Abstract
Objectives
To evaluate the temporal relationship between interval to biochemical recurrence (BCR) following radical prostatectomy (RP) and prostate cancer-specific mortality (PCSM).
Patients and methods
The study comprised of 2,116 men from the Victorian Radical Prostatectomy Register, a whole-of-population database of all RPs performed between 1995 and 2000 in Victoria, Australia. Follow-up prostate-specific antigen and death data were obtained via record linkage to pathology laboratories and the Victorian Registry of Births, Deaths and Marriages. Poisson regression models with PCSM as the outcome were fit to the data. Models included age at surgery, Gleason score and tumour stage as covariates.
Results
Median post-surgery and post-BCR follow-up was 10.3 and 7.5 years, respectively. 695 men (33 %) experienced BCR during follow-up, of which 82 % occurred within 5 years of RP; 66 men died from prostate cancer. Men with combined high Gleason sum (≥4 + 3) and extra-prostatic (≥pT3a) disease had substantially increased mortality rate with early BCR, while those experiencing BCR after a longer interval had significantly lower mortality. Men with combined low Gleason sum (≤3 + 4) and organ-confined disease (≤pT2c) risk disease were not at any substantial risk of death in this time frame regardless of timing of BCR following RP.
Conclusions
This study evaluates the temporal relationship between BCR and PCSM using a whole-of-population cohort of men treated with RP. Men with low-risk features of prostate cancer at time of RP have low mortality even if they experience early BCR. This subgroup may be counselled regarding their favourable long-term prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate-specific antigen (PSA) surveillance following radical prostatectomy (RP) provides an effective means of monitoring for disease recurrence [1]. Approximately, 17–31 % of men may be expected to experience biochemical recurrence (BCR) during follow-up [2–4], and the risk of developing disease recurrence increases with adverse pathological findings, such as extra-prostatic extension, higher-grade Gleason score and positive surgical margins [2, 4–6]. However, the natural history of disease recurrence following RP can have a long and protracted course. Pound et al. [7] demonstrated a median time of 8 years to development of metastases following BCR and a further median of 5 years until death from prostate cancer. Compared to men with slow increases in PSA levels following BCR, men with rapid PSA doubling times (PSA DT) following BCR have increased risk of progression to metastatic disease and prostate cancer-specific mortality (PCSM) [7, 8]. PCSM following RP has been reported to be approximately between 2 and 7 % in mainly large, high-volume institutional series [3, 4, 9, 10].
The prognostic significance of interval from surgery to BCR on mortality from prostate cancer is unclear [7, 8, 11–16]. Most studies evaluating this temporal relationship have defined early or late BCR as a categorical variable, which may have practical limitations when counselling men as the timing of BCR can be variable, and not all men who experience BCR before or after a certain point in time have similar outcomes. Furthermore, the majority of studies assessing this temporal relationship are based on data from high-volume institutional series, which may not reflect patient characteristics or outcomes seen on a community or population level. Early BCR following RP is associated with earlier progression to metastatic disease and death [7, 12, 13]. Conversely, men with delayed BCR have a more favourable long-term prognosis and are more likely to have lower-risk prostate cancer at the time of their surgery [14, 16]. Several large studies with long-term follow-up have demonstrated that mortality in men with low-risk disease is very low [10, 17, 18].
While delayed BCR may be associated with a more favourable prognosis, it is unclear if all men in this subgroup have a similar prognosis. Additionally, while men with low-risk prostate cancer have low mortality overall, there is uncertainty whether early BCR in these men confers an increased risk of mortality. Using a prospective whole-of-population-based series of men who underwent RP for localised prostate cancer during the PSA-era, we assessed the effect of timing of BCR on PCSM in men with post-RP follow-up of more than 10 years.
Patients and methods
Patients
The Victorian Radical Prostatectomy Register (VRPR) is a whole-of-population series of men who underwent RP for the treatment of prostate cancer between 1995 and 2000 in Victoria, Australia. The VRPR was established within the Victorian Cancer Registry (VCR) to record additional information on men who underwent RP. Details of VRPR registration and data collection have been reported previously [19]. The VRPR was approved by the Human Research Ethics Committee of Cancer Council Victoria.
All men underwent PSA testing prior to RP. Tumour details coded to ICDO-2 topography, and morphology rubrics were abstracted from pathology reports submitted to the VCR, and record linkage to the VRPR for both biopsies and RP specimens was subsequently performed. Total prostatectomies performed at cystoprostatectomy for bladder cancer were excluded.
Full follow-up PSA-testing histories were obtained via record linkage to pathology laboratories. BCR was defined as two consecutive PSA values ≥0.2 μg/L, with the date of BCR set to the latter of the two test dates. Deaths were coded by the VCR as either due to prostate cancer or other causes, based on death records obtained from the Victorian Register of Births, Deaths and Marriages. Follow-up began at the date of BCR and ended at the date of death, date of the last ascertained PSA test, or 1 January 2010, whichever occurred first.
Statistical analysis
Poisson regression models, with prostate cancer cause-specific death as the outcome, were fit to the data. In order to obtain mortality rates per 10 person-years, we included log(follow-up time/10) as an offset with its coefficient constrained to equal 1. All models included age at surgery (<55, 55–65, ≥65), Gleason score and tumour stage as covariates.
We modelled time to BCR as continuous covariate, using restricted cubic splines with knots at the twenty-fifth, fiftieth and seventy-fifth percentiles of time to BCR to allow for a nonlinear relationship with the log(mortality rate). Predicted marginal mortality rates were calculated from the fitted models for given values of time to BCR. Confidence intervals (CI) for the predicted log mortality rates were calculated and back transformed to the natural metric. In order to examine whether the predicted mortality rates depended on patient characteristics, we also fit models for low versus high Gleason score, low (≤pT2c) versus high (pT3a, pT3b, pT4) tumour stage and positive versus negative surgical margins. Low Gleason score was defined as less than or equal to Gleason 7 but with a predominance of Gleason 3 pattern (total ≤3 + 4) and high Gleason score as greater than or equal to 7 but with a predominance of Gleason 4 pattern (total ≥4 + 3). These models included the additional covariate of interest fully interacted with the restricted cubic spline basis functions of time to BCR.
Statistical analyses were performed using Stata 12.0 for Linux 64-bit (Stata corporation, College Station, TX, USA).
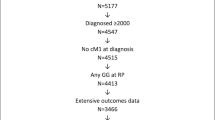
Results
During the accrual period, 2,154 men underwent RP. Median post-surgery follow-up was 10.3 years. Post-surgery PSA follow-up data was available for 2,116 men, 695 of whom experienced BCR during their follow-up.
Eighty-two percentage of men who experienced BCR did so within 5 years of surgery; 16 % had BCR between five and 10 years post-surgery and 2 % had BCR more than 10 years after surgery. During a median post-BCR follow-up of 7.5 years (4,880 total person-years observed), 66 men (10 %) who experienced BCR eventually died from prostate cancer. Of these deaths, 13 (20 %) and six (9 %) occurred following a PSA progression-free period of 5 and 6 years, respectively.
When the characteristics of men who experienced BCR and who survive following disease recurrence were compared to men who died of prostate cancer; there was no substantial difference between the age distribution of the two groups, nor was there any difference in the proportion of patients who underwent surgery in a private hospital, although a higher proportion of men who experienced PCSM were from a rural area compared to metropolitan areas (35 vs. 17 %). Men who experienced PCSM were also more likely to have a higher tumour stage and Gleason score at surgery, but not positive surgical margins.
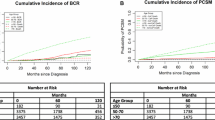
Mortality following biochemical recurrence
Figure 1 presents the predicted overall PCSM rate per 10 person-years for given values of the time between surgery and BCR. The mortality rate decreases with increasing time between surgery and BCR. For BCR at 2 years post-surgery, the mortality rate is 0.14 (95 % CI 0.11–0.19), compared to 0.06 at 5 years (95 % CI 0.02–0.14).
The predicted mortality rate for men with low Gleason sum (≤3 + 4) was low regardless of the time between surgery and BCR. With BCR at two and five years post-surgery, the predicted mortality rate is 0.07 (95 % CI 0.04–0.11) and 0.05 (95 % CI 0.02–0.13), respectively. Conversely, earlier BCR is associated with high predicted mortality rate for men with high Gleason sum (≥4+3), as evidenced by a predicted mortality rate of 0.42 (95 % CI 0.28–0.63) with BCR at 2-year post-RP. However, the mortality rate reduces substantially with increasing interval to BCR, where a mortality rate of 0.08 (95 % CI 0.02–0.27) with BCR at 5 years post-RP is comparable to men with low Gleason sum.
Analysis by tumour stage yielded similar results. The mortality rate for BCR at 2 years post-surgery was substantially higher for men with extra-prostatic disease (0.33, 95 % CI 0.23–0.49) compared to men with organ-confined disease (0.05, 95 % CI 0.02–0.09). However, with delayed BCR at 5 years post-surgery, the mortality rates were more comparable as men with extra-prostatic disease and organ-confined disease had mortality rates of 0.08 (95 % CI 0.03–0.21) and 0.05 (95 % CI 0.02–0.18), respectively.
Models including both Gleason score and tumour stage categorised into low-, intermediate- and high-risk showed a similar pattern (Fig. 2). Men with high-risk disease, as defined by high Gleason sum (≥4 + 3) and extra-prostatic disease, were shown to have significant risk of PCSM with early BCR. Similarly, men with intermediate-risk disease (either low Gleason sum and extra-prostatic disease, or high Gleason sum and organ-confined disease) had higher PCSM with early recurrence. With late BCR, neither of these two groups had substantially increased risk of PCSM. Men with low-risk disease, as defined by low Gleason sum (≤3 + 4) and organ-confined disease, had low mortality rates regardless of early or late BCR.
Discussion
In this whole-of-population series of men who underwent RP and subsequently experienced BCR, we found that the association between BCR and the rate of PCSM depended critically on the interval to BCR from surgery. Men with adverse pathological findings, such as high Gleason score and extra-prostatic disease, who experienced BCR shortly after surgery had a substantially increased mortality rate, while those experiencing BCR after a longer interval had a low mortality rate. Men with low-risk disease were not at any substantial risk of death regardless of when their BCR occurred.
Interval to BCR has a time-varying effect on PCSM. The use of Poisson regression analysis in this study clearly demonstrates this interaction, which remains evident after adjusting for other known adverse prognosticators in our models, such as Gleason score, tumour stage and age. To our knowledge, this is the first study evaluating the temporal relationship between BCR and PCSM in a whole-of-population-based cohort outside of the United States.
Our analyses were performed on a prospective whole-of-population registry of men with localised prostate cancer managed with RP, encompassing a heterogenous group of patients, surgeon volume and experience. These findings may more truly reflect outcomes observed on a community and population level.
Recurrence of prostate cancer following attempted surgical cure with RP is detected by increasing levels of PSA during post-surgery surveillance and follows a varying period of undetectable PSA levels [1]. The clinical course of men who experience BCR varies, depending on the timing of BCR following surgery and the velocity of the PSA rise. It is important, however, to identify men who are at greatest quantifiable risk of PCSM in the event of early BCR following surgery. In this study, men with high-risk prostate cancer had substantial mortality with early BCR, and such men may benefit from the early institution of salvage radiotherapy or other additional treatment, especially those with a rapidly increasing PSA [20].
Studies of men with low-risk features of prostate cancer have demonstrated low PCSM where managed with watchful waiting and followed up for 20 years [17, 18]. Similarly, men undergoing RP with Gleason ≤6 and organ-confined tumours have very low mortality after 15 or more years of follow-up [10, 21]. Our population of men treated with RP support the evidence that this subgroup of men have low rates of PCSM, as men with low Gleason sum (≤7 with primary Gleason 3) and organ-confined disease had low mortality regardless of early or late BCR. Consequently, this subgroup of men may be counselled regarding their favourable long-term prognosis in the event of disease recurrence. We caution the advocacy for active surveillance for men with low-risk prostate cancer based on our findings as we have not performed a subgroup analysis of PCSM in men who would have been suitable for active surveillance based on contemporary protocols [22, 23].
Interval from surgery to first BCR is frequently analysed as a categorical variable in studies evaluating the effect of timing of BCR on PCSM. Defining early or late BCR as a point in time following surgery is also less helpful in clinical practice in regards to assessing prognosis, determining treatment options and counselling patients, as the timing of BCR after surgery is variable. Furthermore, no consensus exists on the definition of either early or late BCR, and current available evidence on the influence of interval to BCR following surgery on PCSM appears mixed [7, 13–15].
Pound et al. [7] found a shorter interval from surgery to first BCR (≤2 years) to be predictive of the development of metastases, but it did not significantly influence time until death. Freedland et al. [13] found shorter interval to BCR (<3 years) following RP was associated with increased risk of PCSM, after adjusting for PSADT and high Gleason score ≥8. Similarly, Caire et al. [14] were able to demonstrate a cancer-specific survival advantage in patients with delayed BCR (>5-year post-surgery). The authors also found Gleason sum <7 and PSA <10 ng/mL to be associated with delayed BCR.
Well-established predictors of BCR include high Gleason score, extra-prostatic disease, positive surgical margins and elevated pre-biopsy PSA levels [2, 4–6]. Although we have not assessed for predictors of early or delayed BCR, men with adverse pathological features at time of RP have been previously shown to be at higher risk of early BCR [15, 24]. The majority of cases of BCR in our study occurred within 5 years of surgery. However, we observed that up to 2 % of men who experienced BCR have a PSA progression-free period of 10 years. Similarly, Loeb et al. [16] demonstrated in their series very late recurrence with 4.9 and 1.5 % of BCR occurring after 10- and 15-years of post-surgery follow-up, respectively.
At this stage, there appears to be limited evidence and consensus regarding the frequency and intensity of PSA surveillance following a period of undetectable PSA levels. Current internationally accepted guidelines recommend life-long annual PSA testing after a PSA progression-free period of 3–5 years [25, 26]. But, investigators have demonstrated low risk of delayed BCR in men with Gleason 6 disease and have consequently suggested less intense surveillance in men with low-risk disease after a similar PSA progression-free period [27, 28]. Loeb et al. [16] found that men with undetectable PSA levels for 10-year post-surgery were at low risk of developing subsequent BCR and had extremely low risk of PCSM. Within this subgroup, no men with Gleason 6 tumours progressed to metastatic disease, and the authors suggested that annual PSA testing may not be required in men with Gleason 6 disease and/or limited life expectancy after a progression-free period of 10 years.
Conclusions
Our findings in this study should influence management in the following manner. Data from this whole-of-population registry of RP shows that time to BCR significantly influences prognosis for men with high-risk prostate cancer, who have significant mortality risk with early BCR. These men should undergo intense PSA surveillance following surgery and may be best managed with salvage therapy in the event of BCR. Men with low-risk prostate cancer have low mortality, and time to BCR following surgery does not alter their prognosis. Thus, in the event of early BCR, this subgroup of men may be counselled regarding their favourable long-term prognosis.
References
Stamey TA, Yang N, Hay AR et al (1987) Prostate-specific antigen as a serum marker for adenocarcinoma of the prostate. N Engl J Med 317:909–916
Han M, Partin AW, Zahurak M et al (2003) Biochemical (prostate specific antigen) recurrence probability following radical prostatectomy for clinically localized prostate cancer. J Urol 169:517–523
Porter CR, Kodama K, Gibbons RP et al (2006) 25-year prostate cancer control and survival outcomes: a 40-year radical prostatectomy single institution series. J Urol 176:569–574
Roehl KA, Han M, Ramos CG et al (2004) Cancer progression and survival rates following anatomical radical retropubic prostatectomy in 3,478 consecutive patients: long-term results. J Urol 172:910–914
Boorjian SA, Karnes RJ, Crispen PL et al (2010) The impact of positive surgical margins on mortality following radical prostatectomy during the prostate specific antigen era. J Urol 183:1003–1009
Lodde M, Harel F, Lacombe L et al (2008) Substratification of high-risk localised prostate cancer treated by radical prostatectomy. World J Urol 26:225–229
Pound CR, Partin AW, Eisenberger MA et al (1999) Natural history of progression after PSA elevation following radical prostatectomy. JAMA 5(281):1591–1597
Ward JF, Blute ML, Slezak J (2003) The long-term clinical impact of biochemical recurrence of prostate cancer 5 or more years after radical prostatectomy. J Urol 170:1872–1876
Isbarn H, Wanner M, Salomon G et al (2010) Long-term data on the survival of patients with prostate cancer treated with radical prostatectomy in the prostate-specific antigen era. BJU Int 106:37–43
Stephenson AJ, Kattan MW, Eastham JA et al (2009) Prostate cancer-specific mortality after radical prostatectomy for patients treated in the prostate-specific antigen era. J Clin Oncol 10(27):4300–4305
Antonarakis ES, Feng Z, Trock BJ et al (2012) The natural history of metastatic progression in men with prostate-specific antigen recurrence after radical prostatectomy: long-term follow-up. BJU Int 109:32–39
Freedland SJ, Humphreys EB, Mangold LA et al (2005) Risk of prostate cancer-specific mortality following biochemical recurrence after radical prostatectomy. JAMA 294:433–439
Freedland SJ, Humphreys EB, Mangold LA (2006) Time to prostate specific antigen recurrence after radical prostatectomy and risk of prostate cancer specific mortality. J Urol 176:1404–1408
Caire AA, Sun L, Ode O et al (2009) Delayed prostate-specific antigen recurrence after radical prostatectomy: how to identify and what are their clinical outcomes? Urology 74:643–647
Amling CL, Blute ML, Bergstralh EJ et al (2000) Long-term hazard of progression after radical prostatectomy for clinically localized prostate cancer: continued risk of biochemical failure after 5 years. J Urol 164:101–105
Loeb S, Feng Z, Ross A et al (2012) Can we stop prostate specific antigen testing 10 years after radical prostatectomy? J Urol 186:500–505
Albertsen PC, Hanley JA, Fine J (2005) 20-year outcomes following conservative management of clinically localized prostate cancer. JAMA 293:2095–2101
Johansson J-E, Andren O, Andersson SO et al (2004) Natural history of early, localized prostate cancer. JAMA 291:2713–2719
Bolton D, Severi G, Millar JL et al (2009) A whole of population-based series of radical prostatectomy in Victoria, 1995 to 2000. Aust N Z J Public Health 33:527–533
Trock BJ, Han M, Freedland SJ et al (2008) Prostate cancer-specific survival following salvage radiotherapy vs observation in men with biochemical recurrence after radical prostatectomy. JAMA 18(299):2760–2769
Eggener SE, Scardino PT, Walsh PC et al (2011) Predicting 15-year prostate cancer specific mortality after radical prostatectomy. J Urol 185:869–875
Klotz L, Zhang L, Lam A et al (2010) Clinical results of long-term follow-up of a large, active surveillance cohort with localized prostate cancer. J Clin Oncol 28:126–131
van den Bergh RCN, Vasarainen H, van der Poel HG et al (2010) Short-term outcomes of the prospective multicentre ‘Prostate Cancer Research International: Active Surveillance’ study. BJU Int 105:956–962
Walz J, Chun FKH, Klein EA et al (2009) Nomogram predicting the probability of early recurrence after radical prostatectomy for prostate cancer. J Urol 181:601–607 (discussion 7–8)
Mohler J, Bahnson RR, Boston B et al (2010) NCCN clinical practice guidelines in oncology: prostate cancer. J Natl Compr Canc Netw 8:162–200
Heidenreich A, Bellmunt J, Bolla M et al (2011) EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and treatment of clinically localised disease. Eur Urol 59:61–71
Ahove DA, Hoffman KE, Hu JC et al (2009) Which patients with undetectable PSA levels 5 years after radical prostatectomy are still at risk of recurrence?—implications for a risk-adapted follow-up strategy. Urology 76:1201–1205
Tollefson MK, Blute ML, Rangel LJ et al (2011) Lifelong yearly prostate specific antigen surveillance is not necessary for low risk prostate cancer treated with radical prostatectomy. J Urol 184:925–929
Acknowledgments
We want to thank participating urologists for their valuable contribution to the VRPR. Initial funding for this project was obtained from a grant in aid from Esso Australia. Ongoing support and infrastructure has been provided by The Cancer Council of Victoria and by the Whitten Foundation.
Conflict of interest
No member of the authorship group has, or did have at any time, any conflict of interest regarding the accrual or publication of the data obtained as part of this ongoing study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bolton, D.M., Ta, A., Bagnato, M. et al. Interval to biochemical recurrence following radical prostatectomy does not affect survival in men with low-risk prostate cancer. World J Urol 32, 431–435 (2014). https://doi.org/10.1007/s00345-013-1125-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-013-1125-0