Abstract
Purpose
No study has evaluated the prognostic impact of the age-adjusted Charlson comorbidity index (AACI) in those with renal cell carcinoma (RCC). This study aimed to evaluate the utility of the AACI for predicting long-term survival in patients with surgically treated non-metastatic clear cell RCC (ccRCC).
Methods
Data from 698 patients with non-metastatic ccRCC who underwent radical or partial nephrectomy as primary therapy from a multi-institutional Korean collaboration between 1988 and 2015 were retrospectively analyzed. Clinicopathological variables and survival outcomes of those with AACI scores ≤ 3 (n = 324), 4–5 (n = 292), and ≥ 6 (n = 82) were compared.
Results
Patients with a high AACI score were older and more likely to be female. They were also more likely to have diabetes or hypertension, a worse Eastern Cooperative Oncology Group performance status, and lower preoperative hemoglobin, albumin, serum calcium, and serum total cholesterol levels. Regarding pathologic features, a high AACI score was associated with advanced stage. Kaplan–Meier analyses revealed that AACI ≥ 6 was associated with shorter cancer-specific (log-rank test, P < 0.001) and overall survival (log-rank test, P < 0.001), but not with recurrence-free survival (log-rank test, P = 0.134). Multivariate Cox regression analyses identified an AACI score as an independent predictor of overall survival (hazard ratio, 6.870; 95% confidence interval, 2.049–23.031; P = 0.002). The AACI score was a better discriminator of overall survival than the Charlson comorbidity index score.
Conclusions
AACI scores may enable more tailored, individualized management strategies for patients with surgically treated non-metastatic ccRCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal cell carcinoma (RCC) accounts for 2–3% of all adult malignancies, and annual estimates of newly diagnosed cases have increased steadily over the last decade (King et al. 2014). RCC has a relatively poor prognosis due to lack of a major breakthrough with respect to primary treatment. Most (70%) patients have clinically localized disease at the time of diagnosis and surgical resection is the mainstay of treatment; however, 20–30% of patients develop metastatic disease after surgery (Motzer et al. 2017). Biologically, RCC ranges from indolent to highly lethal; therefore, treatment outcomes vary widely. Thus, there is an urgent need for prompt and accurate prognostic stratification. Currently, the most commonly used tools for predicting the outcome of RCC are the TNM staging system and nuclear grade (Ljungberg et al. 2019). However, survival of patients with the same stage and grade varies considerably (Escudier et al. 2016). Therefore, predicting prognosis based on pretreatment clinical variables rather than operative and pathological variables is important if we are to improve the prognosis and offer an optimal treatment strategy. Age and comorbidities are associated with overall and disease-specific outcomes for various cancers (Aziz et al. 2014; Dias-Santos et al. 2015; Suidan et al. 2015; Wu et al. 2015). Because RCC patients are likely to have substantial comorbidities due to advanced age at the time of diagnosis, it is important to explore the effects of pre-existing medical diseases on survival after definitive surgical treatment (Verhoest et al. 2007). Capturing information about comorbidities using validated instruments can improve preoperative evaluation by providing more accurate prognostic information.
The age-adjusted Charlson Comorbidity Index (AACI) score is a modified form of the Charlson comorbidity index (CCI); the former considers age as an additional index of comorbidity (Chang et al. 2016; Koppie et al. 2008; Santos Arrontes et al. 2008). The ACCI score has been used to predict survival and treatment options for various types of cancer, including gynecological and urological cancers such as prostate cancer and bladder cancer (Koppie et al. 2008; Park et al. 2018; Robbins et al. 2013; Suidan et al. 2015). Recent studies show that pre-existing comorbidities, as assessed by the CCI, are associated with poor overall survival in RCC (Ather and Nazim 2010; Santos Arrontes et al. 2008). However, the prognostic role of the AACI in RCC is unclear. The aim of the present study was to investigate the utility of the AACI score for predicting recurrence-free survival (RFS), cancer-specific survival (CSS), and overall survival (OS) in patients with surgically treated clear cell RCC (ccRCC).
Materials and methods
Study population and data collection
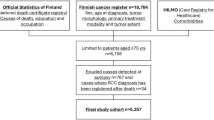
Between January 1988 and December 2015, demographic, surgical, and pathologic information from 7047 anonymous patients who underwent radical or partial nephrectomy as primary therapy for RCC at eight academic centers in Korea were collected retrospectively and pooled centrally. Approval for the study was obtained from the relevant institutional review boards. The study excluded patients with benign pathology, non-ccRCC, metastatic disease (regional or non-regional lymph nodes or distant metastases), bilateral synchronous tumors, hereditary forms of RCC (including hereditary papillary), von Hippel–Lindau and tuberous sclerosis syndromes, those with Wilms tumor, those aged < 18 years at the time of surgery, and those with insufficient data concerning their medical history. Consequently, 698 consecutive patients who were followed for ≥ 6 months after surgery for non-metastatic ccRCC were included in the final analysis.
Measurements
The CCI features 19 conditions that are assigned scores of 1, 2, 3, or 6 based upon disease severity (Santos Arrontes et al. 2008). A binomial value (present or absent) was assigned to 19 different comorbidities. The final score was calculated for each patient, taking into account all comorbid conditions present. The AACI score was calculated by summing the weighted comorbidities and age of each patient (Chang et al. 2016; Koppie et al. 2008). RCC was not considered when assessing the score, and any new medical conditions that developed after the date of surgical treatment were omitted. The distribution of comorbidities for all patients (based on the AACI score) is shown in Table 1.
Protocols used for surgery and follow-up
All surgical procedures were performed by skilled surgeons using standard techniques (Ljungberg et al. 2019; Motzer et al. 2017). Surgery was either open or laparoscopic. Lymph node dissection was performed for patients with clinical or radiologic evidence of lymphadenopathy, or at the surgeons’ discretion for patients deemed to be at high risk for occult nodal metastases at the time of nephrectomy. All surgical specimens were processed according to the standard pathologic procedures of each participating institution. Pathological staging was performed according to the 7th edition of the American Joint Committee on Cancer classification system and histological differentiation was graded according to the Fuhrman nuclear grading system (Edge and Compton 2010; Fuhrman et al. 1982). After surgery, each patient was monitored according to standard guidelines (Escudier et al. 2016). In general, patients were evaluated every 3–4 months for the first year following nephrectomy, and then every 6 months from the second through fifth years; patients without evidence of recurrent disease were monitored annually thereafter. Disease recurrence (based on clinical and radiographic findings) was defined as locoregional recurrence or as a newly identified distant metastasis. RFS was defined as the period between surgery and detection of recurrence or distant metastasis. Death was determined by reviewing medical records. Time to cancer-specific mortality was calculated as the time from surgery to the date of cancer-attributed mortality. Any patients who died without proof of metastasis or recurrence were collated as “overall mortality”.
Statistical analysis
Receiver operating characteristic curves were constructed to determine the AACI score cut-off values conferring optimal sensitivity and specificity for survival analysis. Patients were classified into three risk groups based on their AACI score: low (AACI ≤ 3), intermediate (AACI 4–5), and high (AACI ≥ 6). These cut-off was similar to previous study (Ho et al. 2017). Fisher’s exact test (categorical variables) and ANOVA with Bonferroni’s post hoc test (continuous variables) were used to compare clinical and pathological features between the three groups. The Kaplan–Meier method was used to estimate time to recurrence and cancer-specific death; differences were assessed using the log-rank test. To identify independent predictors of recurrence, CSS, and OS, a forward conditional Cox regression analysis was performed. Variables of P < 0.2 on univariate analysis included in the multivariate analysis. The ability of the CCI and AACI indices to predict OS was compared using the area under receiver operating curves. Differences were considered significant at P < 0.05, and all reported P values were two-sided. Analyses were performed using SPSS 24.0 software (IBM Corp., Armonk, NY, USA).
Ethics statement
The study complied with all applicable laws and regulations, good clinical practice, and ethical principles, as described in the Declaration of Helsinki. The study protocol was approved by the institutional review board of Chungbuk National University (Approval Number: GR2014-12-009). The requirement for informed consent was waived due to the retrospective nature of the study.
Results
Comparison of clinical, operative, and pathologic variables stratified according to the AACI score
Of the 698 surgically treated RCC patients, 324 (46.4%) had a low AACI score (AACI ≤ 3), 292 (41.8%) had a moderate score (AACI 4–5), and 82 (11.7%) had a high score (AACI ≥ 6). The demographic and clinical features stratified according to AACI group are shown in Table 2. Patients with a high score were older, more likely to be female, more likely to have diabetes or hypertension and a worse Eastern Cooperative Oncology Group performance status (ECOG-PS), and were more likely to have lower preoperative hemoglobin, albumin, serum calcium, and serum total cholesterol levels (each P < 0.05). Nephron-sparing surgery and minimal invasive surgery were more common in the low AACI group than in the moderate and high groups (both P < 0.05). Regarding pathologic features, a high AACI score was associated with advanced stage (P = 0.005). There were no significant differences between the groups with respect to tumor laterality, size, and nuclear grade (Table 3).
Ability of the AACI score to predict RFS, CSS, and OS among surgically treated patients with non-metastatic ccRCC
The median follow-up was 37 (interquartile range, 15–67 months) months for all patients. The impact of the AACI score on RFS was assessed in 611 patients with pathologically localized disease (pT1–2N0). During follow-up, recurrence was observed in 50 patients, and 15 and 40 patients died from RCC-attributable and all cause death, respectively. The relationship between the AACI category and RFS, CSS, and OS is illustrated by a Kaplan–Meier survival curve (Fig. 1). The AACI had no impact on RFS in patients with pathologically localized disease (log-rank test, P = 0.134) (Fig. 1a). An AACI score ≥ 6 was associated with shorter CSS and OS (log-rank test, P < 0.001) (Fig. 1b, c). Pairwise comparisons did not identify a significant difference in CSS between the low and moderate AACI groups (log-rank test, P = 0.767). Patients with a ACCI score ≥ 6 had a significantly shorter CSS than those with a low or moderate score (log-rank test, each P < 0.001) (Fig. 1b). Meanwhile, pairwise comparisons identified a significant difference in OS between the three groups (log-rank test: low vs. moderate, P = 0.021; low vs. high and moderate vs. high, each P < 0.005) (Fig. 1c). Kaplan–Meier analyses also exhibit significantly different CSS and OS between AACI groups after stratification based on the pathologic T stages (pT < 2 vs. ≥ 2) (log-rank test, each P < 0.05) (Supplementary Figure).
Kaplan–Meier survival curves showing a recurrence-free survival of patients with localized clear cell renal cell carcinoma (pT1–2), and b cancer-specific survival and c overall survival in patients with surgically treated clear cell renal cell carcinoma, according to the AACI score. AACI age-adjusted Charlson comorbidity index
Multivariate Cox regression analyses identified an AACI score as an independent predictor of overall survival (hazard ratio, 6.870; 95% confidence interval, 2.049–23.031; P = 0.002). Although significant by univariate analysis, the ACCI scores were not independent prognostic factors of CSS in the multivariate analysis (Tables 4 and 5).
Ability of the CCI and AACI indices to predict cancer-specific and overall survival
The CCI and AACI models both discriminated OS after surgery (P = 0.014 and P < 0.001, respectively). However, the AACI score was a better discriminator than the CCI score, with an area under the ROC curve of 0.726 versus 0.616 for OS, respectively (Fig. 2).
Receiver operating curve (ROC) showing the ability of the CCI and AACI indices to predict overall survival in patients with surgically treated clear cell renal cell carcinoma. CCI Charlson comorbidity index, AACI age-adjusted Charlson comorbidity index, AUC area under the ROC curve, CI confidence interval
Discussion
Here, we conducted a large, multi-institutional Korean collaborative study to assess the prognostic impact of the AACI for patients with surgically treated non-metastatic RCC. The results indicate that when the AACI score was an independent predictor of OS after nephrectomy. In addition, the AACI score was a better discriminator of OS than the original CCI score. To the best of our knowledge, this is the first study to evaluate the prognostic value of the AACI score for predicting long-term survival of patients with RCC.
Comorbidity and performance status indices are useful preoperative tools for estimating the risk of comorbidities; as such, they may guide decision-making regarding operative procedure or multimodal therapy approaches (Aziz et al. 2014; Søgaard et al. 2013). The most commonly used comorbidity indices in the literature are the CCI, the AACI, the American Society of Anesthesiologists Physical Status (ASA-PS), the Adult Comorbidity Evaluation-27 (ACE-27), the ECOG-PS, and the Karnofsky Performance Status scale (Extermann 2000; Kang et al. 2017). Previous studies show that comorbidities affect the prognosis of cancer patients (Islam et al. 2015); however, there is a lack of information about the prognostic impact of medical comorbidities on survival of patients with RCC. The ECOG-PS, ASA-PS, and ACE-27 are recognized as independent prognostic factors for OS or CSS in patients with RCC (Berger et al. 2008; de Cássio Zequi et al. 2010; Zisman et al. 2001). Recent studies report that high CCI values are associated with poor OS in RCC. For example, Arrontes et al. examined a surgical series of 192 ccRCC patients and found that those with localized RCC and a CCI > 2 showed a significantly lower OS then patients with a CCI ≤ 2 (Santos Arrontes et al. 2008). However, the CCI did not influence the survival of patients with locally advanced or metastatic ccRCC (Santos Arrontes et al. 2008). Another study by Ather et al. evaluated the effect of the CCI in 157 patients with primary RCC treated by nephrectomy (Ather and Nazim 2010). They found that the CCI was an independent predictor of OS, and was as reliable as tumor-specific variables such as pathologic stage and grade (Ather and Nazim 2010). A Danish population-based study by Jacobsen et al. used CCI scores to estimate the risk of 1- and 5-year mortality among patients with renal cancer (Lund et al. 2009). They found that 5-year mortality in those with a score of ≥ 3 was almost twofold higher, and that for those with a score of 1–2 was 1.2-fold higher, than that for those with no comorbidity (Lund et al. 2009). By contrast, Gettman and colleagues examined a cohort of surgically treated patients with tumor thrombus and noted that the CCI did not predict CSS (Gettman et al. 2003).
The AACI is a modified version of the CCI in that it considers age as an additional comorbidity index (Chang et al. 2016). The AACI score has been used to predict survival and treatment options for those with various types of cancer, including gastrointestinal, gynecological, and urological cancer (Dias-Santos et al. 2015; Koppie et al. 2008; Park et al. 2018; Robbins et al. 2013; Suidan et al. 2015; Wu et al. 2015). Using the AACI, Koppie and colleagues identified an association between age and comorbidity with respect to OS and disease‐specific survival in patients undergoing radical cystectomy for bladder cancer (Koppie et al. 2008). The authors noted that both age and comorbidity were associated with treatment selection (i.e., lymph‐node dissection or postoperative chemotherapy) and lower OS (Koppie et al. 2008). In addition, Park et al. investigated the efficacy of the AACI as a prognostic factor for very high risk prostate cancer patients following radical prostatectomy (Park et al. 2018). Competing risk regression analysis revealed that the AACI score was significantly associated with OS (Park et al. 2018). However, no study has examined the prognostic role of the AACI score in the context of RCC. Several studies support a prognostic role for age in patients with RCC. Previously, we reported the potential impact of age on clinicopathologic characteristics and survival of patients with surgically treated RCC. Although age was not an independent prognostic factor for CSS, old age at the time of diagnosis was closely related to unfavorable pathologic features and shorter CSS (Kang et al. 2016). Therefore, we hypothesized that the AACI is a better discriminator of RCC prognosis than the original CCI score because the former allows integration of both age and comorbidities. As expected, we found here that the AACI was a better discriminator of CSS and OS than the CCI score.
The present study is the first to suggest that the AACI score has a prognostic impact on OS of surgically treated non-metastatic ccRCC. This finding is in line with a recent study showing that a high CCI score is an independent predictor of poor OS in RCC. RCC is characterized by unique biological features; indeed, there is a close association between RCC and metabolic status. The prognostic role of immune–nutritional status has been researched extensively (Ko et al. 2013; Zheng et al. 2018). In this context, a compromised immune–nutritional status coupled with a preoperative medical commodity such as diabetes, liver or renal disease, or a tumor other than RCC, may account for poor OS in those with surgically treated non-metastatic ccRCC. In support of this hypothesis, we found that serum albumin as a marker of protein-energy and total cholesterol concentration as an indicator of a patient’s caloric reserves were significantly lower in those with a high AACI score.
This study has some limitations. First, it is a retrospective and multicentric study, meaning that the assessment of comorbidity may introduce bias. In addition, we included only patients who had undergone surgery; patients who were ineligible candidates for surgery due to high age and a high number of comorbidities were not included. This may have introduced selection bias; therefore, the cohort may not reflect all patients with RCC. Thus, a comprehensive cohort study that includes those with metastatic RCC and those ineligible for surgery is needed to confirm our hypothesis.
Conclusion
We demonstrate for the first time that AACI score was an independent predictor of OS in patients with surgically treated non-metastatic ccRCC. The AACI was a better discriminator of OS than the CCI score. Taken together, these results suggest that the AACI may provide additional prognostic information about patients with surgically treated ccRCC. For example, during preoperative evaluation, the AACI could prove useful for assessing the risk of mortality from cancer and as a tool to develop a more tailored, individualized management strategy.
References
Ather MH, Nazim SM (2010) Impact of Charlson’s comorbidity index on overall survival following tumor nephrectomy for renal cell carcinoma. Int Urol Nephrol 42:299–303
Aziz A et al (2014) Comparative analysis of comorbidity and performance indices for prediction of oncological outcomes in patients with upper tract urothelial carcinoma who were treated with radical nephroureterectomy. Urol Oncol Semin Orig Investig 8:1141–1150
Berger DA et al (2008) Impact of comorbidity on overall survival in patients surgically treated for renal cell carcinoma. Urology 72:359–363
Chang C-M, Yin W-Y, Wei C-K, Wu C-C, Su Y-C, Yu C-H, Lee C-C (2016) Adjusted age-adjusted Charlson comorbidity index score as a risk measure of perioperative mortality before cancer surgery. PLoS One 11:e0148076
de Cássio Zequi S, de Campos EC, Guimarães GC, Bachega W Jr, da Fonseca FP, Lopes A (2010) The use of the American Society of Anesthesiology Classification as a prognostic factor in patients with renal cell carcinoma. Urol Int 84:67–72
Dias-Santos D, Ferrone CR, Zheng H, Lillemoe KD, Fernández-del Castillo C (2015) The Charlson age comorbidity index predicts early mortality after surgery for pancreatic cancer. Surgery 157:881–887
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17:1471–1474
Escudier B et al (2016) Renal cell carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 27:v58–v68
Extermann M (2000) Measurement and impact of comorbidity in older cancer patients. Crit Rev Oncol Hematol 35:181–200
Fuhrman SA, Lasky LC, Limas C (1982) Prognostic significance of morphologic parameters in renal cell carcinoma. Am J Surg Pathol 6:655–663
Gettman MT, Boelter CW, Cheville JC, Zincke H, Bryant SC, Blute ML (2003) Charlson co-morbidity index as a predictor of outcome after surgery for renal cell carcinoma with renal vein, vena cava or right atrium extension. J Urol 169:1282–1286
Ho CH, Chen YC, Chu CC, Wang JJ, Liao KM (2017) Age-adjusted Charlson comorbidity score is associated with the risk of empyema in patients with COPD. Medicine 96:e8040. https://doi.org/10.1097/md.0000000000008040
Islam KM, Jiang X, Anggondowati T, Lin G, Ganti AK (2015) Comorbidity and survival in lung cancer patients. Cancer Epidemiol Prev Biomark 24:1079–1085
Kang HW et al (2016) Impact of young age at diagnosis on survival in patients with surgically treated renal cell carcinoma: a multicenter study. J Korean Med Sci 31:1976–1982
Kang HW et al (2017) Impact of the ASA physical status score on adjuvant chemotherapy eligibility and survival of upper tract urothelial carcinoma patients: a multicenter study. J Korean Med Sci 32:335–342
King SC, Pollack LA, Li J, King JB, Master VA (2014) Continued increase in incidence of renal cell carcinoma, especially in young patients and high grade disease: United States 2001 to 2010. J Urol 191:1665–1670
Ko K, Park YH, Lee JW, Ku JH, Kwak C, Kim HH (2013) Influence of nutritional deficiency on prognosis of renal cell carcinoma (RCC). BJU Int 112:775–780
Koppie TM et al (2008) Age-adjusted Charlson comorbidity score is associated with treatment decisions and clinical outcomes for patients undergoing radical cystectomy for bladder cancer. Cancer Interdiscipl Int J Am Cancer Soc 112:2384–2392
Ljungberg B et al (2019) European Association of Urology guidelines on renal cell carcinoma: the 2019 update. Eur Urol 75:799–810
Lund L, Jacobsen J, Nørgaard M, McLaughlin JK, Blot WJ, Borre M, Sørensen HT (2009) The prognostic impact of comorbidities on renal cancer, 1995 to 2006: a Danish population based study. J Urol 182:35–40
Motzer RJ et al (2017) Kidney cancer, version 2.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 15:804–834
Park JW et al (2018) Age-adjusted Charlson comorbidity index as a prognostic factor for radical prostatectomy outcomes of very high-risk prostate cancer patients. PLoS One 13:e0199365
Robbins JR, Gayar OH, Zaki M, Mahan M, Buekers T, Elshaikh MA (2013) Impact of age-adjusted Charlson comorbidity score on outcomes for patients with early-stage endometrial cancer. Gynecol Oncol 131:593–597
Santos Arrontes D, Fernandez Acenero MJ, Garcia Gonzalez JI, Martin Munoz M, Paniagua Andres P (2008) Survival analysis of clear cell renal carcinoma according to the Charlson comorbidity index. J Urol 179:857–861
Søgaard M, Thomsen RW, Bossen KS, Sørensen HT, Nørgaard M (2013) The impact of comorbidity on cancer survival: a review. Clin Epidemiol 5:3
Suidan RS et al (2015) Predictive value of the age-adjusted Charlson comorbidity index on perioperative complications and survival in patients undergoing primary debulking surgery for advanced epithelial ovarian cancer. Gynecol Oncol 138:246–251
Verhoest G et al (2007) Relationship between age at diagnosis and clinicopathologic features of renal cell carcinoma. Eur Urol 51:1298–1305
Wu C-C, Hsu T-W, Chang C-M, Yu C-H, Lee C-C (2015) Age-adjusted Charlson comorbidity index scores as predictor of survival in colorectal cancer patients who underwent surgical resection and chemoradiation. Medicine 94:e431
Zheng Y, Bao L, Wang W, Wang Q, Pan Y, Gao X (2018) Prognostic impact of the Controlling Nutritional Status score following curative nephrectomy for patients with renal cell carcinoma. Medicine 97:e13409
Zisman A et al (2001) Improved prognostication of renal cell carcinoma using an integrated staging system. J Clin Oncol 19:1649–1657
Funding
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Education (2018R1D1A1B07043906).
Author information
Authors and Affiliations
Consortia
Contributions
Conception and study design: HWK and YJK. Acquisition of data: SMK, WTK, and SJY. Statistical analysis: SMK, WTK and SJY. Drafting and writing of the manuscript: HWK. Revision and critical review of the manuscript: S-CL, W-JK, ECH, SHK, S-HH, JC, TGK, HHK, CK, S-SB, and Y-JK. Manuscript approval: all authors.
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the relevant institutional review boards of the eight participating centers, and informed consent was waived by the board.
Informed consent
Informed consent was waived by the board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

432_2019_3042_MOESM1_ESM.jpg
Supplementary material 1 Supplementary Fig. Kaplan–Meier survival curves showing (a) cancer-specific survival, and (b) overall survival according to pathologic T stages (pT < 2 vs. ≥ 2) (JPEG 454 kb)
Rights and permissions
About this article
Cite this article
Kang, H.W., Kim, S.M., Kim, W.T. et al. The age-adjusted Charlson comorbidity index as a predictor of overall survival of surgically treated non-metastatic clear cell renal cell carcinoma. J Cancer Res Clin Oncol 146, 187–196 (2020). https://doi.org/10.1007/s00432-019-03042-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-019-03042-7