Abstract
Purpose
To study the association between time from diagnosis to radical prostatectomy (RP-interval) and prostate cancer-specific mortality (PCSM), histological findings in the RP-specimen and failure after RP (RP-failure).
Methods
Patients diagnosed with non-metastatic prostate cancer (PCa) in 2001–2010 and prostatectomized within 180 days of biopsy were identified in the Cancer Registry of Norway and the Norwegian Prostate Cancer Registry. Patients were stratified according to risk groups and RP-intervals of 0–60, 61–90, 91–120 and 121–180 days. Aalen-Johansen and Kaplan–Meier methods estimated curves for PCSM, RP-failure and overall mortality. Multivariable Cox regressions and Chi-square tests were used to evaluate the impact of RP-interval on outcomes.
Results
In 5163 eligible patients, the median time from diagnosis to RP was 93 days (range 1–180). Risk group distribution was similar in all RP-interval groups. With almost eight years of observation, no association was found between RP-interval and PCSM in the intermediate-or high-risk groups. Increasing RP-interval did not increase the rate of adverse histological outcomes or incidence of RP-failure.
Conclusions
Increasing RP-interval up to 180 days was not associated with adverse oncological outcomes at eight years follow-up. These findings should be considered when planning for prostatectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
More than 90% of men diagnosed with prostate cancer (PCa) today have no distant metastases [1]. Patients with a life expectancy of 10 or more years are considered candidates for curative treatment with radical prostatectomy (RP) or high-dose radiotherapy (RAD) [2]. Treatment is generally provided as soon as possible after diagnosis, or in selected low-risk patients preceded by a period of active surveillance (AS).
It is a common perception among patients, physicians and decision-makers that delay in cancer treatment adversely affects oncological outcomes. Reports documenting analyzes of the association between time-to-treatment and clinical outcomes, however, show equivocal findings among different cancer types [3,4,5,6,7]. The length of time from diagnosis to RP (‘RP-interval’) has not been shown to impact long-term oncological outcomes, even when months and years have elapsed since diagnosis [8,9,10,11]. In contrast, other studies have shown unfavorable effects on pathological outcomes [8, 12] and biochemical recurrence (BCR) rates [8, 13].
For cancer patients, delays in diagnosis and treatment may aggravate psychological distress [14]. In line with other European countries, the Norwegian health authorities implemented in 2015 a fast track cancer patient pathway (CPP) for patients with suspected PCa, providing upper limits for time intervals from referral to diagnosis and start of treatment (Online Appendix 1). Such standardized CPPs may possibly meet the emotional needs and expectations of the patients. However, currently there is little scientific evidence to support that RP beyond a certain time will adversely affect oncological outcomes in PCa patients.
With this background, our observational study primarily investigates the relation between the length of the RP-interval and PCa-specific mortality (PCSM). Secondarily, we evaluated the association between RP-intervals and adverse histological findings in the RP specimen and incidence of failure after RP (‘RP-failure’).
Material and methods
Data sources
Data were extracted from the Cancer Registry of Norway (CRN) and the Norwegian prostate cancer registry (NoPCR). For prostatectomized patients, these registries contain demographic data and basic diagnostic variables, including the date of the first cancer-positive biopsy and RP, along with histopathological findings in the RP specimen [15]. The referral and treatment decision dates are not recorded in the CRN. Data on radiotherapy and death statistics can be extracted, but information on disease progression or post-RP systemic therapy is not available. The study was approved by the Regional Committee for Medical and Health Research Ethics (2011/1746).
Patients
Eligible patients had to meet the following criteria:
-
Diagnosis of non-metastatic PCa in the time period 2001–2010
-
RP within 180 days of the first cancer-positive biopsy
-
PSA ≤ 100 ng/mL
-
Biopsy Gleason score (GS) ≥ 5
-
Information on clinical (c) T-category, PSA and GS to allow risk group categorization
Patients whose diagnosis was based on cysto-prostatectomy or who were treated abroad were ineligible.
Data management
Patients were divided into RP-interval groups according to the time from the first cancer-positive biopsy to RP (0–60, 61–90, 91–120 and 121–180 days). Considering time from biopsy to treatment decision, the first RP-interval is in accordance with the maximum RP waiting time of 32 days depicted in the CPP.
Patients were stratified into low-, intermediate-or high-risk groups according to the European Association of Urology Guidelines 2017 [2].
-
Low-risk: PSA < 10 ng/mL and GS < 7 and cT1–T2a
-
Intermediate-risk: PSA 10–20 ng/mL or GS 7 or cT2b
-
High-risk localised: PSA > 20 ng/mL or GS > 7 or cT2c
-
High-risk locally advanced: any PSA, any GS, cT3–4
In less than 10% of the cohort (n = 439) data for risk group categorization was missing, and imputation was deemed unnecessary.
If a patient was recorded with an unknown cT2 subgroup (n = 618), he was allocated to the localized high-risk group if he had a GS >7 or PSA > 20 ng/mL, and to the low-risk group if he had a GS < 7 and PSA< 10 ng/mL. All other cT2x tumors were included in the intermediate-risk group. Information on the node (N) category was not available, but performing RP in patients with known N+ disease was not common practice in this time period.
Based on the routinely recorded histopathology of the RP specimen, we considered tumors to be upstaged if the T-category increased by ≥ 2 categories in cT1 patients (pathological ≥ T3) and ≥ 1 category in ≥ cT2 patients. Patients were stratified into biopsy GS-categories (GS 5–6, GS7a, GS7b, GS8, GS9–10). Tumors were considered upgraded if the pathological GS increased by at least one category compared to the biopsy GS. Patients were furthermore divided into groups based on the time of diagnosis (2001–2007 and 2008–2010) to account for the implementation of the 2005 International Society of Urological Pathology (ISUP) GS modifications in Norway [16].
RP-failure, as available from the CRN, was defined as having received post-RP pelvic RAD (≥ 50 Gy) or mammillary RAD, whatever occurred first, indicating BCR. In the time of this cohort, prophylactic mammillary RAD was common practice before initiation of anti-androgen treatment.
Statistical analyzes
Patients were followed from the date of RP until the date of study outcomes (death from PCa or RP-failure), death from other causes, emigration or end of follow-up (December 31st 2015), whichever came first. Overall mortality was estimated using the Kaplan–Meier method. The Aalen–Johansen estimator estimated PCSM, treating death from other causes as a competing risk, and RP-failure, treating death from any cause as a competing risk. To compare PCSM- and RP-failure development across patient groups we estimated a univariable Fine-Gray regression and performed a Wald test of equality of coefficients. Multivariable Cox-regressions documented the impact of RP-interval on the cause-specific hazard of PCa death, as well as the cause-specific hazard of RP-failure, adjusting for potential confounding factors. Standard chi-square tested the association between the RP-interval groups and the rates of upstaging, upgrading and surgical margin status. A p value of < 0.05 was considered statistically significant. Data were analyzed using the IBM Statistical Package for the Social Sciences (SPSS) version 23 and Stata version 14.2.
Results
In the 5163 evaluable patients, 17%, 31%, 26% and 27% of patients underwent RP 0–60, 61–90, 91–120 and 121–180 days from diagnosis (Table 1). The median time from diagnosis to RP was 93 days (range 1–180). The age and risk group distribution were similar in all RP-interval groups. Of all patients included in this cohort, 29% had high-risk disease. Among these, 18% were treated with RP within 60 days compared to 26% between 121–180 days from diagnosis.
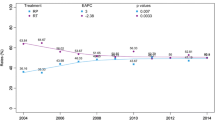
After a median follow-up of 7.9 years (range 0–15), 99 patients (1.9%) had died from PCa (Table 1). For all patients, the 5-year and 10-year PCSM rates were 0.7% and 2.5%, respectively, without any significant difference between time periods (Supplementary Table 5, Supplementary Fig. 3). In the intermediate-risk, high-risk localized and high-risk locally advanced groups, there were no significant differences in PCSM according to RP-interval (Fig. 1). A statistically significant difference emerged for patients in the low-risk group (p < 0.001), but this analysis was regarded as invalid due to event paucity. On multivariate analysis cT-category, biopsy GS and risk group were associated with PCSM, but not RP-interval, PSA, age group or year of diagnosis (Table 2a, b).
No associations between the length of the RP-interval and the rate of upstaging (22%) or upgrading (34%) were demonstrated (Tables 3, 4). The surgical margins were positive in 28% of the RP specimens (low-risk: 23%, high-risk: 35%). Increasing RP-interval was not associated with higher rates of positive surgical margins (PSM) in any risk group (Tables 3, 4).
After a median time of 1.9 years (range 0.1–12.5) after RP, 1273 patients (24.7%) experienced RP-failure. Of these, 528 (41.5%) belonged to the high-risk group at the time of diagnosis. In all risk groups, increasing RP-interval was significantly associated with decreased probability of RP-failure (Fig. 2). This finding was confirmed in multivariate analysis (Online Appendix 2). With low-risk group as reference increasing risk group was associated with significantly increasing hazard ratios of RP-failure (Online Appendix 2).
Discussion
In this population-based cohort with a follow-up time of almost eight years, increasing RP-interval up to 180 days was not associated with increased PCSM in intermediate-or high-risk patients, or with adverse histological outcomes or RP-failure in any risk group.
Our findings are in agreement with a systematic review by Van den Bergh et al. concluding that an association between the timing of RP and PCSM has not yet been documented [8]. The majority of reviewed studies included low and intermediate-risk patients only. Importantly, as shown by Korets et al. and Redaniel et al., this finding confirmed by us, is also valid for high-risk patients [9, 17].
The documented PCSM rates in this cohort are comparable to other observational studies covering patients diagnosed in the same time period [ 18–22]. As expected with a large proportion of high-risk patients, the PCSM is higher than demonstrated in the Protect trial including only screening-detected patients with intra-capsular tumors [23]. Despite a shift towards a larger proportion of prostatectomized patients having high-risk disease (2001–2007: 25.2%, 2008–2010: 32.6%), we observed no difference in PCSM for patients diagnosed in the early versus late period, possibly explained by a decrease in the rate of PSM and intensified adjuvant and salvage treatment in the late period [24].
The observation that increasing RP-interval was not associated with adverse pathological outcomes in our study is in agreement with Sun et al. who found that timing of RP did not affect the rate of upstaging [25]. Neither did Korets et al. find an impact of time from the last positive biopsy to RP on the rate of upgrading or pT-categorization [17]. On the contrary, Berg et al. observed, in patients from the same institution, a significant increase in the proportion of adverse pathological outcomes (upstaging, seminal vesicle invasion, positive lymph nodes, upgrading, PSM) with RP beyond 75 days, ranging from 30 to 150 days depending on the GS and PSA level at the time of diagnosis [12]. In terms of recurrence, Abern et al. found that a delay beyond 9 months was significantly related to PSM and BCR in low- and intermediate risk patients [27], while Zanaty et al. found a positive association between increasing time to RP and BCR in the high-risk group beyond 90 days [13]. The majority of studies, however, do not show increased incidence of BCR with increasing RP-interval, and our findings support these data [8]. We were surprised to find that the risk of RP-failure decreased with increasing RP-interval. This finding may indicate that patients with shorter RP-intervals had more aggressive disease than reflected by our co-variates (e.g., the number of biopsy cores involved with cancer, the percentage of cancer within each biopsy core, PSA doubling time).
We do not know the reasons for increasing RP-interval in this cohort. National guidelines were not implemented in Norway until 2009, and clinical decisions were mainly based on preferences of the treating physician. Increasing age, a co-existing cancer diagnosis or more favorable tumor characteristics did not explain increasing RP-intervals. AS was not formally recorded in the CRN at this time.
The implementation of CPPs in Norway is a political initiative based on the Danish model aiming to improve quality of PCa care [28]. By streamlining services, patients are provided with an efficient and predictable path in close dialog with the hospital, avoiding unnecessary delays. The CPP may facilitate better hospital organization and planning based on available resources and ensure equal cancer handling across regions.
There are, however, challenges with the implementation of the CPP. The time limits for diagnosis and treatment of PCa have proven difficult to put in practice and are currently complied with in about half of the cases. Contrary to the intention of the CPP, patients may suffer additional distress from treatment delay as they anticipate worse prognosis with RP beyond 32 days [29]. The medical rationale behind the time limit for RP, being independent of individual risk assessment, is questioned by clinicians. Medically related delay, like health status optimization or extensive pre-operative planning, may be necessary in selected patients. Moreover, in a time with emerging therapeutic options, patients may wish to seek second opinions before deciding on treatment. Patient preferences and expectations regarding treatment are highly dependent on in-depth counseling by the treating physicians. In our opinion, these priorities, although time-consuming, better reflect quality of PCa care than strict adherence with time limits for RP.
There are several limitations to this study. Firstly, although the registration of new cases of PCa in the CRN is close to complete, the reporting of post-diagnosis outcomes is less exhaustive [1]. Secondly, histological evaluation of prostate biopsies was performed by multiple pathologists without central review, and patients diagnosed before the implementation of the 2005 ISUP modifications were evaluated according to the old Gleason grading system. Third, information on eventual re-biopsies or pre-RP changes in PSA or clinical stage was not available. Fourth, our data on RP-failure underestimates the true incidence of BCR, because the CRN and NoPCR provided no information on post-RP PSA or androgen-deprivation therapy for distant metastasis. Fifth, in older patients, the cause of death may be uncertain as shown in a previous report from the CRN [30]. Finally, this study did not investigate the associations between increasing RP-interval and functional or psychological outcomes. The strength of this study is the long-term follow-up of a large population-based cohort of patients with RP as initial treatment, of which almost one third of the patients had high-risk disease.
Conclusions
Based on the above, the time from diagnosis to RP performed within 6 months of diagnosis is not associated with adverse oncological outcomes at eight years follow-up. These findings should be taken into consideration when counseling candidates for prostatectomy and planning surgical resources at the hospitals. Our study warrants revision of the length of the RP-interval in the current Norwegian CPP for PCa.
References
Cancer Registry of Norway (2017) Annual Report 2016 with Results and Improvements from the Norwegian Prostate Cancer Registry. https://www.kreftregisteret.no/globalassets/publikasjoner-og-rapporter/arsrapporter/publisert-2017/arsrapport-2016_prostatakreft.pdf. Accessed Oct 2018
Mottet N, Bellmunt J, Bolla M et al (2017) Guidelines on Prostate Cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 71(4):618–629. https://doi.org/10.1016/j.eururo.2016.08.003
Neal RD, Tharmanathan P, France B et al (2015) Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? Systematic review. Br J Cancer 112(Suppl 1):S92–S107. https://doi.org/10.1038/bjc.2015.48
Bruins HM, Aben KK, Arends TJ, Heijden AG, Witjes AJ (2016) The effect of the time interval between diagnosis of muscle-invasive bladder cancer and radical cystectomy on staging and survival: a Netherlands Cancer Registry analysis. Urol Oncol 34(4):e161–e166. https://doi.org/10.1016/j.urolonc.2015.11.006
Jensen AR, Nellemann HM, Overgaard J (2007) Tumor progression in waiting time for radiotherapy in head and neck cancer. Radiother Oncol 84(1):5–10. https://doi.org/10.1016/j.radonc.2007.04.001
Jooste V, Dejardin O, Bouvier V et al (2016) Pancreatic cancer: wait times from presentation to treatment and survival in a population-based study. Int J Cancer. 139(5):1073–1080. https://doi.org/10.1002/ijc.30166
Bourgade V, Drouin SJ, Yates DR et al (2014) Impact of the length of time between diagnosis and surgical removal of urologic neoplasms on survival. World J Urol. 32(2):475–479. https://doi.org/10.1007/s00345-013-1045-z
van den Bergh RC, Albertsen PC, Bangma CH et al (2013) Timing of curative treatment for prostate cancer: a systematic review. Eur Urol 64(2):204–215. https://doi.org/10.1016/j.eururo.2013.02.024
Redaniel MT, Martin RM, Gillatt D, Wade J, Jeffreys M (2013) Time from diagnosis to surgery and prostate cancer survival: a retrospective cohort study. BMC Cancer 13:559. https://doi.org/10.1186/1471-2407-13-559
O'Callaghan ME, Shi Z, Kopsaftis T, Moretti K (2017) Prostate cancer outcomes and delays in care. Int Urol Nephrol 49(3):449–455. https://doi.org/10.1007/s11255-017-1508-z
Morini MA, Muller RL, de Castro Junior PCB, de Souza RJ, Faria EF (2018) Time between diagnosis and surgical treatment on pathological and clinical outcomes in prostate cancer: does it matter? World J Urol 36(8):1225–1231. https://doi.org/10.1007/s00345-018-2251-5
Berg WT, Danzig MR, Pak JS et al (2015) Delay from biopsy to radical prostatectomy influences the rate of adverse pathologic outcomes. Prostate 75(10):1085–1091. https://doi.org/10.1002/pros.22992
Zanaty M, Alnazari M, Ajib K et al (2018) Does surgical delay for radical prostatectomy affect biochemical recurrence? A retrospective analysis from a Canadian cohort. World J Urol 36(1):1–6. https://doi.org/10.1007/s00345-017-2105-6
Seklehner S, Hladschik-Kermer B, Lusuardi L, Schabauer C, Riedl C, Engelhardt PF (2013) Psychological stress assessment of patients suffering from prostate cancer. Scand J Urol 47(2):101–107. https://doi.org/10.3109/00365599.2012.700946
Hernes E, Kyrdalen A, Kvale R et al (2010) Initial management of prostate cancer: first year experience with the Norwegian National Prostate Cancer Registry. BJU Int. 105(6):805–811. https://doi.org/10.1111/j.1464-410X.2009.08834.xdiscussion 811
Epstein JI, Allsbrook WC Jr, Amin MB, Egevad LL, Committee IG (2005) The 2005 International Society of Urological Pathology (ISUP) consensus conference on gleason grading of prostatic carcinoma. Am J Surg Pathol 29(9):1228–1242. https://www.ncbi.nlm.nih.gov/pubmed/16096414. Accessed Oct 2018
Korets R, Seager CM, Pitman MS, Hruby GW, Benson MC, McKiernan JM (2012) Effect of delaying surgery on radical prostatectomy outcomes: a contemporary analysis. BJU Int 110(2):211–216. https://doi.org/10.1111/j.1464-410X.2011.10666.x
Pompe RS, Davis-Bondarenko H, Zaffuto E et al (2017) Population-based validation of the 2014 ISUP Gleason grade groups in patients treated with radical prostatectomy, brachytherapy, external beam radiation or no local treatment. Prostate. https://doi.org/10.1002/pros.23316
Abdollah F, Schmitges J, Sun M et al (2012) Comparison of mortality outcomes after radical prostatectomy versus radiotherapy in patients with localized prostate cancer: a population-based analysis. Int J Urol 19(9):836–844. https://doi.org/10.1111/j.1442-2042.2012.03052.x
Stattin P, Holmberg E, Johansson JE et al (2010) Outcomes in localized prostate cancer: National Prostate Cancer Register of Sweden follow-up study. J Natl Cancer Inst 102(13):950–958. https://doi.org/10.1093/jnci/djq154
Aas K, Axcrona K, Kvale R et al (2017) Ten-year mortality in men with nonmetastatic prostate cancer in Norway. Urology 110:140–147. https://doi.org/10.1016/j.urology.2017.07.048
Holmstrom B, Holmberg E, Egevad L et al (2010) Outcome of primary versus deferred radical prostatectomy in the National Prostate Cancer Register of Sweden Follow-Up Study. J Urol 184(4):1322–1327. https://doi.org/10.1016/j.juro.2010.06.008
Hamdy FC, Donovan JL, Lane JA et al (2016) 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med 375(15):1415–1424. https://doi.org/10.1056/NEJMoa1606220
Vatne K, Stensvold A, Myklebust TA et al (2017) Pre- and post-prostatectomy variables associated with pelvic post-operative radiotherapy in prostate cancer patients: a national registry-based study. Acta Oncol. https://doi.org/10.1080/0284186X.2017.1314006
Sun M, Abdollah F, Hansen J et al (2012) Is a treatment delay in radical prostatectomy safe in individuals with low-risk prostate cancer? J Sex Med 9(11):2961–2969. https://doi.org/10.1111/j.1743-6109.2012.02806.x
Kvale R, Moller B, Wahlqvist R et al (2009) Concordance between Gleason scores of needle biopsies and radical prostatectomy specimens: a population-based study. BJU Int 103(12):1647–1654. https://doi.org/10.1111/j.1464-410X.2008.08255.x
Abern MR, Aronson WJ, Terris MK et al (2013) Delayed radical prostatectomy for intermediate-risk prostate cancer is associated with biochemical recurrence: possible implications for active surveillance from the SEARCH database. Prostate 73(4):409–417. https://doi.org/10.1002/pros.22582
Sundhedsstyrelsen (2016) Pakkeforløb for prostatakræft. https://www.sst.dk/da/sygdom-og-behandling/kraeft/pakkeforloeb/~/media/086DCAA5E5B14713BA08556124EB4681.ashx. Accessed Oct 2018
Norwegian Directorate of Health (2016) Pakkeforløp for prostatakreft. https://helsedirektoratet.no/retningslinjer/pakkeforlop-for-prostatakreft. Accessed Oct 2018
Skyrud KD, Bray F, Moller B (2014) A comparison of relative and cause-specific survival by cancer site, age and time since diagnosis. Int J Cancer 135(1):196–203. https://doi.org/10.1002/ijc.28645
Acknowledgements
We would like to thank the Norwegian Cancer Society (Fund no. 5781243), the Radium Hospital Foundation (Project no. 335007) and the Vestre Viken Hospital Trust (Project no. 2503002) for financial support.
Funding
This study was funded by the Norwegian Cancer Society (Fund no. 5781243), the Radium Hospital Foundation (Project no. 335007) and the Vestre Viken Hospital Trust (Project no. 2503002).
Author information
Authors and Affiliations
Contributions
KA: Protocol/project development, Data collection or management, Data analysis, Manuscript writing/editing. SDF: Protocol/project development, Data collection or management, Data analysis, Manuscript writing/editing. RK: Data analysis, Manuscript writing/editing. BM: Protocol/project development, Data collection or management, Data analysis, Manuscript writing/editing. TÅM: Data collection or management, Data analysis, Manuscript writing/editing. LV: Data collection or management, Manuscript writing/editing. SM: Data analysis, Manuscript writing/editing. VB: Protocol/project development, Data analysis, Manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
345_2018_2570_MOESM4_ESM.pdf
Prostate cancer-specific mortality (left) and overall mortality (right) in patients diagnosed with non-metastatic prostate cancer according to year of diagnosis (2001-07 vs 2008-10). PCa: prostate cancer (PDF 64 kb)
Rights and permissions
About this article
Cite this article
Aas, K., Fosså, S.D., Kvåle, R. et al. Is time from diagnosis to radical prostatectomy associated with oncological outcomes?. World J Urol 37, 1571–1580 (2019). https://doi.org/10.1007/s00345-018-2570-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2570-6