ureteropyelography according to the method described by Elbahnasy et al. [3]. These parameters were compared as well between both groups.
Clavien–Dindo scale was used to classified intra and postoperative complications [11].
The patients without any postoperative complaints were discharged on the first postoperative day. The patients were evaluated after 2–4 weeks in outpatients’ clinic. Postoperative imaging methods were X-ray and/or ultrasonography. The patients who had 3 mm or smaller stone fragments were considered as stone free patients. Patients’ stone free status was accepted as surgical success. The surgical time was accepted as during between started to the insertion of the UAS and end of stone fragmentation.
Statistical analyses
Statistical analyses of the data obtained from these procedures were conducted using 23.0 version of the Statistical Package for Social Sciences (SPSS®, IBM in Armonk, New York, USA). Chi-square test was conducted for univariate analysis of the groups. An independent T-test was performed to obtain parametric data, and Mann–Whitney U test to obtain non-parametric data. We compared demographic, kidney stone-related factors (HU, IPA, etc.), pre and postoperative values between groups.
A multivariate evaluation was conducted with a logistic regression analysis the factors affecting SFR between groups. We included factors such as stone size, number of stones, UAS use, IPA, Hounsfield units (HU) value, presence of preoperative hydronephrosis, gender, and using disposable or reusable fURS in these methods.
Furthermore, we performed univariate analysis for factors affecting operative time. Finally, the multivariate analysis after univariate analyses was conducted.
Factors that considered being statistically significant in the univariate analysis, affecting operative time were also included in the multivariate analysis.
A confidence interval of 95% and a threshold level of p of less than 0.05 were considered as indicators of statistical significance.
Results
Out of the 122 patients, 52 were in Group 1 and 70 in Group 2. Mean stone size was 11.75 ± 4.89 mm in Group 1 and 12.17 ± 4.44 in Group 2. There were no differences between to the Groups in terms of stone size (p: 0.621). All stones were located in the lower calyx. No difference was observed among reusable and disposable groups in terms of age, gender, comorbidity, stone laterality, IPA, number of stone, HU, and demographic and preoperative parameters (All parameters p > 0.05) (Table 1). Preoperative JJ stent was inserted in 15 (28.8%) of the patients in Group 1, and 25 (35.7%) of the patients in Group 2. This rate was similar statistically (p: 0.424).
The UAS could not inserted in any of the patients in Group 1. The situation may cause due to the high diameter of UAS for disposable URS. Also, we could not place the UAS to 51 patients in Group 2. The UAS using was higher in Group 2 than Group 1 (p < 0.001).
Postoperative JJ stents were inserted to 98 patients (80.3%) in both Groups (45 patient in Group 1; and 53 patient in Group 2). Other patients (7 patients in Group 1; and 17 patients in Group 2) were stentless at the end of surgery. This postoperative stenting’ rate was similar between the Groups (p: 0.137).
Among the intracorporeal laser lithotripsy techniques was dusting the most frequently used technique in both groups (63.9%), in the remaining patients stones were extracted with a basket and dusting was performed in the pelvis.
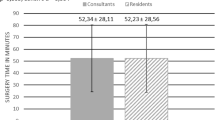
The operative time was 47.02 ± 9.91 min for Group 1, and 57.97 ± 14.28 min for Group 2. This time was higher in Group 2 (p: 0.001). SFR was achieved in 84.6% of the patients (44 patients) in Group 1. This ratio was 80% (56 patient) in Group 2, and there were no differences between the Groups (p: 0.512). The fluoroscopy time was 72 ± 31 s in Group 1 and 69 ± 28 s in Group 2 (p: 0.528). The CR was seen in 17.3% of (9 patients) Group 1, and in 10% (7 patients) of Group 2. CR rate was similar for both Groups (p: 0237). Most of the complications encountered were of Clavien I–II grade. We did not observe Clavien grade IV–V complications in any of the participants. There is no statistically significant difference in terms of hospitalization time between the two groups (p: 0.15) (Table 2).
The results of the multivariate analyses have shown that the factors with an impact on SFR after RIRS are IPA (p: 0.001), stone number (p: 0.04), and stone size (p: 0.001). Neither fURS nor the other factors evaluated during the multivariate analyses do have an effect on the success of the surgery conducted. Factors with an impact on stone clearance are presented in Supplementary Table 2.
The univariate regression result to evaluate the factors with an effect of operative time has shown that the use of disposable fURS was associated with a 10.95-min decrease in the operative time (p < 0.001). Moreover, HU degree (p: 0.29), increasing stone size (p < 0.001), stone number (p < 0.001), UAS use (p: 0.016) and IPA (p: 0.013) were associated with significant increases in the operative time. The monovariate analysis results to evaluate the factors with an effect of operative time have shown Fig. 1. However, on evaluating the factors with an impact on operative time with multivariate analyses have shown that HU degree and IPA were not associated with operative time. However, like in the univariate analyses, the use of reusable fURS (p < 0.001), increasing stone size (p < 0.001), presence of multiple stones (p: 0.036), were associated with increased operative time.
Factors effecting operative time are presented in Supplementary Table 3.
Discussion
In the present study, disposable fURS and reusable fURS were compared in the treatment of lower pole stones. The surgical time is shorter with RIRS performed with disposable flexible ureteroscope. Furthermore, the success rate of disposable fURS had a higher success rate in lower pole stones operations compared to reusable fURS, this is not statistically significant (88% vs 86%).
Flexible ureterorenoscopy in stone management has become an indispensable part of daily urology practice. SWL and endoscopic modalities are the first recommended treatment modalities, especially for lower calyceal stones with a diameter less than 2 cm [1]. In systematic review and meta-analysis, it has been stated that SFR is higher in RIRS compared to SWL, especially in 10–20 mm lower calyceal stones [12, 13]. Also in another study, retreatment was less, and transition to normal life was earlier in the RIRS group [14]. Although the need for more prospective randomized studies is obvious, RIRS has an important therapeutic advantage in the treatment of lower calyceal stones.
There are several factors affecting the success of RIRS in lower calyceal stone SFR. In the study of Jessen et al., a very low IPA (< 30°) and a long infundibulum have a negative effect on the SFR. However, the same study has also stated that even in case of unfavorable anatomic conditions, a complete stone clearance is achievable with secondary procedures [15]. In the present study, IPA, stone load, HU and number all affected SFR independent of the tools employed in the procedure.
Many authors have determined that RIRS has a high efficacy in treatment for renal stones [12,13,14]. In spite of the technological progression in scope, design, and function, durability continues to be main concern in starting and maintaining this surgery [16]. Due to these advancements, success of surgical outcomes were improved [12, 17]. Replacement and repair of these scopes necessitate high costs and vitally important time. These instruments may require repair after 5–40 usages [16, 18]. One of the most important damage risk factors in fURS, with high maintenance and repair costs, is exceeding the deflection limit of the device during surgery. This damage was determine to occur most often during the treatment of lower pole stones [19].
To overcome these handicaps, disposable fURS have been developed [17]. Disposable fURS have been determined to be comparable with reusable fURS in terms of image resolution and flexibility [18]. These devices, which have come more and more into use in recent years, comparative for their in effectiveness compared to reusable devices became a necessity [16].
There is no certainty about the economic superiority of disposable devices over reusable ones. However, there are publications stating that it is more economical in centers with a low volume of cases or in large volume lower pole stones [20]. In the study of Martin et al., it has been stated that the use of disposable equipment is economically superior in centers where less than 99 flexible ureteroscopy is performed annually [21]. In the present study, no cost calculation was made due to the variability in the financial data inhibiting a precise calculation of the cost.
In the study of Mager et al., it was stated that no significant difference was found between SFR between disposable fURS and reusable fURS in the treatment of kidney stones (81% vs 87%) [8]. In the same study, no significant difference was observed between the two devices in terms of operative time and fluoroscopy time [8]. In the study of Usawachintachit M et al., they reported that procedural outcomes and complications were comparable between disposable and reusable groups. In their study, when they evaluated all kidney stones, surgeries performed with disposable fURS were statistically significantly shorter than those intervened with reusable fURS [20]. In study by Salvadó et al., they compared to efficiency of disposable and reusable devices in lower calyceal stones. They observed that the surgery time and the fluoroscopy time were been shorter in the disposable fURS group [22]. In our study, as in other studies, the SFR rate was similar in both fURS groups. HU value, IPA, stone size, and stone number were factors affecting SFR in our analysis.
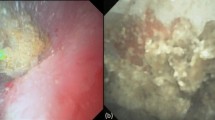
The most important difference in both groups was in the operative time in our study. The surgery time of disposable fURS was 10 min shorter, on average, than reusable fURS. In univariate analysis, operative time was affected by stone size, stone number, IPA, and HU. We can, however, speculate on factors that might account for differences in procedural time. We think that the operative time is affected by technical and surgical factors. The disposable scope is lighter than the reusable scope and flexes like a new scope with every case. In study by Usawachintachit et al., similar to our study, intrinsic characteristics may explain the faster performance of disposable fURS [20]. Although the endoscope angulation and up–down flexion feature of disposible fURS is similar to the reusable fURS in the empty working channel, these features of disposable URS are better when the insertion of laser fiber (Fig. 2) [23]. Especially in reusable fURS that has been used many times, this difference is obvious. Therefore, disposable fURS may be easier to target during fragmentation the stone. Also, the reflexes of surgeons to protect the reusable fURS may limit the angulation and up–down flex. We think that this situation could be effect the operative time. Although we are not sure about the explanation of this time difference, stone size and stone number are important factors affecting the operative time. In addition, these factors are also correlate with multivariate analysis. More studies are needed to evaluate the factors affecting the operative time.
The impact of the use of a UAS in RIRS, SFR is controversial [24]. According to EAU Guidelines; the use of UAS depends on the surgeon’s preference [25]. Also, the association between the use of a UAS and ureteral damage has been underreported for many years. The increased diameter of UAS is related to the growing ureteral damage, in experimental and human studies, the damage can exceed 50% [24, 26, 27]. In addition, the short and long-term consequences of UAS are not fully known [24, 27]. Similarly, in a meta-analysis, it was stated that adding a UAS when performing fURS should not be a systematic step, and this decision should be made on a patient-specific basis [28]. So, we did not use the UAS in Group 1 due to the large diameter of disposable fURS. Moreover, we have also not used the UAS the majority of patients in Group 2 (27.1%). Also, we have not forced for the placement of UAS, and the time of UAS replacement did not exceed a few minutes. So, we think that using UAS could not significantly affect the operative time in our study.
Urinary tract infection and sepsis can be seen less, since the procedure is performed with sterile instruments in procedures performed with disposable instruments [29]. However, in our study, no significant difference was found in both groups in terms of infective complications. The underlying reason could be that the reusable device is used on two patients a day.
In addition to the fact that our clinic is tertiary health center in our region, frequent referral of patients is also another factor with an impact on patient numbers. In the present study, the results more standardized since the fURS were performed by the same surgical team in almost the same period and with surgeons who have had similar surgical experience. In addition, the selection of patients from the same demographic region is one of the factors affecting the cohort to be more homogeneous. However, one of the main points that should not be forgotten is that randomized controlled studies to compare disposable and fURS are necessary.
The recently added Moses technology and TFL has higher efficiency and lower retropulsion rate during the stone fragmentation [30, 31]. Also laser ablation and surgery time are shorter than Ho:YAG lasers in vivo and in vitro studies [31, 32]. Although we have used 30-W holmium laser in our study, it is obvious that the operative time and SFR would be better by new laser technologies, in the future.
The present study has some inherent limitations. First, the limitations of the study that it is a single-center study. Thus, the number of patients is not sufficient to generalize to the whole population. Second, cost-effectiveness factors could not consider in this study. Third, we evaluated only lower pole stones. Despite these limitations, this present study provides important findings on the efficiency of disposable and reusable URS in the treatment of lower pole renal stones.
Conclusion
The findings of the present study indicate that disposable fURS is a more advantageous technique due to qualities such as a shorter operative time in cases with increased stone volume (> 10 mm sized), and multiple stones. In the treatment of lower pole stones the use of disposable fURS present an effective alternative to reusable fURS commonly used in urological interventions.
Availability of data and material
Data are available on request.
References
Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M et al (2016) EAU guidelines on interventional treatment for urolithiasis. EurUrol 69(3):475–482
Doizi S, Traxer O (2018) Flexible ureteroscopy: technique, tips and tricks. Urolithiasis 46(1):47–58
Elbahnasy AM, Clayman RV, Shalhav AL, Hoenig DM, Chandhoke P, Lingeman JE et al (1998) Lower-pole caliceal stone clearance after shockwave lithotripsy, percutaneous nephrolithotomy, and flexible ureteroscopy: impact of radiographic spatial anatomy. J Endourol 12(2):113–119
Fan J, Zhang T, Zhu W, Gurioli A, Ketegwe IR, Zeng G (2019) The role of super-mini percutaneous nephrolithotomy (SMP) in the treatment of symptomatic lower pole renal stones (LPSs) after the failure of shockwave lithotripsy (SWL) or retrograde intrarenal surgery (RIRS). Urolithiasis 47(3):297–301
Karim SS, Hanna L, Geraghty R, Somani BK (2019) Role of pelvicalyceal anatomy in the outcomes of retrograde intrarenal surgery (RIRS) for lower pole stones: outcomes with a systematic review of literature. Urolithiasis 48(3):263–270
Salvadó JA, Cabello JM, Moreno S, Cabello R, Olivares R, Velasco A (2019) Endoscopic treatment of lower pole stones: is a disposable ureteroscope preferable? Results of a prospective case-control study. Cent Eur J Urol 72(3):280
Davis N, Quinlan M, Browne C, Bhatt N, Manecksha RP, D’Arcy F et al (2018) Single-use flexible ureteropyeloscopy: a systematic review. World J Urol 36(4):529–536
Mager R, Kurosch M, Höfner T, Frees S, Haferkamp A, Neisius A (2018) Clinical outcomes and costs of reusable and single-use flexible ureterorenoscopes: a prospective cohort study. Urolithiasis 46(6):587–593
Ozimek T, Schneider MH, Hupe MC, Wiessmeyer JR, Cordes J, Chlosta PL et al (2017) Retrospective cost analysis of a single-center reusable flexible ureterorenoscopy program: a comparative cost simulation of disposable fURS as an alternative. J Endourol 31(12):1226–1230
Doizi S, Kamphuis G, Giusti G, Andreassen KH, Knoll T, Osther PJ et al (2017) First clinical evaluation of a new single-use flexible ureteroscope (LithoVueTM): a European prospective multicentric feasibility study. World J Urol 35(5):809–818
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205
Donaldson JF, Lardas M, Scrimgeour D, Stewart F, MacLennan S, Lam TB et al (2015) Systematic review and meta-analysis of the clinical effectiveness of shock wave lithotripsy, retrograde intrarenal surgery, and percutaneous nephrolithotomy for lower-pole renal stones. EurUrol 67(4):612–616
Junbo L, Yugen L, Guo J, Jing H, Ruichao Y, Tao W (2019) Retrograde intrarenal surgery vs. percutaneous nephrolithotomy vs. extracorporeal shock wave lithotripsy for lower pole renal stones 10–20 mm: a meta-analysis and systematic review. Urol J. 16(2):97–106
Singh BP, Prakash J, Sankhwar SN, Dhakad U, Sankhwar PL, Goel A et al (2014) Retrograde intrarenal surgery vs extracorporeal shock wave lithotripsy for intermediate size inferior pole calculi: a prospective assessment of objective and subjective outcomes. Urology 83(5):1016–1022
Jessen JP, Honeck P, Knoll T, Wendt-Nordahl G (2014) Flexible ureterorenoscopy for lower pole stones: influence of the collecting system’s anatomy. J Endourol 28(2):146–151
Knudsen B, Miyaoka R, Shah K, Holden T, Turk TM, Pedro RN et al (2010) Durability of the next-generation flexible fiberopticureteroscopes: a randomized prospective multi-institutional clinical trial. Urology 75(3):534–538
Somani BK, Al-Qahtani SM, de Medina SDG, Traxer O (2013) Outcomes of flexible ureterorenoscopy and laser fragmentation for renal stones: comparison between digital and conventional ureteroscope. Urology 82(5):1017–1019
Tosoian JJ, Ludwig W, Sopko N, Mullins JK, Matlaga BR (2015) The effect of repair costs on the profitability of a ureteroscopy program. J Endourol 29(4):406–409
Legemate JD, Kamphuis GM, Freund JE, Baard J, Zanetti SP, Catellani M et al (2019) Durability of flexible ureteroscopes: a prospective evaluation of longevity, the factors that affect it, and damage mechanisms. Euro Urol focus 5(6):1105–1111
Usawachintachit M, Isaacson DS, Taguchi K, Tzou DT, Hsi RS, Sherer BA et al (2017) A prospective case–control study comparing LithoVue, a single-use, flexible disposable ureteroscope, with flexible, reusable fiber-optic ureteroscopes. J Endourol 31(5):468–475
Martin CJ, McAdams SB, Abdul-Muhsin H, Lim VM, Nunez-Nateras R, Tyson MD et al (2017) The economic implications of a reusable flexible digital ureteroscope: a cost-benefit analysis. J Urol 197(3):730–735
Salvadó JA, Olivares R, Cabello JM, Cabello R, Moreno S, Pfeifer J et al (2018) Retrograde intrarenal surgery using the single–use flexible ureteroscopeUscope 3022 (PusenTM): evaluation of clinical results. Cent Eur J Urol 71(2):202
Deininger S, Haberstock L, Kruck S, Neumann E, da Costa IA, Todenhöfer T et al (2018) Single-use versus reusable ureterorenoscopes for retrograde intrarenal surgery (RIRS): systematic comparative analysis of physical and optical properties in three different devices. World J Urol 36(12):2059–2063
Traxer O, Thomas A (2013) Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal surgery. J Urol 189(2):580–584
Donaldson JF, Ruhayel Y, Skolarikos A, MacLennan S, Yuan Y, Shepherd R et al (2019) Treatment of bladder stones in adults and children: a systematic review and meta-analysis on behalf of the European Association of Urology Urolithiasis Guideline Panel. EurUrol 76(3):352–367
Miernik A, Wilhelm K, Ardelt PU, Adams F, Kuehhas FE, Schoenthaler M (2012) Standardized flexible ureteroscopic technique to improve stone-free rates. Urology 80(6):1198–1202
Lildal SK, Sørensen FB, Andreassen KH, Christiansen FE, Jung H, Pedersen MR et al (2017) Histopathological correlations to ureteral lesions visualized during ureteroscopy. World J Urol 35(10):1489–1496
De Coninck V, Keller EX, Rodríguez-Monsalve M, Audouin M, Doizi S, Traxer O (2018) Systematic review of ureteral access sheaths: facts and myths. BJU Int 122(6):959–969
Carlos EC, Li J, Young BJ, Radvak D, Wollin DA, Winship BB et al (2019) Let’s get to the point: comparing insertion characteristics and scope damage of flat-tip and ball-tip holmium laser fibers. J Endourol 33(1):22–26
Enikeev D, Shariat SF, Taratkin M, Glybochko P (2020) The changing role of lasers in urologic surgery. CurrOpinUrol 30(1):24–29
Dymov A, Rapoport L, Enikeev D, Tsarichenko D, Sorokin N, Proskura A et al (2019) Prospective clinical study on superpulse thulium fiber laser: Initial analysis of optimal laser settings. EurUrolSuppl 18(1):e500
Aldoukhi AH, Black KM, Hall TL, Roberts WW, Ghani KR (2020) Frequency threshold for ablation during holmium laser lithotripsy: how high can you go? J Endourol 34(10):1075–1081
Funding
The authors declare that this work has not received any funding.
Author information
Authors and Affiliations
Contributions
YEG: Protocol/project development; data collection or management; manuscript writing/editing; critical revision of the manuscript; supervision; approval of the final manuscript. MSO: Protocol/project development; data collection or management; data analysis; manuscript writing/editing; critical revision of the manuscript; supervision; approval of the final manuscript. MTK: data collection or management; manuscript writing/editing; critical revision of the manuscript; administrative, technical, or material support; approval of the final manuscript. HHT: data collection or management; manuscript writing/editing; critical revision of the manuscript; administrative, technical, or material support; approval of the final manuscript. EG: data collection or management; manuscript writing/editing; critical revision of the manuscript; administrative, technical, or material support; and approval of the final manuscript. AA: data collection or management; manuscript writing/editing; critical revision of the manuscript; administrative, technical, or material support; approval of the final manuscript. MGS: protocol/project development; data collection or management; data analysis; manuscript writing/editing; critical revision of the manuscript; approval of the final manuscript. GK: protocol/project development; data collection or management; data analysis; manuscript writing/editing; critical revision of the manuscript; approval of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval and informed consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The analysis and data collection were performed following the written informed consent was obtained from all patients. The institutional human research ethics committee approved the protocol enumareted as 2020/2657 (Necmettin Erbakan University, Meram Medical Faculty Ethics Committee).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Göger, Y.E., Özkent, M.S., Kılınç, M.T. et al. Efficiency of retrograde intrarenal surgery in lower pole stones: disposable flexible ureterorenoscope or reusable flexible ureterorenoscope?. World J Urol 39, 3643–3650 (2021). https://doi.org/10.1007/s00345-021-03656-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-021-03656-y