Abstract
Purpose
To examine the effect of marital status and gender on stage at diagnosis, tumor grade, treatment type and cancer specific mortality (CSM) in patients with localized renal cell carcinoma (RCC).
Methods
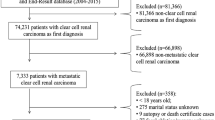
Within Surveillance, Epidemiology, and End Results registry (2001–2013), we identified 57,700 patients with T1–2 N0 M0 RCC. Logistic regression and competing-risks regression models tested the effect of marital status and gender on stage, tumor grade, treatment type and cancer specific mortality (CSM).
Results
Of all patients, 8.8, 10.6 and 14.8% were, respectively, widowed, separated/divorced and never married. The three categories accounted for 3.9, 9.0 and 14.9% of males (35,641) and for 16.7, 13.1 and 14.7% of females (22,059). Widowed (OR 1.13, p = 0.04), separated/divorced (OR 1.16, p = 0.02) and never married status (OR 1.38, p < 0.001) predisposed to higher rate of no surgical treatment. Widowed (HR 1.32, p < 0.001) and separated/divorced (HR 1.32, p < 0.001) status predisposed to higher CSM. Male gender predisposed to higher T-stage (OR 1.12, p < 0.001), higher tumor grade (OR 1.35, p < 0.001), no surgical treatment (OR 1.23, p < 0.001) and higher CSM (1.13, p = 0.01). Interaction tests between gender and marital status failed to reach independent predictor status in all analyses.
Conclusions
Male patients are at higher risk of less favorable baseline characteristics. Additionally, male, widowed and separated/divorced patients exhibit worse cancer control outcomes after treatment for T1–2 N0 M0 RCC. These observations indicate the need of more focused attention to those patients prior to, as well as after treatment for localized RCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unmarried status, such as widowed, separated/divorced and never married, represent an adverse predictor of stage and/or cancer control outcomes in various urological malignancies, such as prostate and bladder cancer [1, 2], as well as in non-urological cancers [3].
However, to date no study examined the effect of marital status and gender on stage, tumor grade, treatment type and cancer specific mortality (CSM) in patients with localized non-metastatic RCC. To address this void, we examined these risk factors in a comprehensive analysis within a contemporary, population-based cohort. We also hypothesized that an interaction may exist between gender and marital status.
Methods
Data source and study population
The study cohort consisted of individuals diagnosed with T1–2 N0 M0 RCC (International Classification of Disease for Oncology C64.9) from Surveillance, Epidemiology, and End Results (SEER) database (2001–2013).
We focused on patients with renal parenchymal tumors aged ≥18-years-old with histologically confirmed RCC. Death certificate only, autopsy cases and bilateral tumors were removed from the analysis. Included histological subtypes were: clear cell RCC (ccRCC), papillary, chromophobe, sarcomatoid, cyst-associated RCC, collecting duct carcinoma and any RCC. Papillary and chromophobe tumors were grouped as non-ccRCC; while sarcomatoid, cyst-associated RCC, collecting duct carcinoma and any RCC were grouped as “other”. Finally, patients with missing data on tumor stage, tumor size, tumor grade, treatment type and marital status were excluded.
Variables definition
Marital status was coded as married, widowed, separated/divorced and never married according to SEER database categories [4]. Other variables consisted of gender, age categories (18–49, 50–64, 65–74, 75–84, ≥85), race (white, black, other), T-stage (T1, T2), histologic subtype (ccRCC, non-ccRCC, other RCC), tumor grade (G1/G2, G3/G4), treatment type (no-surgery, surgery), year of diagnosis (2001–2008, 2009–2013) and socio-economic (SES) status [1, 5]. CSM was defined according to SEER mortality code. All other deaths were considered as other-cause mortality (OCM).
Statistical analysis
Descriptive statistics relied on tests of means and proportions and used the Chi-square for categorical and the t test for continuous variables. Five sets of analyses were performed. First, we evaluated the temporal trends of marital status, defined as widowed, separated/divorced and never married. To quantify temporal trends, we relied on annual percentage change (APC) with the least squares linear regression. Since differences may exist between males and females, the analyses were stratified according to gender.
Second, we examined the effect of marital status and gender on distribution of T-stage (T2 vs. T1), tumor grade (G3/G4 vs. G1/G2) and treatment type (no-surgery vs. surgery) using multivariable logistic regression models (LRMs). Covariates in multivariable LRMs consisted of marital status, gender, age, year of diagnosis, race, socio-economic status, histologic subtypes, as well as T-stage, tumor grade and treatment type when appropriate.
Third, we examined the effect of marital status and gender on CSM using competing-risks regression (CRR) models [6]. Multivariable CRR models accounted for the effect of OCM to provide the most unbiased estimate of CSM, after controlling for all covariates.
Fourth, interaction tests focused on the potential combined effect of marital status and gender in all LRMs and CRR models. Fifth, since ccRCC may behave differently from other histologic subtype, we relied on subgroup analyses that focused on ccRCC. Here, we repeated LRMs and CRR models, as previously described. Finally, we repeated all five steps of the analyses using a simplified coding of marital status. Specifically, married patients were compared to the combined category of separated/divorces, widowed and never married (unmarried).
All statistical tests were two-sided. The level of significance was set at p < 0.05. Analyses were performed using the R software environment for statistical computing and graphics (version 3.3.2; http://www.r-project.org/).
Results
Descriptive analyses and trends over time
We identified 57,700 patients with T1–2 N0 M0 RCC. Median age at diagnosis was 61 years (IQR 52–73). Majority were married (65.8%), male (61.8%), Caucasian (81.9%) and of high SES (52.4%). Most harbored T1 stage (84.9%), tumor grade G1/G2 (73.7%) and ccRCC (62.6%). Virtually, all underwent surgery (94.9%). Of all, 8.8, 10.6 and 14.8% were widowed, separated/divorced and never married. These three categories respectively accounted for, 3.9, 9.0 and 14.9% of males (35,641); and respectively for, 16.7, 13.1 and 14.7% of females (22,059) (Table 1). Temporal trends (2001–2013) revealed that in males, the proportion of separated/divorced increased from 5.4 to 9.7% (APC +2.5%, CI 1.1–3.9, p = 0.005), as well as the proportion of never married increased from 12.8 to 16.1% (APC +2.5%, CI 2.0–2.9, p < 0.001). Conversely, the proportion of widowed was stable: 3.9–2.6% (APC −1.3%, CI −2.9 to 0.4, p = 0.2). In females, no significant changes in proportions of individuals within examined marital status categories were recorded over time. Specifically, between 2001 and 2013 separated/divorced ranged from 11.0 to 13.7% (APC 0.6%, CI −0.6 to 1.8, p = 0.4), never married ranged from 12.9 to 17.8% (APC 2.3%, CI −0.1 to 4.7, p = 0.08) and widowed ranged from 17.8 to 13.8% (APC −1.4%, CI −2.8 to 0.1, p = 0.1).
The effect of marital status and gender on stage, grade and treatment type
In multivariable LRMs predicting pathological stage T2 vs. T1, marital status only showed an increased risk in never married patients with ccRCC histology (OR 1.11, CI 1.02–1.21; p = 0.02). Male gender predicted higher risk of T2 stage in the entire cohort (OR 1.12, CI 1.07–1.18; p < 0.001), as well as in the ccRCC subgroup (OR 1.14, CI 1.07–1.21; p < 0.001).
In multivariable LRMs predicting tumor grade G3/G4 vs. G1/G2, marital status failed to show an increased risk of tumor grade G3/G4. Male gender predicted higher risk of tumor grade G3/G4 in the entire cohort (OR 1.35, CI 1.30–1.41; p < 0.001), as well as in the ccRCC subgroup (OR 1.48, CI 1.40–1.55; p < 0.001).
In multivariable LRMs predicting treatment type, no-surgery vs. surgery, marital status showed an increased risk in widowed (OR 1.13, CI 1.00–1.28; p = 0.04), separated/divorced (OR 1.16, CI 1.02–1.32; p = 0.02) and never married (OR 1.38, CI 1.23–1.54; p < 0.001) patients. However, in the ccRCC subgroup, only never married status showed higher risk of no-surgery treatment type (OR 1.24, CI 1.08–1.44; p < 0.001). Male gender also predicted higher risk for no-surgery treatment type in the entire cohort (1.23, CI 1.13–1.33; p < 0.001), as well as in the ccRCC subgroup (1.17, CI 1.06–1.29; p = 0.002) (Table 2).
Virtually the same results were recorded for the combined category of unmarried predicting the rates of T2 stage (OR 1.05, p = 0.07), G3/G4 (OR 1.00, p = 0.8) and no-surgery treatment type (OR 1.23, p < 0.001) in the entire cohort, as well for the same three endpoints in ccRCC subgroup: (OR 1.07, p = 0.04), (OR 0.99, p = 0.9), (OR 1.16, p = 0.004).
The effect of marital status and gender on CSM
During the study period, a total of 6062 deaths were recorded in the entire cohort. Of those, 62.8% were OCM. Similarly, in the ccRCC subgroup a total of 3572 deaths were recorded. Of those 63.1% were OCM.
In multivariable CRR models, after accounting for OCM, widowed (HR 1.32, CI 1.15–1.52; p < 0.001), separated/divorced (HR 1.32, CI 1.15–1.51; p < 0.001) status and male gender (HR 1.13, CI 1.03–1.23; p = 0.01) were associated with higher CSM, but not never married status (HR 1.12, CI 0.98–1.28; p = 0.09) (Table 3).
Additionally, established predictors such as T2-stage (HR 3.46, CI 3.17–3.77; p < 0.001), tumor grade G3/G4 (HR 2.02, CI 1.85–2.20; p < 0.001) and no surgical treatment (HR 1.48, CI 1.22–1.81; p < 0.001) were also associated with higher CSM. All analyses were repeated in the ccRCC subgroup and yielded virtually the same results. Virtually the same results were recorded for the combined category of unmarried predicting the rates of CSM (HR 1.24, p < 0.001) in the entire cohort, as well as in the ccRCC subgroup (HR 1.25, p < 0.001).
Interaction tests between marital status and gender
Interaction tests that focused on the potential combined effect of gender and marital status failed to reach independent predictor status in LRMs and in CRR models, in the entire cohort and in the ccRCC subgroup.
Discussion
Widowed, separated/divorced and never married patients are known for more unfavorable outcomes in several cancers, other than RCC [1,2,3]. To the best of our knowledge despite rich literature focusing on biological outcomes determinants such as stage, grade and even molecular tumor make-up [7, 8], no study examined marital status and gender effect on T1–2 N0 M0 RCC in a comprehensive analysis. We hypothesized that marital status and gender may affect stage, tumor grade, treatment modality and CSM. Moreover, we hypothesized that an interaction may exist between gender and marital status.
Our results showed several important observations. First, marital status defined as widowed, separated/divorced and never married affected treatment type. Specifically, it conferred higher risk of no surgical treatment. Second, marital status showed no increased risk for higher T-stage and tumor grade at presentation. The exception consisted of never married status that increased the risk of T2 vs. T1 stage in the ccRCC subgroup. Third, marital status defined as widowed or separated/divorced conferred higher CSM risk, even after accounting for OCM. Fourth, when marital status was dichotomized between married and unmarried patients (separated/divorced, widowed and never married), unmarried status maintained the same effect on all examined endpoints. Fifth, similar to marital status, male gender invariably conferred higher risk of no surgical treatment, but also indicated higher risk of higher T-stage, higher tumor grade and higher CSM. Sixth, despite the existence of increased risk related to specific marital status categories and according to male gender, formal testing of the interaction between these two risk variables failed to demonstrate that their combined effect accounts for more than just the sum of their individual effects. In consequence, the effects of maleness and marital status do not require being multiplied by another in risk assessment.
These observations indicate that widowed, separated/divorced or simply all unmarried patients, as well as male patients deserve more focused attention prior to, as well as after treatment for localized RCC. This suggestion is based on the predisposing effects of marital status and gender towards less favorable stage, tumor grade and cancer control outcomes.
It is noteworthy that only a small proportion of male patients were widowed (3.9%) and a larger proportion were separated/divorced (9.0%). In consequence, the combination of these two categories resulted of 12.9% of male patients treated for localized RCC that deserve such particular attention.
It is also noteworthy, that the proportion of widowed as well as, separated/divorced patients differs between males and females. In females, the rates of widowed (16.7%) and separated/divorced (13.1%) were substantially higher than in males: 3.9 and 9.0%, respectively. In consequence, in females, marital status predisposes a larger proportion of patients to less favorable post-treatment cancer control outcomes.
The rationale for worse disease characteristics at presentation, higher rates of no surgical treatment and worse cancer control outcomes according marital status and gender have been also examined in malignances other than RCC. Differences were shown between married and unmarried patients regarding treatment type [1, 3], access to care [3], and social support [2]. Moreover, married patients might be better capable of managing distresses secondary to cancer diagnosis [3]. Additionally, differences in sexual hormone levels and their effect on immune function, as well as differences in inflammatory response between male and females might also contribute [9, 10].
To the best of our knowledge, no other investigators addressed the effect of marital status in localized RCC, in an equally comprehensive fashion. Partial analyses were performed in smaller and more historical cohorts by Hallenthal et al. [11]. They found that married patients are more likely to undergo nephrectomy [11]. Similarly, Trudeau et al. showed that male gender and unmarried status were associated with lower access to local tumor ablation [12]. Others specifically addressed the effect of marital status in prostate [1], bladder [2], liver [4] and colorectal [13] cancers.
In a recent SEER database analysis, investigators focused on ten leading causes of cancer-related deaths in the United States. Those did not include RCC. The results showed significantly higher risk of metastases, under-treatment and CSM in unmarried patients [3].
Similarly, smaller scale and more historical analyses examined gender in RCC. Rampersaud et al. described lower risk of advanced RCC and CSM in women [14]. Kates et al. showed higher risk of non-localized disease, in males with small renal masses (≤3 cm) [15]. Finally, the Collaborative Research on Renal Neoplasms Association (CORONA) database reported improved survival in females [16].
To the best of our knowledge, our analysis represents the first report on marital status in which CRR models were applied. This step allows to control for the confounding effect of OCM, that represent a particularly important competing-risk in patients with T1–2 N0 M0 RCC. Indeed, in our analysis 62.8% of mortalities represented OCM events. Such elevated proportion of OCM validates the need for CRR methodology. Moreover, the use of CRR obviates the need for adjustment for comorbidities that may culminate in OCM.
Several limitations apply to this study. First, outside of the SEER database, a different distribution of marital status may exist and our findings may not apply to patients that differ from the SEER database population. Second, marital status was recorded at diagnosis and may change during the disease course. Third, other social characteristics, such as relationships that modify marital status cannot be investigated in SEER database, since the database relies on predetermined marital status definitions. Fourth, all the limitations related to the retrospective nature of the SEER database apply to this, as well as all other SEER database or population-based analyses. Fifth, we exclusively focused on patients with T1–2 N0 M0 stages to avoid the effects associated with locally advanced or metastatic disease on CSM that leave little if any role for marital status or gender or other sociodemographic aspects.
Conclusion
Male patients are at higher risk of less favorable baseline characteristics. Additionally, male, widowed and separated/divorced patients exhibit worse cancer control outcomes after treatment for T1–2N0M0 RCC. These observations indicate the need of more focused attention to those patients prior to, as well as after treatment for localized RCC.
References
Abdollah F, Sun M, Thuret R et al (2011) The effect of marital status on stage and survival of prostate cancer patients treated with radical prostatectomy: a population-based study. Cancer Causes Control CCC 22:1085–1095. doi:10.1007/s10552-011-9784-x
Sammon JD, Morgan M, Djahangirian O et al (2012) Marital status: a gender-independent risk factor for poorer survival after radical cystectomy. BJU Int 110:1301–1309. doi:10.1111/j.1464-410X.2012.10993.x
Aizer AA, Chen M-H, McCarthy EP et al (2013) Marital status and survival in patients with cancer. J Clin Oncol 31:3869–3876. doi:10.1200/JCO.2013.49.6489
He X-K, Lin Z-H, Qian Y et al (2016) Marital status and survival in patients with primary liver cancer. Oncotarget. doi:10.18632/oncotarget.11066
Du XL, Fang S, Coker AL et al (2006) Racial disparity and socioeconomic status in association with survival in older men with local/regional stage prostate carcinoma: findings from a large community-based cohort. Cancer 106:1276–1285. doi:10.1002/cncr.21732
Scrucca L, Santucci A, Aversa F (2010) Regression modeling of competing risk using R: an in depth guide for clinicians. Bone Marrow Transplant 45:1388–1395. doi:10.1038/bmt.2009.359
Sun M, Shariat SF, Cheng C et al (2011) Prognostic factors and predictive models in renal cell carcinoma: a contemporary review. Eur Urol 60:644–661. doi:10.1016/j.eururo.2011.06.041
Karakiewicz PI, Briganti A, Chun FK-H et al (2007) Multi-institutional validation of a new renal cancer-specific survival nomogram. J Clin Oncol 25:1316–1322. doi:10.1200/JCO.2006.06.1218
McArdle CS, McMillan DC, Hole DJ (2003) Male gender adversely affects survival following surgery for colorectal cancer. Br J Surg 90:711–715. doi:10.1002/bjs.4098
de Perrot M, Licker M, Bouchardy C et al (2000) Sex differences in presentation, management, and prognosis of patients with non-small cell lung carcinoma. J Thorac Cardiovasc Surg 119:21–26. doi:10.1016/S0022-5223(00)70213-3
Hellenthal NJ, Chamie K, Ramirez ML, deVere White RW (2009) Sociodemographic factors associated with nephrectomy in patients with metastatic renal cell carcinoma. J Urol 181:1013–1018. doi:10.1016/j.juro.2008.10.159
Trudeau V, Larcher A, Sun M et al (2016) Sociodemographic disparities in the nonoperative management of small renal masses. Clin Genitourin Cancer 14:177–182. doi:10.1016/j.clgc.2015.10.011
Li Q, Gan L, Liang L et al (2015) The influence of marital status on stage at diagnosis and survival of patients with colorectal cancer. Oncotarget 6:7339–7347. doi:10.18632/oncotarget.3129
Rampersaud EN, Klatte T, Bass G et al (2014) The effect of gender and age on kidney cancer survival: younger age is an independent prognostic factor in women with renal cell carcinoma. Urol Oncol 32:30. doi:10.1016/j.urolonc.2012.10.012
Kates M, Korets R, Sadeghi N et al (2012) Predictors of locally advanced and metastatic disease in patients with small renal masses. BJU Int 109:1463–1467. doi:10.1111/j.1464-410X.2011.10553.x
May M, Aziz A, Zigeuner R et al (2013) Gender differences in clinicopathological features and survival in surgically treated patients with renal cell carcinoma: an analysis of the multicenter CORONA database. World J Urol 31:1073–1080. doi:10.1007/s00345-013-1071-x
Author information
Authors and Affiliations
Contributions
Protocol/project development: Marchioni, Martel, Bandini and Karakiewicz. Data collection or management: Marchioni, Bandini, Pompe, Tian. Data analysis: Marchioni and Tian. Manuscript writing/editing: all authors. Karakiewicz is acknowledged for supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participant and/or animals and informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Marchioni, M., Martel, T., Bandini, M. et al. Marital status and gender affect stage, tumor grade, treatment type and cancer specific mortality in T1–2 N0 M0 renal cell carcinoma. World J Urol 35, 1899–1905 (2017). https://doi.org/10.1007/s00345-017-2082-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-017-2082-9