Abstract
Introduction
Recently, small renal masses (SRMs) (≤4 cm) are found more frequently, especially in the elderly and co-morbid patients. Standard treatment for SRMs is nephron-sparing surgery (NSS). New techniques like energy ablation and surveillance have been introduced.
Materials and methods
Overview of treatment options for SRMs, based mainly on the meta-analyses available for NSS, cryoablation, radio-frequency ablation (RFA), and surveillance.
Results
NSS for SRMs is the standard therapy with excellent cancer-specific survival rates up to 97%. Cryoablation was mainly performed laparoscopically, and RFA mainly percutaneously. Pretreatment biopsies were used frequently for cryoablation (80%) and less frequently for RFA (50%). Primary failure rate for cryoablation was 4.8% and for RFA 13%. Major complication rates for both procedures are around 5%. Based on 6-month post-ablative biopsies, non-contrast enhancement seems to be an effective surrogate marker after cryoablation, but not after RFA. Follow-up after energy ablation is too short to draw final conclusion. Data on surveillance are based on small, retrospective data with insufficient follow-up. Growth patterns during follow-up do not correlate with the underlying tumour entity.
Conclusion
Standard therapy for SRMs is still NSS. Energy ablation should be reserved for the elderly patients with co-morbidities and surveillance for the elderly and infirm patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nephron-sparing surgery (NSS) is the current standard of care for small renal masses (SRMs) (smaller or equal to 4 cm) [1]. This approach demonstrated excellent outcomes with 5-year cancer-specific survival (CSS) rates up to 97%. With the advances and widespread usage of cross-sectional imaging, the detection of renal tumours has increased in the last three decades and thereafter decreased since 2004 in Austria [2]. This rise is mostly due to the increasing detection of SRMs, especially in the elderly and co-morbid patients. The United States NCI Surveillance Epidemiology and End Results Program (SEER) data between 1983 and 2002 showed that the detection of SRMs was almost threefold higher for tumours <2 cm and 2–4 cm, respectively. Whereas the detection rate of 4–7 cm and >7 cm just rose by 50 and 26%, respectively [3]. Today, the vast majority of SRMs are diagnosed incidentally and therefore tend to have a better prognosis [4–6]. But despite the detection of more and more SRMs, mortality rates of renal cell carcinoma (RCC) rose, e.g. in the USA from 1.5 deaths to 6.5 per 100.000 individuals between 1983 and 2002, respectively. This is most probably due to the fact that the absolute number of patients with detectable lethal lesions has not diminished. And it is these larger, lethal masses that mainly mediate mortality. Because surgery cures only a fraction of these cancers, mortality is unaffected. Additionally, a lead time bias is suggested [3]. Taken together, this data suggest an overtreatment of SRMs.
Energy ablative techniques (mostly radio-frequency ablation (RFA) and cryoablation) and surveillance protocols have evolved as alternative management options [7, 8]. Oncological short-term and intermediate results for these energy ablative therapies showed promising and comparable results to NSS [6]. Recently, emerging data on active Surveillance (AS) for SRM in selected patients are promising but they also surrogate an overtreatment for SRMs [9, 10]. Today, the challenge in treating SRMs is to find a balance between the need for the surgical treatment of aggressive tumours and the observation of less aggressive or harmless tumours [8].
Benign tumours
Today, being able to choose the correct patient management for SRMs requires the full comprehension of their natural history, aggressive potential, and their growth characteristics. Most renal tumours are considered to be RCCs. Benign renal tumours are grouped into renal cell tumours, metanephric tumours, mesenchymal tumours, and mixed epithelial and mesenchymal tumours. Some benign lesions such as typical angiomyolipomas (AML) show unique radiological characteristics and with today’s imaging modalities they can be distinguished from other renal tumours. However, it is mostly very difficult to identify SRMs as benign or malign [11]. Most of the time a histological evaluation is needed to ascertain an accurate diagnosis and to implement the optimal treatment. In recent surgical series, the incidence of benign tumours is about 20% [11–14]. Vasudevan et al. [15] analysed 70 diagnostic core biopsies and correlated them with final pathology. They reported 33% of cases considered malignant on radiological examination to be ultimately benign in renal biopsies and in 47% of patients in whom a benign pathology was proven by biopsies, radical surgery was avoided. Similarly, a recent report by Remzi et al. [16] declared only 17% of all benign lesions to be correctly identified as benign at preoperative CT scans. Forty-three per cent of these lesions were overtreated with a radical nephrectomy.
Is tumour size a predictor for biological behaviour?
In a study observing 287 SRMs, 24.6, 20.4, and 16.0% of renal tumours with a size of ≤2 cm, 2–3 cm, 3–4 cm were reported to be benign, respectively. A correlation with tumour size was not observed (P = 0.66). Additionally, there was a dramatic increase in potential aggressive parameters beyond a tumour diameter of 3 cm. It was also shown that 4.2, 5, and 25.5% of renal cell carcinomas (RCC) <=2 cm, 2.1–3 cm, and 3.1–4 cm in diameter respectively, had Fuhrman grade G3/4. Again 4.2, 14.9, 35.7% had advanced stage (pT3a or higher) for the same categories, respectively (P = 0.0023) [11]. Gill et al. observed 30% of the 100 lesions (mean diameter 2.8 cm) on which they performed laparoscopic partial nephrectomy to be benign [17]. In their study including 1208 SRMs, Klatte et al. observed a frequency of benign lesions in the tumour size ranges 0.1–1.0, 1.1–2.0, and 2.1–3.0 to be 15, 14, and 14%, respectively. They also observed a significant decrease in the incidence of benign lesions in tumours measuring 3.1–4.0 cm (8%, P = .001) [18]. In a larger report from the Mayo clinic [19], 2935 solid renal tumours of all sizes treated over a 25-year period were retrospectively examined, the results showed 46.3, 22.4, 22.0, and 19.9% of renal lesions <1, 2, 3, and 4 cm in size, respectively, to be benign. Therefore, tumour size alone is not sufficient to distinguish between benign and malignant tumour nature or between RCC with less aggressive or more aggressive behaviour [18].
Role of biopsy
A recent review by Remzi et al. described why, in whom, and how a renal tumour biopsy (RTB) should be performed [8]. In recent years, the potential role of biopsy (renal core and aspiration biopsy) for renal tumours has improved. This is due to the fact that about 20% of SRMs are actually benign [11–19]. In addition, accuracy and safety of renal mass biopsy has improved substantially [8, 20–23]: False-negative rates are low (about 1%; 10–15% are indeterminate), symptomatic complications requiring interventions occur in less than 2%, needle-tract seeding is exceedingly rare and besides all, molecular analyses provide an improved accuracy [8, 21]. Thus, renal tumour biopsies gained popularity in patient counselling and clinical decision-making, but is only useful if the result will affect patient management, which also implies that all treatment modalities are available. Limitations of renal tumour biopsies are multifocality, hybrid tumours [24], and cystic tumours. Recommended uses for RTB in SRMs are (1) to help in differentiating benign from malignant lesions; (2) prior to or during ablative therapies; and (3) during follow-up after ablative therapies, especially after RFA, for defining treatment success or failure.
Nephron-sparing surgery (NSS) and radical nephrectomy (RN)
NSS is the standard care for clinical T1a lesions today, especially for the young and healthy. This is because patients with SRMs who are treated with NSS exhibit similar recurrence-free (0–3%) and CSS rates when compared to RN [7, 25–28]. However, RN is associated with an increased risk of chronic kidney disease. Recent data showed an association between chronic kidney disease and cardiovascular morbidity and mortality [29, 30]. Thus, the goal of today is to spare as much nephrons as possible. Despite all, today, NSS even for SRMs is still underutilized, i.e. in the USA for <20% [31] and in England for <4% [32]. This is an emerging quality-of-care concern.
The choice between laparoscopic (L-NSS) or open (O-NSS) NSS depends on surgeon’s skills as well as on tumour features. The first studies on L-NSS during its learning curve disclosed higher morbidity rates. However, the new studies from the hands of experienced surgeons with shorter ischaemia times and lower complication rates present better long-term oncologic and renal functional outcomes, with decreased patient morbidity compared to open NSS [33]. The largest series with more than 1800 patients (771 L-NSS, 1029 O-NSS) showed significant lower blood loss (300 vs. 376 ml), operating time (201 vs. 266 min), and duration of hospitalization (3.3 vs. 5.8 days) for the L-NSS compared to O-NSS (P < 0.0001), with an equivalent 3-year survival rate of 99.3 and 99.2%, respectively. However, warm ischaemia time (30.7 vs. 20.1 min), post-operative complications (18.6 vs. 13.7%), and subsequent procedures (6.9 vs. 3.5%) were significantly higher in the L-NSS group compared to O-NSS (P < 0.0001), regardless of significant smaller tumour size 2.6 vs. 3.3 cm and better performance status of the patients in the L-NSS group [34]. Recently, also robotic-assisted laparoscopic NSS has been added in the armamentarium for the treatment of SRMs [35].
A recent meta-analysis [28] showed that the total major urological complication rates for O-NSS were 6.3%, statistically similar to L-NSS (9.0%), cryotherapy (4.9%) and RFA (6.0%). The major non-urological complication and re-intervention rates for O-NSS were only 2.2 and 1.6%, respectively. Additionally, O-NSS had the longest follow-up (mean 55.5 months, which was significant longer than for all other modalities (L-NSS, cryoablation, RFA and surveillance) and the highest number of treated patients (n = 5057) in literature.
Energy ablative therapies: cryoablation and radio-frequency ablation (RFA)
Prerequisites for the success of minimal invasive therapies are as follows: (1) Comparable oncological outcomes to the standard treatment of NSS (95–100% cancer-specific survival after 5–10 years, local recurrence rate 5% after 10 years), (2) lower morbidity compared to standard treatment, and finally (3) excellent preservation of kidney function.
Both procedures can be performed percutaneously or laparoscopically. Cryoablation is mainly performed laparoscopically (75%) whereas RFA is mainly performed percutaneously (84%) [36]. Mean follow-up for cryoablation (n = 463) was 19.5 months and for RFA (n = 528) 22.9 months [28]. Possible advantages of cryoablation and RFA compared to laparoscopic or open NSS are (1) Lower morbidity, (2) lower hospitalization time, (3) treatment option for surgical unfit patients. Disadvantages are (1) tumour remains in situ thus surgical radicality cannot be assessed adequately; (2) definition of treatment success (mainly lack of contrast enhancement) is not based on evidence and reports showed in up to 47% viable tumour [37] regardless of no contrast enhancement 6 months after RFA, (3) close radiological follow-up with consecutive contrast-enhanced investigations.
Patients treated with energy ablative techniques are significantly older (68 vs. 60 years, P < 0.001) and have smaller tumours (2.6 vs. 3.1 cm, P < 0.001) than patients treated with NSS [7, 28]. Patient selection is a main criterion for the success of energy ablation, because RCC even in a SRM can be dangerous and can cause mortality if left un- or undertreated. Salvage therapies for advanced RCCs are not curative.
Cryoablation
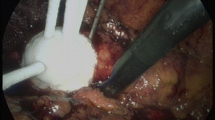
The main advantage of the laparoscopic approach is the precise positioning of the cryoprobes and monitoring of the evolving ice ball by ultrasound and direct visualization. Moreover, adjacent organs can be mobilized away from the ablation site.
Biopsy rates for cryoablation (80%) were significantly higher than that for RFA [7]. A recent report demonstrated excellent correlation between 6-month post-ablative findings and subsequent percutaneous biopsy of treated lesions. No lesion without enhancement on post-treatment imaging revealed viable tumour [37]. However, in most patients routine post-ablation biopsies were not performed [7, 8, 28].
Oncological outcome
Insufficient ablation, as defined by the “Working Group on Image-Guided Tumor Ablation” is the necessity of performing more than one ablation to achieve radiological success (no contrast enhancement), was 4.8% for cryoablation and14.0% for RFA [38] This is not only due to the technique itself, but more likely due to the approach (percutaneously or laparoscopically). However, skipping seems to be an inherent problem of RFA [39]. Data on CSS should be interpreted with high caution, because the definition of success is unclear. Patient selection is always in favour of energy ablation compared to NSS series (smaller tumour size and older patients), and tumour entity is unknown or benign in a significant proportion.
Complication rates
The major urological complication rate for cryoablation was 4.9%; this rate was similar to rates for RFA, OPN, and ORN and significantly lower than that for LPN. The most common complication is haemorrhage mostly due to renal fracture. Conversion rates for cryoablation (3.5%) were similar to LPN rates (3.9%) but were nearly twice as high as RFA rates (1.6%). Cryoablation was associated with good renal function preservation in the absence of complications, but renal loss has been reported in the presence of complications [28].
Laguna et al. evaluated the perioperative morbidity of laparoscopic cryoablation in a European multicentre study [40]. One hundred and forty-eight procedures in 144 patients with a median age of 70.5 year and median tumour size of 2.6 cm (range: 1.0–5.6) showed a complication rate of 15.5%. Most of the complications were Clavien grade 1 and 2, and grade 3 complications occurred in 4% of cases.[41] Only one-third of the complications resulted directly from cryoablation procedure. The presence of cardiac conditions, female gender, and tumour size were independent prognostic factors for the occurrence of a perioperative negative outcome.
Radiofrequency ablation
The main advantage of RFA is that only one puncture of the tumour is necessary and thus it can be done theoretically in local anaesthesia and thus percutaneously, which has clearly a lower morbidity than the laparoscopic approach [7, 36].
Oncological outcome
Only 40–50% of SRMs treated with RFA had a pretreatment biopsy [7, 28]. Efficacy outcomes for RFA are 85.2% total and 87% local recurrence-free survival, as defined by the Working Group on Image-Guided Tumor Ablation if more than one ablation is necessary to achieve radiological success (no contrast enhancement) [38]. CSS and metastatic recurrence-free survival after RFA did show favourable initial results. But the re-intervention rate is about 14% [28]. However, many advocates of RFA would consider salvage RFA as easy for incomplete ablation.
Weight et al. showed viable tumour on a routine 6-month post-ablation biopsy in 47%, even in a non-enhancing mass [37]. Raman et al. questioned the value of a 6-month biopsy. They performed a 4 core biopsy after 1 year of RFA in 20 non-enhancing tumours. None of these lesions showed viable tumour [42]. Thus, the value and timing of post-ablation biopsies are unclear.
Complication rates
RFA results in fewer conversions than other procedures with the exception of OPN; however, patients may require re-intervention more frequently than that in other treatment options. Complications associated with RFA are similar to those reported in other treatment modalities [28].
Comparison between partial nephrectomy, cryoablation and radio-frequency ablation
A recent meta-analyses [7] showed that despite shorter follow-up, cryoablation (RR = 7.45) and RFA (RR = 18.23) had a significant higher risk of developing recurrence compared to partial nephrectomy. However, CSS was very high for all modalities.
In summary, energy ablative techniques are minimal invasive but should be reserved for patients with a high surgical risk. This also implies that the patients understand the need for lifelong radiographic surveillance and possible repeat biopsies after treatment. The patient has to be informed that recurrences are seen frequently than that in standard treatment options (NSS), and that surgical salvage after treatment failures can be difficult due to fibrotic reaction within the perinephric space and can be associated with significant complications and loss of the kidney [43].
Following problems are currently associated with energy ablation: (1) no standard technique, (2) no clear indications for patient selection, (3) lack of pretreatment biopsies, (4) No clear definition of success, (5) no standardized follow-up (with or without biopsy, when to perform biopsies). (6) unclear salvage treatment in case of residual tumours.
Active surveillance
Active surveillance is a possible treatment option in elderly patients with severe co-morbidities or in patients who are not willing to undergo surgery. The current literature is mostly based on small, retrospective studies with limited data. Due to unpredictable nature of SRMs, patient recruitment should be done very carefully. Excellent patient compliance and close follow-up with enhanced imaging techniques is essential. Kunkle et al. [7] showed that only about 40% of patients included in surveillance protocols had a histological evaluation. Renal tumour biopsies are recommended for a better understanding of tumour biology. Benign lesion on renal tumour biopsy is an inclusion criterion for active surveillance [9]. A tumour diameter less or equal to 3–4 cm seems to be a better cut-off point for patient selection [8, 9, 44].
Beisland et al. showed a two-year tumour-specific survival in the cohort selected for observation to be 93.3% compared with overall survival (OS) of only 65.9%. From then on, CSS remained stable but 5 years of OS dropped to 42.8%. This study also included tumours larger than 4 cm, which was a risk factor for tumour progression [44]. Recently, Abouassaly et al. reported their results on 110 elderly patients (median 81 years; range 76–95) under active surveillance with an enhancing SRM (median 2.5 cm). Thirty-one percent of patients died from non-RCC-related reasons during a median follow-up of 24 month [45]. In a meta-analysis by Chawla et al. [10], 234 SRM under surveillance were included. Mean lesion size at presentation was 2.60 cm (median 2.48, ranging from 1.73 to 4.08). Lesions were observed for a mean follow-up of 34 months (median 32, ranging from 26 to 39 in all series combined). The mean growth rate was 0.28 cm per year (median 0.28, ranging from 0.09 to 0.86) and only 1% of the patients developed metastatic disease. In 46% of the cases (131 out of 286), a pathological confirmation was available, which showed RCC in 92% (120 of 131). Among RCC, a mean growth rate of 0.40 cm yearly (median 0.35, ranging from 0.42 to 1.6) was observed. Lesion size at presentation did not correlate with growth rate (P = .46). This is concordant with the current literature [7, 10, 44]. Similarly in Kunkle et al’s report, the rate of RCC (83 vs. 89%) in lesions with zero growth was not different than those with a significant growth (0,31 cm/year) [7]. Serial radiographic data alone were insufficient to predict the true natural history of SRM, and patients’ concomitant diseases should also be taken into consideration when deciding for active surveillance. In literature there is also a report of a SRM under active surveillance which exhibits a spontaneous partial regression, yet this remains to be a rare phenomenon [46]. At present, surveillance is still experimental and inclusion of patients has to be highly selective. The optimal protocol will result in 100% cancer-specific survival with 0% overall survival and no other complications from the renal tumour during the follow-up period [47].
It seems to be clear that not all SRMs are good candidates for surveillance. Benign tumours on renal tumour biopsy should be good candidates, and so as less aggressive RCCs [9]. Recently, the Molecular Loss of chromosome 9p has been implicated in the progression of renal cell carcinoma. Brunelli et al. showed the 5-year cancer-specific survival of patients without loss of chromosome 9p to be 88% and to be 43% in those with loss of chromosome 9p (P < 0.001).[48] Molecular detection of loss of chromosome 9p can give prognostic information when recruiting patients for active surveillance. Waldert et al. showed that hybrid RCCs containing parts of oncocytoma and chromophobe RCCs might be candidates for surveillance [24]. Patient’s will to undergo regular CT or MRI scans and possible repeated biopsies (good compliance) is of utmost necessity. Moreover, the patients have to be informed that growth rates on further follow-up might be inadequate to predict the aggressiveness of the tumour [7, 10].
Novel treatments
Numerous treatment modalities such as High-intensity focused Ultrasound (HIFU) Radiosurgery (“Cyberknife”) Microwave Thermotheraphy (MWT), Laser Interstitial Thermal Therapy (LITT), Puls Cavitational Ultrosound (PCU), Natural Orifice Translumenal Endoscopic Surgery (NOTES) are emerging today. These modalities remain to be experimental due to the lack of literature and experience regarding their outcomes. At present, most interesting data are on HIFU: The extracorporeal approach for HIFU ablation of SRMs had major problems. In a phase 2 study, 9 out of 14 SRMs treated with HIFU showed shrinkage, but histopathological examination revealed necrosis in only 15–35% [49]. Similarly in another study, poor results were reported [50]. In a phase one study by Klingler et al., laparoscopic intracorporal HIFU ablation of SRMs has been investigated. Of the 10 patients, 3 showed viable tumour cells after treatment [51]. Currently, HIFU did not reach the safety for treatment of SRM out of phase 1 or 2 studies, but might become an option in the future if the technical difficulties are overcome. NOTES as NSS has been proven to be technically feasible but the current results are immature, with newly emerging data it might in the future be added to the surgical armamentarium. Especially cryoablation seems to be a very promising indication for NOTES [52, 53].
Conclusion
For all novel therapies without histological examination, the term CSS should be used with caution. If no or only a minority of patients had a histological examination, the term tumour-specific survival would be appropriate. Excellent and to NSS comparable CSS rates for all treatment modalities in SRMs are reported in the literature, but follow-up in energy ablative therapies and surveillance are too short to make a conclusion. Today we know that not all SRMs are destined to progress, metastasize, and threaten the life of the patient and there is a rise in the incidence of SRMs especially in the elderly patients with co-morbidities. Thus, minimal invasive therapies and surveillance are new and attractive options to treat those patients. Patient selection is essential for good results when deciding for energy ablative therapies or surveillance. A renal tumour biopsy to understand the tumour biology and to better counsel further follow-up is recommended. Patients have to be precisely informed that recurrence rates after energy ablation are significantly higher compared to standard therapy. The percutaneous approach seems to be less safe than the laparoscopic approach, which can explain higher re-intervention and recurrence rates for RFA compared to cryoablation. Surveillance strategies are still experimental and should be reserved for the old and infirm patient. Standard of care for SRM is O-NSS and in experienced hands Lap-NSS.
References
Ljungberg B, Hanbury DC, Kuczyk MA, Merseburger AS, Mulders PFA, Patard JJ, Sinescu IC (2009) Guidelines on renal cell carcinoma. Update http://www.uroweb.org/fileadmin/tx_eauguidelines/2009/Full/RCC.pdf
Hackl M (2004) Krebsinzidenz und Krebsmortalität in Österreich. Statistik Austria, Vienna
Hollingsworth JM, Miller DC, Daignault S, Hollenbeck BK (2006) Rising incidence of small renal masses: a need to reassess treatment effect. J Natl Cancer Inst 98(18):1331–1334
Jayson M, Sanders A (1998) Increased incidence of serendipitously discovered renal cell carcinoma. Urology 51:203–205
Luciani LG, Gestari R, Tallarigo C (2000) Incidental renal cell carcinoma—age and stage characterization and clinical implications: study of 1092 patients (1982–1997). Urology 56:58–62
Aron M, Gill IS (2007) Minimally invasive nephron-sparing surgery (MINSS) for renal tumours: Part II: Probe ablative therapy. Eur Urol 51:348–357
Kunkle DA, Egleston BL, Uzzo RG (2008) Excise, ablate or observe: the small renal mass dilemma—a meta-analysis and review. J Urol 179:1227–1233
Remzi M, Marberger M (2009) Renal tumor biopsies for evaluation of small renal tumors: why, in whom, and how? Eur Urol 55:359–367
Ozsoy M, Klatte T, Waldert M, Remzi M (2008) Surveillance for the management of small renal masses. Adv Urol 196701
Chawla SN, Crispen PL, Hanlon AL, Greenberg RE, Chen DY, Uzzo RG (2006) The natural history of observed enhancing renal masses: meta-analysis and review of the world literature. J Urol 175:425–431
Remzi M, Özsoy M, Klingler HC, Susani M, Waldert M, Seitz C et al (2006) Are small renal tumors harmless? Analysis of histopathology features according to tumor size in tumors 4 cm or less in diameter. J Urol 176:1–4
Dechet CB, Sebo T, Farrow G, Blute ML, Engen DE, Zincke H (1999) Prospective analysis of intraoperative frozen needle biopsy of solid renal masses in adults. J Urol 162:1282–1284
Özen H, Colowick A, Freiha FS (1993) Incidentally discovered solid renal masses: what are they? Br J Urol 72:274–276
Silver DA, Morash C, Brenner P, Campbell S, Russo P (1997) Pathologic findings at the time of nephrectomy for renal mass. Ann Surg Oncol 4:570–574
Vasudevan A, Davies RJ, Shannon BA, Cohen RJ (2006) Incidental renal tumors: the frequency of benign lesions ad the role of preoperative core biopsy. BJU Int 97:946–949
Remzi M, Katzenbeisser D, Waldert M, Klingler HC, Susani M, Memarsadeghi M et al (2007) Renal tumor size measured radiologically before surgery is an unreliable variable for predicting histopathological features:benign tumors are not necessarily small. BJU Int 99:1002–1006
Gill IS, Matin SF, Desai MM et al (2003) Comparative analysis of laparoscopic versus open partial nephrectomy for renal tumors in 200 patients. J Urol 170(1):64–68
Klatte T, Patard J-J, de Martino M et al (2008) Tumor size does not predict risk of metastatic disease or prognosis of small renal cell carcinomas. J Urol 179(5):1719–1726
Frank I, Blute ML, Cheville JC, Lohse CM, Weaver AL, Zincke H (2003) Solid renal tumors: an analysis of pathological features related to tumor size. J Urol 170:2217–2220
Schmidbauer J, Remzi M, Memarsadeghi M et al (2008) Diagnostic accuracy of computed tomography-guided percutaneous biopsy of renal masses. Eur Urol 53:1003–1012
Volpe A, Kachura JR, Geddie WR, Evans AJ, Gharajeh A, Saravanan A et al (2007) Techniques, safety and accuracy of sampling of renal tumors by fine needle aspiration and core biopsy. J Urol 178:379–386
Silverman SG, Gan YU, Mortele KJ, Tuncali K, Cibas ES (2006) Renal masses in the adult patient: the role of percutaneous biopsy. Radiology 240:6–22
Lane BR, Samplaski MK, Herts BR, Zhou M, Novick AC, Campbell SC (2008) Renal mass biopsy—a renaissance? J Urol 179:20–27
Waldert M, Klatte T, Haitel A, Ozsoy M, Schmidbauer J, Marberger M, Remzi M (2009) Hybrid renal cell carcinomas containing histopathologic features of chromophobe renal cell carcinomas and oncocytomas have excellent oncologic outcomes. Eur Urol. doi: 10.1016/j.eururo.2009.05.009
Lee CT, Katz J, Shi W, Thaler HT, Reuter VE, Russo P (2000) Surgical management of renal tumors 4 cm or less in a contemporary cohort. J Urol 163(3):730–736
Uzzo RG, Novick AC (2001) Nephron-sparing surgery for renal tumors: indications, techniques and outcomes. J Urol 166(1):6–18
Delakas D, Karyotis I, Daskalopoulos G, Terhorst B, Lymberopoulos S, Cranidis A (2002) Nephron-sparing surgery for localized renal cell carcinoma with a normal contralateral kidney: a European three-centre experience. Urology 60(6):998–1002
Novick AC, Campbell SC, Belldegrun A et al. (2009) Guideline for management of the clinical stage 1 renal mass. American Urological Association Web site. http://www.auanet.org/content/guidelinesand- quality-care/clinical-guidelines/main-reports/renalmass09.pdf
Huang WC, Levey AS, Serio AM, Snyder M, Vickers AJ, Raj GV et al (2006) Chronic kidney disease after nephrectomy in patients with renal cortical tumours: a retrospective cohort study. Lancet Oncol 7:735–740
Go AS, Chertow GM, Fan D, McCulloch CE (2004) Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Eng J Med 351:1296–1305
Miller DC, Hollingsworth JM, Hafez KS, Daignault S, Hollenbeck BK (2006) Partial nephrectomy for small renal masses: an emerging quality of care concern? J Urol 175:853–858
Nuttall M, Cathcart P, van der Meulen J, Gillatt D, McIntosh G, Emberton MA (2005) Description of radical nephrectomy practice and outcomes in England: 1995–2002. BJU Int 96:58–61
Heuer R, Gill IS, Guazzoni G, Kirkali Z, Marberger M, Richie JP, de la Rosette JJ (2009) A critical analysis of the actual role of minimally invasive surgery and active surveillance for kidney cancer. Eur Urol. doi: 10.1016/j.eururo.2009.10.023
Gill IS, Kavoussi LR, Lane BR et al (2007) Comparison of 1, 800 laparoscopic and open partial nephrectomies for single renal tumors. J Urol 178:41–46
Rogers C, Menon M, Weise E et al (2008) Robotic partial nephrectomy: a multi-institutional analysis. J Robotic Surg 2:141–143
Hui GC, Tuncali K, Tatli S, Morrison PR, Silverman SG (2008) Comparison of percutaneous and surgical approaches to renal tumor ablation: metaanalysis of effectiveness and complication rates. JVIR 19:1311–1320
Weight CJ, Kaouk JH, Hegarty NJ et al (2008) Correlation of radiographic imaging and histopathology following cryoablation and radio frequency ablation for renal tumors. J Urol 179:1277–1281
Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD III, Dupuy DE et al (2009) Image-guided tumor ablation: standardization of terminology and reporting criteria. J Vasc Interv Radiol 20(Suppl 7):377–390
Klingler HC, Marberger M, Mauermann J, Remzi M, Susani M (2007) ‘Skipping’ is still a problem with radiofrequency ablation of small renal tumours. BJU Int 99(5):998–1001
Laguna MP, Beemster P, Kumar P et al (2009) Perioperative morbidity of laparoscopic cryoablation of small renal masses with ultrathin probes: a European multicentre experience. Eur Urol 56:355–362. doi:10.1016/j.eururo.2009.05.002
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Raman JD, Stern JM, Zeltser I et al (2008) Absence of viable renal carcinoma in biopsies performed more than 1 year following radio frequency ablation confirms reliability of axial imaging. J Urol 179:2142–2145. doi:10.1016/j.juro.2008.01.119
Nguyen CT, Lane BR, Kaouk JH, Hegarty M, Gill IS, Novick AC et al (2008) Surgical salvage of renal cell carcinoma recurrence after thermal ablative therapy. J Urol 180:104–109
Beisland C, Hjelle KM, Reisæter LAR, Bostad L (2009) Observation should be considered as an alternative in management of renal masses in older and comorbid patients. Eur Urol 55(6):1424–1427
Abouassaly R, Lane BR, Novick AC (2008) Active surveillance of renal masses in elderly patients. J Urol 180:505–508
Weibl P, Lutter I, Romancik M, Karwandgar M, Kollarik B, Obsitnik M (2009) Spontaneous regression of complex cystic renal mass of bosniak class IV–a rare phenomenon Bratisl. Lek Listy 110(3):195–196
Remzi M (2009) Editorial comment on: observation should be considered as an alternative in management of renal masses in older and comorbid patients. Eur Urol 55(6):1427–1428
Brunelli M, Eccher A, Gobbo S, Ficarra V, Novara G (2008) Loss of chromosome 9p is an independent prognostic factor in patients with clear cell renal cell carcinoma. Mod Pathol 21(1):1–6
Marberger M, Schatzl G, Cranston D, Kennedy JE (2005) Extracorporeal ablation of renal tumours with high-intensity focused ultrasound. BJU Int 95(Suppl 2):52–55
Hacker A, Michel MS, Marlinghaus E, Kohrmann KU, Alken P (2006) Extracorporeally induced ablation of renal tissue by high-intensity focused ultrasound. BJU Int 97:779–785
Klingler HC, Susani M, Seip R, Mauermann J, Sanghvi N, Marberger M (2008) A novel approach to energy ablative therapy of small renal tumours: laparoscopic high-intensity focused ultrasound. Eur Urol 53:810–816
Merseburger AS, Kuczyk MA (2008) Changing concepts in the surgery of renal cell carcinoma. World J Urol 26:127–133
Kaouk JH, White WM, Goel RK, Brethauer S (2009) NOTES transvaginal nephrectomy: first human experience. Urology 74(1):5–8
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Remzi, M., Javadli, E. & Özsoy, M. Management of small renal masses: a review. World J Urol 28, 275–281 (2010). https://doi.org/10.1007/s00345-010-0516-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-010-0516-8