Abstract
Objective
To examine the effect of diagnosis year, defined as contemporary (2010–2014), intermediate (2006–2009) and historical (2001–2005) on cancer-specific mortality (CSM) in patients with metastatic renal cell carcinoma (mRCC).
Methods
Within Surveillance, Epidemiology, and End Results registry (2001–2014), we identified patients with mRCC. Cumulative incidence and competing risks regression (CRR) models examined CSM, after accounting for other-cause mortality. Finally, we performed subgroup analyses according to histological subtype: clear-cell mRCC (ccmRCC) versus non-ccmRCC.
Results
We identified 15,444 patients with mRCC. Of those, 41.0, 28.7 and 30.3% were diagnosed, respectively, in the contemporary, intermediate and historical years. Of all, 47.1, 5.3 and 47.6% were, respectively, ccmRCC, non-ccmRCC and other mRCC histological variants [sarcomatoid mRCC, cyst-associated mRCC, collecting duct carcinoma and mRCC not otherwise specified (NOS)]. Overall, 24-month CSM rates were, respectively, 61.0, 63.7 and 67.3% in contemporary, intermediate and historical patients. In all patients, multivariable CRR models exhibited higher CSM in intermediate (HR 1.11; p < 0.001) and historical patients (HR 1.24; p < 0.001) than in contemporary patients. Multivariable CRR models focusing on ccmRCC yielded virtually the same results. However, multivariable CRR models focusing on non-ccmRCC showed no CSM differences according to diagnosis year (all p ≥ 0.3).
Conclusion
The introduction of new therapeutic agents resulted in CSM-free survival improvement over study time. However, this effect exclusively applies to patients with ccmRCC, but not to those with non-ccmRCC. This observation is in agreement with established efficacy of systemic therapies for ccmRCC, but lesser efficacy of these agents for non-ccmRCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Until the advent of targeted therapies, metastatic renal cell carcinoma (mRCC) represented a lethal malignancy, with median survival of 12 months [1]. Before the introduction of targeted and immunotherapy agents, the only available molecules were interleukin-2 and interferon alpha. In 2005 and 2006, two novel targeted agents were Food and Drug Administration (FDA) approved for clear-cell mRCC (ccmRCC): sorafenib and sunitinib. Temsirolimus, an mTOR inhibitor, was introduced in 2007. Three additional agents were introduced in 2009: everolimus, bevacizumab and pazopanib. In 2012, axitinib was made available. Finally, in 2015 and 2016, three most recent agents, nivolumab, cabozantinib and lenvatinib, were introduced [2]. With novel therapies, overall survival (OS) improved according to several pivotal phase III studies [3,4,5].
Survival outcomes were also examined in population-based analyses. These studies showed better survival in more contemporary patients [6,7,8,9,10]. However, most of these studies focused on patients treated until 2010 [6,7,8,9]. Based on ongoing advancements with respect to available novel targeted therapies for mRCC [2], it may be postulated that the previously observed survival improvements may have become even more meaningful. Based on this hypothesis, we decided to re-examine cancer-specific mortality (CSM) in mRCC patients diagnosed until 2014, using the most contemporary version of the Surveillance, Epidemiology, and End Results (SEER) database. Moreover, we relied on competing risks regression (CRR) models to account for other-cause mortality (OCM) that is of importance, especially in the light of longer disease-free survival. Adjustment for OCM allows to maximally reduce the confounding effect of significant comorbidities that compete for OS, with CSM.
Methods
Data source and study population
Within the SEER database, we identified patients diagnosed with mRCC (International Classification of Disease for Oncology C64.9). We only included patients ≥ 18 years old, diagnosed between 2001 and 2014, with histologically confirmed mRCC. Death certificate only or autopsy cases and bilateral tumors were excluded. Histological subtypes were stratified as follows: ccmRCC (n = 7280), non-ccmRCC [papillary (n = 665) and chromophobe (n = 147)] and other mRCC histological variants [sarcomatoid mRCC (n = 1037), cyst-associated RCC (n = 9), collecting duct carcinoma: (n = 132) and mRCC not otherwise classified (NOS) (n = 6174)]. Patients without follow-up data were also excluded.
Variables definition
In the SEER database, detailed information on specific chemotherapy lines directed at mRCC is not available. In consequence, analyses that are stratified according to type or number of sequential treatment lines could not be completed. Despite this limitation, we still attempted to test for better survival in most contemporary patients. To accomplish this, diagnosis year was stratified into three intervals: contemporary (2010–2014), intermediate (2006–2009) and historical (2001–2005). Covariates consisted of age categories (≤ 49, 50–64, 65–74, 75–84, ≥ 85), gender, race (white, black, other), marital status [married, never married, separated/divorced/widowed (SDW), unknown], Fuhrman grade [11, 12] (G1/G2, G3/G4, Gx), treatment type (nephrectomy, no nephrectomy) and histological subtype (ccmRCC, non-ccmRCC, other mRCC). CSM was defined according to SEER mortality code. All other deaths were considered as OCM.
Statistical analysis
Descriptive statistics relied on tests of means and proportions and used the Chi-square for categorical and the t test for continuous variables. Three sets of analyses were performed. First, cumulative incidence plots depicted CSM rates after accounting for OCM [13, 14]. Second, CRR models examined the effect of diagnosis year on CSM [15]. Multivariable CRR models accounted for the effect of OCM to provide the most unbiased estimate of CSM, after controlling for all covariates. Third, subgroup analyses were performed according to histological subtype: ccmRCC and non-ccmRCC.
All statistical tests were two-sided. The level of significance was set at p < 0.05. Analyses were performed using the R software environment for statistical computing and graphics (version 3.3.2; http://www.r-project.org/).
Results
We identified 15,444 mRCC patients. Of those, 41.0, 28.7 and 30.3% were diagnosed, respectively, in contemporary, intermediate and historical diagnosis year intervals. The median follow-up was 8 (IQR 3–20) months. The median age at diagnosis was 63 years (IQR 55–72). The majority were male (68.6%), married (60.9%) and Caucasian (83.9%). Of all, 14.4, 37.8 and 47.8%, respectively, harbored Fuhrman grade G1/G2, G3/G4 and Gx. Overall, 47.1, 5.3 and 47.6% of patients had ccmRCC, non-ccmRCC and other mRCC histological variants. Overall, 47.6% underwent nephrectomy (Table 1).
During the study period, a total of 10,896 deaths were recorded. Of those, 6.9% were OCM events and accounted for, respectively, 6.9, 6.9 and 7.0% of all recorded deaths, respectively, in contemporary, intermediate and historical diagnosis years. These observations validate the importance of OCM and the need for OCM adjustment.
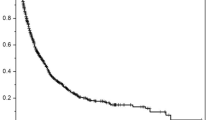
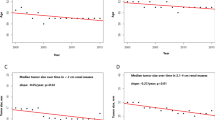
At 24 months, CSM rates were, respectively, 61.0, 63.7 and 67.3% in contemporary, intermediate and historical patients (Fig. 1). In multivariable CRR models, intermediate (HR 1.11, CI 1.06–1.17; p < 0.001) and historical patients (HR 1.24, CI 1.18–1.30; p < 0.001) had higher CSM rates than their contemporary counterparts (Table 2).
In ccmRCC subgroup analyses, the 24-month CSM rates were, respectively, 51.8, 54.7 and 57.5% in contemporary, intermediate and historical patients (Fig. 1). Here, in multivariable CRR models, intermediate (HR 1.12, CI 1.04–1.20; p < 0.001) and historical (HR 1.29, CI 1.19–1.39; p < 0.001) patients had higher CSM rates than their contemporary counterparts, to an even greater extent than recorded in all mRCC patients (Table 2).
In non-ccmRCC subgroup analyses, cumulative incidence and multivariable CRR models failed to reveal statistically significant differences between the three diagnosis year intervals (Fig. 1 and Table 2).
Discussion
Over the past decade, numerous novel therapies were introduced in the management of metastatic renal cell carcinoma and several novel molecules showed an improved progression-free survival [3, 4, 16,17,18,19,20,21]. Three molecules (cabozantinib, temsirolimus and nivolumab) demonstrated an improved OS in pivotal phase III trials [3,4,5].
These milestones resulted in an improved survival that was also recorded in population-based registry analyses [6,7,8,9,10]. However, virtually all such analyses only included patients diagnosed up to 2010 [6,7,8,9]. Based on this consideration, we hypothesized that more contemporary data might be capable of showing that survival continues to improve. To test our hypothesis, we relied on the most contemporary SEER database that provides patient follow-up until 2014. Our results showed two key observations.
First, we documented improved CSM-free survival according to three diagnosis year intervals. Specifically, we recorded a significant reduction in mortality rates over time. To the best of our knowledge, this is the first report of a dose–response effect according to diagnosis year. Specifically, we report highest survival in contemporary patients (2010–2014) that were not included in most of previous analyses [6,7,8,9]. The survival of contemporary patients exceeded that of intermediate diagnosis year patients, in a clinically meaningful and statistically significant fashion.
Second, our results corroborate an improved survival in contemporary and intermediate patients relative to their historical counterparts in subgroup analyses that focused on ccmRCC patients, but not in patients with non-ccmRCC. This observation corroborates treatment efficacy in ccmRCC but shows not improved survival trends in non-ccmRCC [22, 23].
Our results corroborate observations made in more historical series that also reported statistically significant survival improvements among patients with advanced or metastatic RCC, over the time. However, all such previous studies have limitations, of which the foremost is their historical nature [6,7,8,9,10]. Indeed, most studies relied on patients diagnosed up to 2010 [6,7,8,9]. In consequence, the effect of some of the FDA-approved agents, such as bevacizumab, everolimus, pazopanib and axitinib, could not be truly investigated, since these molecules were FDA approved as of 2009 or later [2]. This limitation was circumvented in our study since follow-up was available until December 2014.
Furthermore, two studies relied on January 2005 to define patients as contemporary [6, 8]. Such definition may not be ideal, since the first two targeted therapy molecules, sorafenib and sunitinib, were only FDA approved as of December 2005 [2]. In consequence, the vast majority of patients with 2005 diagnosis year truly represent pre-targeted therapy patients. In our study, we circumvented this potential misclassification error and relied on the date of January 2006 for inclusion into the intermediate diagnosis year category that defined early targeted therapy patients.
Additional limitations of previous studies consisted of broad inclusion criteria. Specifically, patients with locally advanced and patients with mRCC were included in three of such studies [7, 8, 10]. This may have resulted in inclusion of patients with T4M0 RCC. Such patients may show better survival than their M1 counterparts, and they represent a specific highly selected patient category [24, 25]. We circumvented this limitation and only included M1 patients in all our analyses.
Additionally, unlike previous studies, our study is the first to rely on CRR models that account for OCM. The latter allows to control for the confounding effect of OCM and obviates the need for adjustment for comorbidities that may culminate in OCM. Indeed, not all mRCC patients die of their disease. During the study period, 6.9% of deaths were OCM events, which accounted for, respectively, 6.9, 6.9 and 7.0% of all recorded deaths, respectively, in contemporary, intermediate and historical diagnosis year. In the presence of non-negligible OCM rate, the use of competing risks is strongly indicated [14, 15], as was done in the current study with the intent of maximally reducing the confounding effect of OCM that originates from significant comorbidities.
It is also noteworthy that we were able to identify a dose–response effect according to diagnosis year, where contemporary and intermediate diagnosis year intervals included patients who could be treated with targeted therapies. Our study is the first to confirm statistical significance of the dose–response effect, even in multivariable CRR models. In the most recent report, Pal et al. relied on the SEER-Medicare population (2006–2012) of 1245 patients versus 15,444 included in our study. In their report, lack of statistical significance was reported in OS, when contemporary patients were compared to historical patients in multivariable analysis (2006–2011 vs. 1994–2005). However, statistically significant differences in OS were identified, when patients diagnosed between 2010 and 2012 were compared to those diagnosed between 2006 and 2009, but only in univariable models that do not account for OCM [10]. Conversely, in our study we were able to show statistically significant survival differences also in multivariable CRR models.
It also warrants emphasis that our analysis only showed an improved survival over time in patients with ccmRCC. This finding is in agreement with prospective phase III trials that exclusively or predominantly focused on ccmRCC [26]. In phase III trials that included non-ccmRCC patients, the absolute survival duration was shorter in non-ccmRCC patients than in those with ccmRCC [22, 23].
Finally, a large proportion of our patients, classified in the SEER database as mRCC NOS, were included in other mRCC histological variants. In these patients, the exact histological subtype could have represented more aggressive variants or could have been misclassified. Moreover, if a central review had been performed, patients with mRCC NOS histology may have been classified as ccmRCC or non-ccmRCC, resulting in inclusion in those specific categories [27].
Several additional limitations apply to this study. First, the SEER database does not allow to ascertain the exact type of systemic therapy that was used. Moreover, it is unknown how many therapy lines were used and in which sequences such therapies were administered. Furthermore, most recent systemic agents, such as nivolumab, cabozantinib and lenvatinib, that were FDA approved after 2014 could not have affected the observed rates [2]. Additionally, adjustment could not be performed according to established stratification variables such as performance status. Also we could not stratify according to risk stratification tools used in reference publications, such as Motzer or Heng score [28, 29]. Furthermore, the variable defining the site of metastases was only made available in the SEER database as of 2010. For this reason, it was not possible to adjust for this covariate, despite the established effect of different metastatic sites on cancer survival, as well as on the known role of single versus multiple metastases in single versus multiple organs [30, 31]. Finally, all the limitations related to the retrospective nature of the SEER database apply to this, as well as all other SEER database or population-based analyses.
Conclusion
The introduction of new therapeutic agents resulted in CSM-free survival improvement over study time. However, this effect exclusively applies to patients with ccmRCC, but not to those with non-ccmRCC. This observation is in agreement with established efficacy of systemic therapies for ccmRCC but lesser efficacy of these agents for non-ccmRCC.
References
Motzer RJ, Bukowski RM (2006) Targeted therapy for metastatic renal cell carcinoma. J Clin Oncol 24(35):5601–5608. doi:10.1200/JCO.2006.08.5415
Modi PK, Farber NJ, Singer EA (2016) Precision oncology: identifying predictive biomarkers for the treatment of metastatic renal cell carcinoma. Transl Cancer Res 5(Suppl 1):S76–S80. doi:10.21037/tcr.2016.06.05
Choueiri TK, Escudier B, Powles T et al (2016) Cabozantinib versus everolimus in advanced renal cell carcinoma (METEOR): final results from a randomised, open-label, phase 3 trial. Lancet Oncol 17(7):917–927. doi:10.1016/S1470-2045(16)30107-3
Hudes G, Carducci M, Tomczak P et al (2007) Temsirolimus, interferon alfa, or both for advanced renal-cell carcinoma. N Engl J Med 356(22):2271–2281. doi:10.1056/NEJMoa066838
Motzer RJ, Escudier B, McDermott DF et al (2015) Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med 373(19):1803–1813. doi:10.1056/NEJMoa1510665
Pal SK, Nelson RA, Vogelzang N (2013) Disease-specific survival in de novo metastatic renal cell carcinoma in the cytokine and targeted therapy era. PLoS ONE 8(5):e63341. doi:10.1371/journal.pone.0063341
Li P, Wong Y-N, Armstrong K et al (2016) Survival among patients with advanced renal cell carcinoma in the pretargeted versus targeted therapy eras. Cancer Med 5(2):169–181. doi:10.1002/cam4.574
Vaishampayan U, Vankayala H, Vigneau FD et al (2014) The effect of targeted therapy on overall survival in advanced renal cancer: a study of the National Surveillance Epidemiology and End Results Registry Database. Clin Genitourin Cancer 12(2):124–129. doi:10.1016/j.clgc.2013.09.007
Macleod LC, Tykodi SS, Holt SK et al (2015) Trends in metastatic kidney cancer survival from the cytokine to the targeted therapy era. Urology 86(2):262–268. doi:10.1016/j.urology.2015.05.008
Pal SK, Ghate SR, Li N et al (2017) Real-world survival outcomes and prognostic factors among patients receiving first targeted therapy for advanced renal cell carcinoma: a SEER–Medicare Database Analysis. Clin Genitourin Cancer. doi:10.1016/j.clgc.2016.12.005
Sun M, Lughezzani G, Jeldres C et al (2009) A proposal for reclassification of the fuhrman grading system in patients with clear cell renal cell carcinoma. Eur Urol 56(5):775–781. doi:10.1016/j.eururo.2009.06.008
Fuhrman SA, Lasky LC, Limas C (1982) Prognostic significance of morphologic parameters in renal cell carcinoma. Am J Surg Pathol 6(7):655–663
Grunkemeier GL, Jin R, Eijkemans MJC, Takkenberg JJM (2007) Actual and actuarial probabilities of competing risks: apples and lemons. Ann Thorac Surg 83(5):1586–1592. doi:10.1016/j.athoracsur.2006.11.044
Zhang Z (2017) Survival analysis in the presence of competing risks. Ann Transl Med 5(3):47. doi:10.21037/atm.2016.08.62
Scrucca L, Santucci A, Aversa F (2010) Regression modeling of competing risk using R: an in depth guide for clinicians. Bone Marrow Transplant 45(9):1388–1395. doi:10.1038/bmt.2009.359
Escudier B, Eisen T, Stadler WM et al (2009) Sorafenib for treatment of renal cell carcinoma: final efficacy and safety results of the phase iii treatment approaches in renal cancer global evaluation trial. J Clin Oncol 27(20):3312–3318. doi:10.1200/JCO.2008.19.5511
Motzer RJ, Hutson TE, Tomczak P et al (2009) Overall survival and updated results for sunitinib compared with interferon alfa in patients with metastatic renal cell carcinoma. J Clin Oncol 27(22):3584–3590. doi:10.1200/JCO.2008.20.1293
Motzer RJ, Hutson TE, Cella D et al (2013) Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N Engl J Med 369(8):722–731. doi:10.1056/NEJMoa1303989
Motzer RJ, Escudier B, Tomczak P et al (2013) Axitinib versus sorafenib as second-line treatment for advanced renal cell carcinoma: overall survival analysis and updated results from a randomised phase 3 trial. Lancet Oncol 14(6):552–562. doi:10.1016/S1470-2045(13)70093-7
Escudier B, Bellmunt J, Négrier S et al (2010) Phase III trial of bevacizumab plus interferon alfa-2a in patients with metastatic renal cell carcinoma (AVOREN): final analysis of overall survival. J Clin Oncol 28(13):2144–2150. doi:10.1200/JCO.2009.26.7849
Motzer RJ, Escudier B, Oudard S et al (2010) Phase 3 trial of everolimus for metastatic renal cell carcinoma. Cancer 116(18):4256–4265. doi:10.1002/cncr.25219
Vera-Badillo FE, Templeton AJ, Duran I et al (2015) Systemic therapy for non-clear cell renal cell carcinomas: a systematic review and meta-analysis. Eur Urol 67(4):740–749. doi:10.1016/j.eururo.2014.05.010
Fernández-Pello S, Hofmann F, Tahbaz R et al (2017) A systematic review and meta-analysis comparing the effectiveness and adverse effects of different systemic treatments for non-clear cell renal cell carcinoma. Eur Urol 71(3):426–436. doi:10.1016/j.eururo.2016.11.020
Karakiewicz PI, Briganti A, Chun FK-H et al (2007) Multi-institutional validation of a new renal cancer-specific survival nomogram. J Clin Oncol 25(11):1316–1322. doi:10.1200/JCO.2006.06.1218
Cindolo L, Chiodini P, Brookman-May S et al (2013) Assessing the accuracy and generalizability of the preoperative and postoperative Karakiewicz nomograms for renal cell carcinoma: results from a multicentre European and US study. BJU Int 112(5):578–584. doi:10.1111/j.1464-410X.2012.11670.x
Sánchez P, Calvo E, Durán I (2011) Non-clear cell advanced kidney cancer: is there a gold standard? Anticancer Drugs 22(Suppl 1):S9–14. doi:10.1097/01.cad.0000390767.85658.83
Shuch B, Hofmann JN, Merino MJ et al (2014) Pathologic validation of renal cell carcinoma histology in the Surveillance, Epidemiology, and End Results program. Urol Oncol 32(1):23.e9–23.e13. doi:10.1016/j.urolonc.2012.08.011
Ljungberg B, Albiges L, Bex A et al (2017) EAU guidelines on renal cell carcinoma. http://uroweb.org/wp-content/uploads/10-Renal-Cell-Carcinoma_2017_web.pdf. Accessed 27 Feb 2017
Heng DYC, Xie W, Regan MM et al (2009) Prognostic factors for overall survival in patients with metastatic renal cell carcinoma treated with vascular endothelial growth factor-targeted agents: results from a large, multicenter study. J Clin Oncol 27(34):5794–5799. doi:10.1200/JCO.2008.21.4809
Capitanio U, Abdollah F, Matloob R et al (2013) Effect of number and location of distant metastases on renal cell carcinoma mortality in candidates for cytoreductive nephrectomy: implications for multimodal therapy. Int J Urol 20(6):572–579. doi:10.1111/iju.12004
Abdel-Rahman O (2017) Clinical correlates and prognostic value of different metastatic sites in metastatic renal cell carcinoma. Future Oncol. doi:10.2217/fon-2017-0175
Author information
Authors and Affiliations
Contributions
Marchioni, Bandini and Karakiewicz contributed to protocol/project development. Marchioni, Bandini, Pompe and Tian helped in data collection or management. Marchioni, Bandini and Tian analyzed the data. All authors wrote and edited the manuscript. Karakiewicz is acknowledged for supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study, formal consent is not required.
Human and animals rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Marchioni, M., Bandini, M., Pompe, R.S. et al. Survival of metastatic renal cell carcinoma patients continues to improve over time, even in targeted therapy era. Int Urol Nephrol 49, 2143–2149 (2017). https://doi.org/10.1007/s11255-017-1703-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-017-1703-y