Abstract
The incidence of renal cell carcinoma has been rising for years, particularly in industrial countries. It is very frequently diagnosed at the early stage of T1a, probably due to better early detection. At the same time, there is an increasing prevalence of chronic renal failure with higher morbidity and shorter life expectancy in those affected. Both factors underscore the urgent need for nephron-sparing treatments. The gold standard has thus shifted from radical to partial nephrectomy. Given good conditions, the intervention can be performed by laparoscopy, which offers the advantages of lower invasiveness. A treatment alternative can be advantageous for selected patients with high morbidity and an increased risk of anesthetic or surgical complications. Appropriate risk stratification requires prior histological confirmation of the small renal mass (cT1a) by assessment of biopsy specimens. Active surveillance represents a controlled delay in the initiation of treatment. Percutaneous radiofrequency ablation (RFA) and laparoscopic cryoablation are currently the most common treatment alternatives, though there are limitations particularly for central tumors near the renal hilum. Newer ablation procedures such as high-intensity focused ultrasound (HIFU), irreversible electroporation, microwave ablation, percutaneous stereotactic ablative radiotherapy, and high-dose brachytherapy have high potential in some cases but are still considered experimental for the treatment of renal cell carcinoma.
M. Schostak and J. J. Wendler contributed equally to this work.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Small renal masses
- Focal therapy
- Active surveillance
- Radiofrequency ablation (RFA)
- Cryoablation
- High-intensity focused ultrasound (HIFU)
- Irreversible electroporation (IRE)
- Microwave ablation (MWA)
- Percutaneous radiotherapy
- Surgery
Introduction
Renal cell carcinoma is a relatively common disease in industrial countries like the German Federal Republic. Factors associated with affluence such as obesity probably play an essential role. In Germany, the Society of Epidemiological Cancer Registers (Gesellschaft der Epidemiologischen Krebsregister, GEKID) and the Robert Koch Institute (RKI) predict a continuous increase over the next few years (Robert Koch-Institut and und die Gesellschaft der epidemiologischen Krebsregister in Deutschland e.V. 2015).
Apart from the rising incidence of all types of cancer with increasing age, there is also an increase in the incidence of other diseases that can have a direct or indirect influence on the clinical course of cancer and particularly also on renal function. Especially chronic renal failure is associated a priori with a poorer life expectancy and a poorer quality of life (Kirchberger et al. 2012).
Radical nephrectomy was historically considered to be the treatment of choice for renal tumors. However, it offers no prognostic advantage over partial nephrectomy, at least for small tumors, and involves a markedly higher probability of consecutive renal failure. Organ-sparing therapy has therefore been established as the first treatment choice in the international guidelines during the last decades. Thus nephron-sparing or renal function-sparing surgery is regarded as the gold standard in the guidelines of the German Cancer Society, the German Urological Association, the European Association of Urology, and the American Urological Association (Olbert et al. 2015). In this context, however, a distinction is made between small renal masses (SRM ≤ 4 cm in diameter) and large ones. It is only at stage T2, i.e., over 7 cm in diameter, that removal of the entire kidney or radical nephrectomy is regarded as the standard treatment, especially since partial nephrectomy is generally no longer possible for tumors of this size (Ljungberg et al. 2016).
Imaging technology has vastly improved in the course of decades. CT and especially MRI now enable adequate differentiation between benign and malignant tumors as well as satisfactory staging. This is paralleled by the development of new treatment techniques suitable for destroying renal tumors in a minimally invasive manner without requiring traditional surgery. In particular, radiofrequency ablation and cryoablation are already available as treatment alternatives. Numerous other ablation techniques still considered experimental are being investigated for their therapeutic advantage.
Confirming the Diagnosis: From Small Renal Masses to Renal Cell Carcinoma
Regardless of the clinical picture, patients should only be expected to endure additional morbidity if it has therapeutic consequences (Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF) 2015). With reference to small renal tumors, this means that a biopsy to histologically confirm the image-based diagnosis of an uncertain mass is only necessary if it helps in selecting the appropriate therapy. For a surgical intervention such as radical or partial nephrectomy, however, imaging of a morphologically suspicious lesion without biopsy confirmation is considered an adequate indication if there are no serious contraindications for surgical exposure. For alternative treatments such as the ablations described in the following, a biopsy is absolutely necessary to compare initial and follow-up histology. It is unclear how preoperative biopsies with negative, i.e., nonmalignant, histology should be assessed. Basically, it would seem that surgery could be avoided in such cases. On the other hand, it is of course possible that the biopsy did not hit the intended target but only shows a central necrotic area, for example. The recommended procedure for solid tumors is a coaxial double-sleeve core biopsy (18-gauge needle) outside a possible central tumor necrosis with histological analysis (Ljungberg et al. 2016).
Cystic tumors are a special entity. They can already be malignant from category IIF (3–10%, most often papillary renal cell carcinomas) according to the morphological Bosniak classification system for CT evaluation (Graumann et al. 2015). Such a finding requires at least follow-up imaging (Visapää et al. 2013). Biopsy of cystic tumors harbors a high risk of false-negative results with a low cell density in fluid as well as the potential risk of a puncture-related needle tract seeding through cyst fluid leakage (Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF) 2015). The procedure recommended to confirm the diagnosis here is a combination of coaxial core biopsy with histological analysis and fine-needle aspiration with cytological analysis (Ljungberg et al. 2016).
For suspected urothelial cancer of the collecting system, particularly if centrally located and/or invading the calyceal system (with or without hematuria), percutaneous biopsy is considered contraindicated because of the increased risk of metastases in the puncture canal (Robertson and Baxter 2011). In such cases, it is essential to attempt endoscopic confirmation of the findings on the condition that this will have therapeutic consequences, as stated above.
Despite the relatively high sensitivity (94–98%) and specificity (100%) of biopsy for accurately diagnosing a renal cell carcinoma, there is a high rate (up to 20%) of false-negative or inconclusive samples. A negative biopsy (normal parenchyma) is therefore an indication for repeat biopsy. A 90% success rate has been described for such a procedure (Ljungberg et al. 2016; Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF) 2015).
Another limitation of biopsy-based diagnosis with precise determination of the tumor entity is the intratumoral biological heterogeneity of renal cell carcinomas (Höfflin et al. 2015). It is difficult in some cases to distinguish between basically benign oncocytomas and oncocytic renal cell carcinomas. Besides, the potential of such tumors to degenerate into cancer is being discussed. Biopsy of small renal masses usually correlates with the initiation of therapy (Maurice et al. 2015).
Active Surveillance and Watchful Waiting
Active Surveillance
The concept of active surveillance (AS) involves regular follow-up imaging for small localized asymptomatic renal tumors (SRM, cT1a, ≤4 cm) that grow slowly and show a low metastatic tendency. This risk is defined by the tumor size and the pathological subtype after histological confirmation by punch biopsy. Curatively intended treatment should only be initiated if the tumor size increases or at the patient’s request. Thus the active surveillance strategy is directly dependent on the tumor biology and the diagnostic certainty. There are no objective criteria for selecting appropriate patients, and no uniform definition of the precise way in which AS should be carried out. To correctly determine whether AS is indicated, it is therefore necessary to consider comprehensive information obtained in an interdisciplinary setting involving urologists, radiologists, pathologists, and possibly other specialists. Numerous studies on the progression of small cT1a renal tumors have revealed a relatively slow growth rate of 0.2–0.4 cm per year and a very low metastatic rate of 1–2% in the first 2–4 years of follow-up. However, these data include a considerable number of histologically unconfirmed tumors or even tumors histologically classified as benign and also comprise substantial heterogeneity within renal cell carcinoma subtypes (Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF) 2015). From a meta-analysis for the subgroup of biopsy-confirmed pT1a renal cell carcinomas (n = 120) with a median tumor size of 2.48 cm (1.7 to 4.0 cm), Chawla et al. calculated a median growth rate of 0.35 cm per year (0.42 to 1.6 cm per year) after a mean follow-up period of 30 months (25 to 39 months), although the initial tumor size did not correlate significantly with the growth rate (Chawla et al. 2006). Thompson et al. described a metastatic rate of 0.13% for renal cell carcinoma < 3 cm (1/178), although the metastatic risk increased by 24% per centimeter of additional growth (Thompson et al. 2009).
Visualization of vascular, capsular, adrenal, and calyceal invasion is a prognostically unfavorable factor and thus a contraindication for AS. Another adverse factor is biopsy histology revealing Fuhrman nuclear grade 3–4 (high-grade) clear cell or non-clear cell renal cell carcinoma. Anatomical classification systems like the PADUA score (preoperative aspects and dimensions used for anatomical classification), the R.E.N.A.L. score (radius, exophytic/endophytic, nearness to collecting systems or sinus, anterior/posterior, and location relative to polar lines), or the C-index can also provide early indications for surgery or the type of surgery and can thus be helpful in making the decision for or against AS (Camacho et al. 2015).
There is no tumor marker for monitoring renal masses; the concept of repeat biopsy to monitor renal tumors during AS has not been established either. Therefore, AS is generally performed only with follow-up imaging (Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF) 2015).
Unfortunately, there is also no recommended scheme for the imaging modality or time interval. Depending on the risk of progression, it may be expedient to adapt the follow-up scheme to the schemes recommended by current guidelines for postoperative care after successful surgical treatment of renal cell carcinoma (Ljungberg et al. 2016; Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF) 2015).
In staging the upper body, conventional noncontrast computed tomography (CT) tends to be advantageous for diagnosing abdominal conditions, while magnetic resonance imaging (MRI) tends to be the better for further differentiating malignancy and grading (Vargas et al. 2013; Hallscheidt et al. 2004). Image-based monitoring during active surveillance should be carried out at least once a year. Retrospective studies and meta-analyses, but no prospective randomized study data, are available on AS of small renal masses and pT1a renal cell carcinomas. Moreover, no large series or meta-analyses have been performed to investigate biopsy-confirmed pT1a renal cell carcinomas during AS (Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF) 2015).
Jewett at al. analyzed a progression rate of 0.13 cm per year and a metastatic rate of 1.1% in 101 biopsy-confirmed pT1a renal cell carcinomas over a median follow-up of 28 months (Jewett et al. 2011). Lane et al. found no significant survival difference between AS and surgical treatment with partial or radical nephrectomy for small renal masses in 537 patients with a mean age ≥75 years. However, only 4% of 148 deaths during a median follow-up of 3.9 years were attributed to clinical progression of renal cell carcinoma (Lane et al. 2010). Pierorazio et al. found that quality of life did not differ between immediate treatment and active surveillance groups after one year of follow-up (Pierorazio et al. 2013). In general, AS is not recommended for renal tumors >4cm with ill-defined margins and/or marked inhomogeneity or for biopsy-confirmed aggressive renal cell carcinoma or nonmorbid patients with a long life expectancy and morphologically suspicious imaging findings. In clinical use, however, active surveillance is now retreating more and more into the background in view of the alternative procedures for local ablation described in the following.
Watchful Waiting
In patients with a low life expectancy (e.g., due to old age or very high comorbidity), follow-up of an incidentally detected asymptomatic tumor would cause unnecessary psychological stress without having therapeutic consequences. Therefore, a wait-and-see strategy without targeted diagnostic or therapeutic measures should be considered in such cases. This watchful waiting or wait-and-see approach differs fundamentally from active surveillance. Factors that can lead to diagnostic procedures and/or therapy include symptoms such as bone pain caused by bone metastasis or hematuria caused by collecting system invasion. The aim here should be purely palliative treatment – for example, radiotherapy for pain relief or embolization/local ablation of the abnormality causing the symptoms. Such a watchful waiting strategy should be accompanied by a procedure known as best supportive care. This includes general support measures such as nutrition counseling, physiotherapy, or targeted pain therapy. Since by definition there are no follow-up imaging examinations or objectifiable quality-of-life parameters, such a procedure cannot be substantiated by large published series.
Ablation
Guideline-Based Ablation Procedures
Radiofrequency ablation (RFA) and cryoablation (CA) are evaluated as alternative curative treatment options for small renal tumors in the guidelines of the German, European, and American urological and radiological associations. The greatest amount of data is available here because these techniques have been used for such a long time; however, there are no data from prospective studies or even randomized controlled trials (Whitson et al. 2012). Apart from effectiveness for tumor control, assessment of the complication rates and quality of life plays an important role. Direct comparison of RFA and CA revealed no superiority of one procedure over the other in terms of disease-specific, relapse-free, or overall survival (Ljungberg et al. 2016). Decisive for the success and complication rate is the location and size of the renal tumor. Camacho et al. demonstrated that an R.E.N.A.L. score > 8 results in a higher local relapse and complication rate with RFA and CA (Camacho et al. 2015).
A definitive assessment of the two procedures as treatment alternatives cannot be made in the current data situation. Therefore, this treatment option is not recommended at present for noncentral T1a renal tumors in older patients with high morbidity and corresponding surgical or anesthetic risks and contraindications (Ljungberg et al. 2016; Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF) 2015).
Radiofrequency Ablation (RFA)
RFA is a hyperthermal ablation technique in which a high-frequency alternating current (375–400 kHz) causes ionic agitation via active electrodes with resultant frictional heat (Joule effect) reaching 100 °C and consecutive coagulation necrosis in the target tissue. This frictional heat is conducted radially outward from the electrode into the tissue (conduction principle). On the whole, temperatures of 50–105 °C are reached with a multivarying effect. At low temperatures, there will be protein denaturation, chromosomal alterations, damage to cellular membranes and organelles, and damage to the vascular system. High temperatures of around 100 °C lead to coagulation, vaporization, and carbonization of tissue (Duffey and Kyle Anderson 2010). Electrodes applied are monopolar or bipolar probes, compact single, cluster, or preferentially expandable guard electrodes of various sizes.
RFA was first applied in 1997 (Zlotta et al. 1997). The probe type, application time, and temperature level influence the size and homogeneity of the ablation zone. Zones ranging up to 7 cm can be achieved. A safety margin of 5–10 mm around the visualized mass is recommended. RFA has limited applicability for central renal cell carcinomas because of their proximity to the hilum and the associated risk of perforation. Heat loss through blood and urine flow (heat-sink convection) should also be taken into account. Prior transarterial embolization of the target and margin tissue can serve to reduce the heat-sink effect through renal arteries.
Open-surgical, percutaneous, and laparoscopic RFA approaches have been described. Percutaneous RFA is the energy-based ablation method most commonly applied for alternative treatment of renal cell carcinoma. It is technically easy to perform and takes relatively little time (10–20 min).
RFA applicators can be monitored by CT or MRI real-time scanning. RFA is performed primarily under local anesthesia with analgesia and sedation. Target temperatures of about 80 °C for 8–10 min are required within the operating temperature range to hyperthermally destroy tissue as completely as possible.
The occasional inhomogeneity and varying vascularity of renal tumors can sometimes lead to incomplete ablation (skipped lesions) through the above-described heat-sink effect with consecutive impedance jumps in the energy flow (Klingler et al. 2007). Thus, despite formally adequate application of the technique, the primary success rate is not 100% but only 90–100%, depending on the size and location of the tumor (Zagoria et al. 2011). The prospects of success are greater for smaller tumors (SRM < 3 cm) and especially for those located in the cortex. Diverse studies describe a progression/local relapse rate of 2–12% for pT1a renal cell carcinomas in the first 5 years (Kunkle and Uzzo 2008).
An advantage of ablation techniques in general is that they can be repeated. A secondary success rate of nearly 100% has been described. The probability of metastatic spread after RFA is comparable to that associated with an active surveillance strategy (metastasis-free and disease-specific survival rates of 95–99%) (T racy et al. 2010). Mostly only minor complications occur after renal RFA and are expected in 0–20%. As mentioned above, proximity to the renal collecting system or large vessels poses a risk, and therefore RFA is not recommended in these cases because it can result in perforations, fistulas, or strictures (Wah et al. 2014). Outcomes of RFA are comparable to those of partial nephrectomy with the reservation that there have been no prospective randomized controlled trials (Takaki et al. 2010). However, expansion of the indications for RFA, possibly even beyond T1a tumors, is to be expected as more and more long-term data become available.
Cryoablation
Cryoablation (CA) is the only hypothermal ablation procedure and was first applied in 1995 as the oldest of the procedures discussed here (Uchida et al. 1995). A cryoprobe is inserted to carry out active freeze-thaw processes with temperatures dropping to -70°C and rising above 0 °C. Subsequent cell dehydration and mechanical disruption through ice crystal formation in the tissue are accompanied by hypoperfusion-related ischemia that ultimately leads to coagulation necrosis in the target area. In contrast to hyperthermal ablation, CA does not provide adequate hemostasis and thus involves an increased risk of bleeding. Like RFA, CA has only limited applicability for centrally located renal cell carcinoma because of its proximity to the renal hilum and the collecting system. Thermoregulation takes place via gas-filled cryoprobes with a thermally insulated shaft and noninsulated tip, utilizing the so-called Joule-Thomson effect (density- and pressure-related temperature change). Argon gas (−180 °C) is used for freezing and helium gas for thawing. Depending on the tumor size, 3–5 cryoablation needles and 2 thermal sensors are placed under image guidance. A safety margin of 5–10 mm is recommended. As described for RFA, the cold-sink effect can compromise the treatment success here too through impedance jumps (Berger et al. 2009). The cold-sink effect can also be reduced for CA by prior transarterial embolization (Duffey and Kyle Anderson 2010).
Like RFA, CA has also been applied using open-surgical, percutaneous, and laparoscopic as well as transluminal and endoscopic approaches. In contrast to RFA, the laparoscopic intervention under general anesthesia is the most widespread technique, though the procedure is currently very rarely performed in Europe. The surgical complexity is high because, like in laparoscopic partial nephrectomy, the kidney has to be surgically exposed so that the needles can be precisely placed in the tumor. After CA has been performed, the ice ball is mechanically compressed for 5–10 min and then visually monitored for another 5–10 min under reduced intra-abdominal gas pressure. Hemostasis can be achieved using liquid or solid hemostyptics or glue; persistent bleeding can also be treated with other surgical procedures such as circular suturing (Gill et al. 2003).
The primary success rate of CA ranges between 90% and 100% for small renal masses (Atwell et al. 2008). For technical reasons, the success rate depends on the tumor size and location; in analogy to RFA, the best results are obtained for tumors < 3 cm and located in the peripheral cortex (Georgiades et al. 2008). Diverse studies have described a progression or local relapse rate ranging between 3% and 17% for T1a tumors in the first 5 years (Atwell et al. 2008; Georgiades et al. 2008; Pirasteh et al. 2011). Thus, in terms of metastasis-free or disease-specific survival, CA also does not differ substantially from purely conservative treatment methods such as active surveillance. The complication rate is low at 2–19%, and mostly only minor complications occur here as well (Gill et al. 2005). The technical and surgical complexity is much greater than with percutaneous radiofrequency ablation. Moreover, the materials are far more expensive, so that the technique is now performed in only very few centers.
Other Potential Alternative Ablation Techniques
High-Intensity Focused Ultrasound (HIFU)
High-intensity focused ultrasound (HIFU) is a hyperthermal ablation procedure with temperatures of over 80 °C. A parabolic reflector is used to focus ultrasound waves of a piezoelectric crystal (1–4 MHz, pulse duration 4–6 s, peak energy 2000 kJ/cm (Kirchberger et al. 2012)) on the target tissue. This subsequently leads to coagulation necrosis as with radiofrequency ablation. Percutaneous HIFU therapy uses the so-called split-beam technology (external HIFU probe with integrated ultrasound coupling) for ablation at a penetration depth of 3.5–8.0 cm. Such a measure usually requires general anesthesia. Percutaneous HIFU is technically difficult to apply, however, due to factors such as respiration-induced kidney motions, acoustic window limitations through signal loss across bone, and dynamic manual ultrasound control (Wu et al. 2003; Ritchie et al. 2010).
Laparoscopic HIFU therapy may circumvent this problem. In analogy to laparoscopic cryoablation, however, this requires laparoscopic exposure of the entire kidney. The HIFU transducer is relatively large (18 mm in diameter). We are dealing here with a HIFU probe (“side firing dual focal length,” Misonix, Inc., USA). During a 10–40 min procedure, the tumor is ablated at a temperature of > 90 °C under real-time ultrasound monitoring. Klingler et al. performed surgical resection of the ablated tumor after laparoscopic HIFU. Ablation was found to be complete in four and incomplete in three of seven patients (Klingler et al. 2008). The HIFU procedure was uneventful in these seven patients. Ritchie et al. analyzed 12 patients with small renal masses (median 3.8 cm, 2.0–4.7 cm, 2 endophytic tumors, 10 exophytic cortical tumors, 4 oncocytomas, and 8 renal cell carcinomas) after uneventful laparoscopic HIFU followed by laparoscopic partial nephrectomy. In eight cases, ablation was incomplete with primarily subcapsular residues (skipped lesions) (Ritchie et al. 2010). The data situation for high-intensity focused ultrasound as a therapy for small renal masses is very limited, and there is a high rate of incomplete ablations in this small series.
Irreversible Electroporation
Irreversible electroporation (IRE) is a relatively new minimally invasive nonthermal technique for tissue ablation. Here a local critical electrically induced disturbance of the cell membrane dipole potential causes irreversible membrane pore formation. This leads to a permanent increase in cell membrane permeability and a loss of cell homeostasis with consecutive cytolysis within 1–7 days. Via 2–6 needles, 90–100 high-energy ultrashort rectangular high-voltage pulses per electrode pair (at least 90 per pair, 1.500–3.000 V, current strength 30–50 A, pulse duration 70–100 μs) are locally applied under endotracheal anesthesia with complete muscle relaxation and ECG triggering. Through the postulated all-or-none reaction starting at a “critical” induced transmembrane potential and the cellular effect (sparing the matrix), the ablated area should exhibit a very small transition zone and sharp delineation between treated and surrounding tissue (Rubinsky 2010). In 2007, IRE (NanoKnife® system; AngioDynamics Inc, 2–6 needle electrodes) was granted approval for clinical application (general approval for soft tissue tumors). Previous experimental and phase-1 publications were able to demonstrate safe application with sparing of the collecting system and renal vessels. In seven patients submitted to CT-guided IRE for pT1a renal cell carcinoma (1.6–3.1 cm), Thomson et al. found five cases of complete ablation and two cases of tumor progression (29%) by follow-up CT after 3 months (Thomson et al. 2011). After CT-guided IRE of 20 peripheral T1a renal tumors (1.5–2.9 cm; including 13 biopsy-confirmed renal cell carcinomas), Trimmer et al. identified residual tumors by CT or MRI morphology in 2 of 20 cases after 6 weeks (10%) as well as a biopsy-confirmed relapse in one of 6 cases after one year (17%) (Trimmer et al. 2015).
First post-resection histological results 4 weeks after IRE of biopsy-confirmed solid pT1a renal cell carcinomas were presented in a phase 2a trial by Wendler et al. Resected tumor samples after IRE showed massive tumor damage without evidence of viable tumor remnants. However, in contrast to previous assumptions, affected nontumorous renal tissue displays side effects such as intimal hyperplasia with large-vessel occlusions in the perifocal area and renal papillary necrosis (Wendler et al. 2015a, 2015b). These first preliminary study results suggest that percutaneous ablation of solid renal cell carcinomas by IRE requires further technical optimation but is basically possible and also favorable as a nephron-sparing therapy for central tumors.
Microwave Ablation
In microwave ablation (MWA), energy is delivered to target tissue by induction of frictional heat. Through its dipole moment, rotational motion is caused by dielectric hysteresis (rotating dipoles) at a frequency of 915–2,450 MHz via a microwave generator (45–200 watts) and appropriate antennas. This generates local temperatures of at least 100 °C and ranging above 150 °C over 10–15 min.
Hyperthermia results in coagulation necrosis with a radius of damage that varies according to the antenna geometry. The literature contains numerous experimental animal studies on in vivo renal tissue but only a few clinical studies on microwave therapy of small renal masses (Floridi et al. 2014). After percutaneous ultrasound-guided MWA in 98 patients with pT1a renal cell carcinomas (0.6–4 cm), Yu et al. found a success rate of 97% over a median period of 26 months and progression in only one case after 32 months. The major complication rate was 1.7% (Yu et al. 2015).
Moreland et al. treated 53 patients with biopsy-confirmed pT1a renal cell carcinoma (0.8–4.0 cm) by percutaneous ultrasound-guided MWA. Follow-up CT or MRI examinations were carried out in 38 patients after 8 months. None of the cases showed a local relapse. The clinical examination revealed a significant change in renal function in six cases (11.3%) (Moreland et al. 2014). Due to its specific mode of action in stimulating water molecules, MWA may be a particularly suitable ablation method for cystic renal tumors or complicated/malignant renal cysts. Carrafiello et al. found an ablation rate of 100% and no relapses over a period of 24 months after percutaneous CT- or ultrasound-guided MWA in seven patients with Bosniak III or IV cysts (1.4–2.7 cm) (Carrafiello et al. 2013). Given the high technical complexity and the relatively large antennas, MWA has thus far been unable to prevail over other percutaneous hyperthermal ablation techniques, particularly RFA.
Percutaneous Radiotherapy
Primary percutaneous radiotherapy for focal treatment of localized renal cell carcinoma is historically regarded as ineffective and thus useless. The basis for this is the relatively high radiation resistance of renal cell carcinoma and the high toxicity in radiosensitive adjacent organs (small and large bowel) due to the lack of tissue-sparing potential. Technological advances enable more precise hypofractionated irradiation (radiosurgery) known as stereotactic ablative radiotherapy. Treatment is delivered in one fraction or only a few fractions (24–40 Gy in 1–5 fractions with 4–25 Gy per fraction). Robot-assisted linear accelerators are applied as well as modern immobilization measures and new computer-based radiation geometry with 3D and 4D simulation, respiratory triggering, fiducial markers, cone beam imaging, intensity-modulated radiotherapy (IMRT), etc.
As opposed to conventional radiotherapy, which induces apoptosis by DNA damage, stereotactic radiotherapy acts on various cellular structures and signaling pathways with consecutive lethal nonthermal damage. Campbell et al. summarized the results of 14 studies published from 2003 to 2015 in which stereotactic ablative radiotherapy (SABR) of localized renal cell carcinomas was performed in 138 patients with 166 T1a-T1b tumors (Campbell et al. 2015). A conclusive uniform assessment, however, is strongly limited by the great heterogeneity of the tumor data and treatment regimens as well as the assessment criteria. The authors conclude that primary SABR may be a future treatment option for local renal cell carcinoma.
Brachytherapy
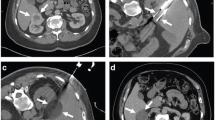
Brachytherapy (BT) delivers very high radiation doses to target tissue via temporarily implanted radiation sources. The typical steep dose reduction can prevent high and unwanted radiation exposure of surrounding tissue. In image-guided afterloading, initially inactive applicators are placed under CT scan real-time monitoring und then secondarily loaded with the divergent radiation source via the afterloader. An exact radiation therapy plan (dose distribution) is calculated via the position and dwell time of the applicators. High-dose rate brachytherapy (HDR-BT) is characterized by a continuous high-dose rate (HDR > 12 Gy/h), Iridium-192 currently being the isotope most commonly used for beta therapy. This leads to lethal nonthermal cell damage by acting on various cellular structures and signaling pathways.
After positioning the brachytherapy catheter via fixed valve introducers (e.g., angiography introducers) inserted by the Seldinger technique under intravenous analgesia and sedation, a contrast-enhanced planning CT or MRI scan (breath-hold technique, section thickness ≤ 5mm) is acquired to determine the exact location in relation to tumor extension (coordinates x, y, z). The irradiation time of about 20–90 min is dependent on the tumor volume (TV); ideally 100% (D 100) of the target volume (TV + safety margin of a few millimeters) should be covered by the intended dose. If necessary, underexposed tumor areas are treated again in a second session.
This technique enables treatment of irregularly shaped tumors without size limitation and regardless of respiratory motion. No clinical data have as yet been published on percutaneous HDR-BT for treatment of localized renal cell carcinoma. The irradiation of renal cell carcinomas and the tolerance dose of nontumorous renal parenchyma are currently being investigated in a prospective phase I/II trial (Ricke et al., University of Magdeburg, Germany) (Bretschneider et al. 2012).The as yet unpublished interim results show good controllability and a good response of renal cell carcinomas.
Surgery
Partial Nephrectomy and Renal Tumor Enucleation
Renal tumor resection is regarded as the treatment of choice, but partial nephrectomy (PN, nephron-sparing surgery) should be performed whenever possible. In experienced centers, laparoscopic and open interventions do not differ with regard to overall or cancer-specific survival. However, laparoscopy is associated with a smaller intraoperative blood loss and a shorter hospital stay than open surgery (Ljungberg et al. 2016; Gill et al. 2007).
The indication with regard to the access path strongly depends on the patient’s constitution, the location of the tumor (R.E.N.A.L. score), and, above all, the surgeon’s experience with laparoscopic nephrectomy. Consecutive urine output is not dependent on the access. Despite shorter operation and ischemia times with open PN with a less marked postoperative decrease in GFR and, on the other hand, lower morbidity with laparoscopic PN, no difference in the degree of renal failure was found after a follow-up period of 3.6 years (Muramaki et al. 2012).
The most important outcome parameter is the ischemia time of healthy renal parenchyma spared, which has to be as short as possible for maximum preservation of renal function. Cooling (cold ischemia) is recommended for an expected ischemia time of more than 25 min. Zero ischemia partial nephrectomy can be performed when a tumor is more favorably, especially peripherally, located and heavy bleeding is not expected (Gill et al. 2011). Furthermore, a maximum of healthy parenchyma should be spared in the sense of a possible tumor enucleation (nephron-sparing surgery).
Meta-analyses after partial nephrectomies or tumor enucleations show a rate of 0–7% for positive resection margins, most of which appear to have no influence on the relapse rate or the cancer-specific or overall survival rate (Marszalek et al. 2012). Therefore, current guidelines recommend a simple follow-up rather than repeat surgery. Comparative studies have not yet been conducted to assess the value of laparoscopic single-port PN or other laparoscopic techniques such as robot-assisted PN.
Conclusions for Clinical Practice
-
1.
Partial nephrectomy is the gold standard for small renal tumors if there is no contraindication.
-
2.
With good image accessibility, active surveillance with or without histological monitoring is also a possible alternative. This is recommended only for selected patients with low-risk renal cell carcinoma < 3 cm.
-
3.
As a “non-therapy,” watchful waiting is a viable option for older and comorbid patients whose renal tumor will probably have no consequences.
-
4.
There are numerous alternative ablation procedures, but only radiofrequency ablation and cryotherapy are guideline approved.
-
5.
All other procedures, as, for example, IRE, are currently considered experimental.
References
Atwell TD, Farrell MA, Leibovich BC, et al. Percutaneous renal cryoablation: experience treating 115 tumors. J Urol. 2008;179:2136–40.
Berger A, Kamoi K, Gill IS, Aron M. Cryoablation for renal tumors: current status. Curr Opin Urol. 2009;19(2):138–42.
Bretschneider T, Peters N, Hass P, Ricke J. Update on interstitial brachytherapy. Radiologe. 2012;52(1):70–3.
Camacho JC, Kokabi N, Xing M, Master VA, Pattaras JG, Mittal PK, Kim HS. R.E.N.A.L. (Radius, exophytic/endophytic, nearness to collecting system or sinus, anterior/posterior, and location relative to polar lines) nephrometry score predicts early tumor recurrence and complications after percutaneous ablative therapies for renal cell carcinoma: a 5-year experience. J Vasc Interv Radiol. 2015;26(5):686–93. https://doi.org/10.1016/j.jvir.2015.01.008. Epub 2015 Mar 11
Campbell SP, Song DY, Pierorazio PM, Allaf ME, Gorin MA. Stereotactic ablative radiotherapy for the treatment of clinically localized renal cell carcinoma. J Oncol. 2015;2015:547143. https://doi.org/10.1155/2015/547143. Epub 2015 Nov 11, Review
Carrafiello G, Dionigi G, Ierardi AM, Petrillo M, Fontana F, Floridi C, Boni L, Rovera F, Rausei S, Mangano A, Spampatti S, Marconi A, Carcano G, Dionigi R. Efficacy, safety and effectiveness of image-guided percutaneous microwave ablation in cystic renal lesions Bosniak III or IV after 24 months follow up. Int J Surg. 2013;11 s.30–35.
Chawla SN, Crispen PL, Hanlon AL, Greenberg RE, Chen DY, Uzzo RG. The natural history of observed enhancing renal masses: meta-analysis and review of the world literature. J Urol. 2006;175(2):425–31.
Duffey BG, Kyle Anderson J. Current and future technology for minimally invasive ablation of renal cell carcinoma. Indian J Urol. 2010;26(3):410–7.
Floridi C, De Bernardi I, Fontana F, Muollo A, Ierardi AM, Agostini A, Fonio P, Squillaci E, Brunese L, Fugazzola C, Carrafiello G. Microwave ablation of renal tumors: state of the art and development trends. Radiol Med. 2014;119(7):533–40. https://doi.org/10.1007/s11547-014-0426-8. Epub 2014 Jul 8
Georgiades CS, Hong K, Bizzell C, Geschwind JF, Rodriguez R. Safety and efficacy of CT-guided percutaneous cryoablation for renal cell carcinoma. J Vasc Interv Radiol. 2008;19:1302–10.
Gill IS, Matin SF, Desai MM, Kaouk JH, Steinberg A, Mascha E, et al. Comparative analysis of laparoscopic versus open partial nephrectomy for renal tumors in 200 patients. J Urol. 2003;170:64–8.
Gill IS, Remer EM, Hasan WA, Strzempkowski B, Spaliviero M, Steinberg AP, et al. Renal cryoablation: outcome at 3 years. J Urol. 2005;173:1903–7.
Gill IS, Kavoussi LR, Lane BR, et al. Comparison of 1,800 laparoscopic and open partial nephrectomies for single renal tumors. J Urol. 2007;178(1):41–6.
Gill IS, et al. “Zero ischemia” partial nephrectomy: novel laparoscopic and robotic technique. Eur Urol. 2011;59(1):128–34.
Graumann O, Osther SS, Karstoft J, Hørlyck A, Osther PJ. Bosniak classification system: a prospective comparison of CT, contrast-enhanced US, and MR for categorizing complex renal cystic masses. Acta Radiol. 2015;56(3):374–83
Hallscheidt PJ, et al. Diagnostic accuracy of staging renal cell carcinomas using multidetector-row computed tomography and magnetic resonance imaging: a prospective study with histopathologic correlation. J Comput Assist Tomogr. 2004;28(3):333–9.
Höfflin R, Roth W, Sültmann H, Grüllich C, Hatiboglu G, Nyarangi-Dix J, Schönberg G, Teber D, Hadaschik B, Pahernik S, Hohenfellner M, Duensing S. Intratumoral heterogeneity in renal cell carcinoma. Molecular basis and translational implications. Urologe A. 2015;54(6):800–3.
Jewett MA, Mattar K, Basiuk J, Morash CG, Pautler SE, Siemens DR, Tanguay S, Rendon RA, Gleave ME, Drachenberg DE, Chow R, Chung H, Chin JL, Fleshner NE, Evans AJ, Gallie BL, Haider MA, Kachura JR, Kurban G, Fernandes K, Finelli A. Active surveillance of small renal masses: progression patterns of early stage kidney cancer. Eur Urol. 2011;60(1):39–44.
Kirchberger I, Meisinger C, Heier M, Zimmermann AK, Thorand B, Autenrieth CS, Peters A, Ladwig KH, Döring A. Patterns of multimorbidity in the aged population. Results from the KORA-Age study. PLoS One. 2012;7(1):e30556.
Klingler HC, Marberger M, Mauermann J, Remzi M, Susani M. ‘Skipping’ is still a problem with radiofrequency ablation of small renal tumours. BJU Int. 2007;99(5):998–1001.
Klingler HC, Susani M, Seip R, Mauermann J, Sanghvi N, Marberger MJ. A novel approach to energy ablative therapy of small renal tumours: laparoscopic high-intensity focused ultrasound. Eur Urol. 2008;53(4):810–6.
Kunkle DA, Uzzo RG. Cryoablation or radiofrequency ablation of the small renal mass: a meta-analysis. Cancer. 2008;113(10):2671–80.
Lane BR, Abouassaly R, Gao T, Weight CJ, Hernandez AV, Larson BT, Kaouk JH, Gill IS, Campbell SC. Active treatment of localized renal tumors may not impact overall survival in patients aged 75 years or older. Cancer. 2010;116(13):3119–26.
Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF). Diagnostik, Therapie und Nachsorge des Nierenzellkarzinoms, S3-Leitlinie, Langversion 1.0; 2015, AWMF Registernummer: 043/017OL. http://leitlinienprogramm-onkologie.de/Leitlinien.7.0.html. Accessed 31 Dec 2016.
Ljungberg B, Bensalah K, Bex A, Canfield S, Dabestani S, Giles RH, Hofmann F, Hora M, Kuczyk MA, Lam T, Marconi L, Merseburger AS, Powles T, Staehler M, Volpe A. Guidelines on Renal Cell Carcinoma. European Association of Urology (EAU); 2016. Accessed 31 Dec 2016.
Marszalek M, Carini M, Chlosta P, Jeschke K, Kirkali Z, Knüchel R, Madersbacher S, Patard JJ, Van Poppel H. Positive surgical margins after nephron-sparing surgery. Eur Urol. 2012;61(4):757–63.
Maurice MJ, Zhu H, Kiechle JE, Kim SP, Abouassaly R. Increasing biopsy utilization for renal cell carcinoma is closely associated with treatment. Urology. 2015;86(5):906–13.
Moreland AJ, Ziemlewicz TJ, Best SL, Hinshaw JL, Lubner MG, Alexander ML, Brace CL, Kitchin DR, Hedican SP, Nakada SY, Lee FT Jr, Abel EJ. High-powered microwave ablation of t1a renal cell carcinoma: safety and initial clinical evaluation. J Endourol. 2014;28(9):1046–52.
Muramaki M, Miyake H, Sakai I, et al. Prognostic factors influencing postoperative development of chronic kidney disease in patients with small renal tumors who underwent partial nephrectomy. Curr Urol. 2012;6:129–35.
Olbert PJ, Maier M, Heers H, Hegele A, Hofmann R. Indications for nephron-sparing surgery. Analysis over a 13-year period in the context of changing guidelines. Urologe A. 2015;54(6):804–10.
Pierorazio P, McKiernan J, Allaf M. Quality of life on active surveillance for small renal masses versus immediate intervention: interim analysis of the DISSRM (delayed intervention and surveillance for small renal masses) registry. J Urol. 2013;189 s.30–35.
Pirasteh A, Snyder L, Boncher N, Passalacqua M, Rosenblum D, Prologo JD. Cryoablation vs. radiofrequency ablation for small renal masses. Acad Radiol. 2011;18:97–100.
Ritchie RW, Leslie T, Phillips R, Wu F, Illing R, ter Haar G, Protheroe A, Cranston D. Extracorporeal high intensity focused ultrasound for renal tumours: a 3-year follow-up. BJU Int. 2010;106(7):1004–9.
Robert Koch-Institut, . (Hrsg). Krebs in Deutschland 2011/2012. 10. Ausgabe. Berlin; 2015.
Robertson EG, Baxter G. Tumour seeding following percutaneous needle biopsy: the real story! Clin Radiol. 2011;66(11):1007–14. https://doi.org/10.1016/j.crad.2011.05.012. Epub 2011 Jul 23
Rubinsky B. Irreversible Electroporation, Series in biomedical engineering. Berlin\Heidelberg: Springer-Verlag; 2010.
Takaki H, Yamakado K, Soga N, et al. Midterm results of radiofrequency ablation versus nephrectomy for T1a renal cell carcinoma. Jpn J Radiol. 2010;28(6):460–8.
Thompson RH, Hill JR, Babayev Y, Cronin A, Kaag M, Kundu S, Bernstein M, Coleman J, Dalbagni G, Touijer K, Russo P. Metastatic renal cell carcinoma risk according to tumor size. J Urol. 2009;182(1):41–5. https://doi.org/10.1016/j.juro.2009.02.128. Epub 2009 May 17
Thomson KR, Cheung W, Ellis SJ, Federman D, Kavnoudias H, Loader-Oliver D, Roberts S, Evans P, Ball C, Haydon A. Investigation of the safety of irreversible electroporation in humans. J Vasc Interv Radiol. 2011;22(5):611–21.
Tracy CR, Raman JD, Donnally C, Trimmer CK, Cadeddu JA. Durable oncologic outcomes after radiofrequency ablation: experience from treating 243 small renal masses over 7.5 years. Cancer. 2010;116:3135–42.
Trimmer CK, Khosla A, Morgan M, Stephenson SL, Ozayar A, Cadeddu JA. Minimally invasive percutaneous treatment of small renal tumors with irreversible electroporation: a single-center experience. J Vasc Interv Radiol. 2015;26(10):1465–71. https://doi.org/10.1016/j.jvir.2015.06.028. Epub 2015 Aug 4
Uchida M, Imaide Y, Sugimoto K, Uehara H, Watanabe H. Percutaneous cryosurgery for renal tumours. Br J Urol. 1995;75(2):132–7.
Vargas HA, Delaney HG, Delappe EM, Wang Y, Zheng J, Moskowitz CS, Tan Y, Zhao B, Schwartz LH, Hricak H, Russo P, Akin O. Multiphasic contrast-enhanced MRI: single-slice versus volumetric quantification of tumor enhancement for the assessment of renal clear-cell carcinoma fuhrman grade. J Magn Reson Imaging. 2013;37(5):1160–7. https://doi.org/10.1002/jmri.23899. Epub 2012 Nov 13
Visapää H, Glücker E, Haukka J, Taari K, Nisen H. Papillary renal cell cancer is strongly associated with simple renal cysts. Urol Int. 2013;91(3):269–72. https://doi.org/10.1159/000351751. Epub 2013 Aug 10
Wah T, Irving H, Gregory W, Cartledge J, Joyce A, Selby P. Radiofrequency ablation (RFA) of renal cell carcinoma (RCC): experience in 200 tumours. BJU Int. 2014;113(3):416–28.
Wendler JJ, Ricke J, Pech M, Fischbach F, Jürgens J, Siedentopf S, Roessner A, Porsch M, Baumunk D, Schostak M, Köllermann J, Liehr UB. First delayed resection findings after irreversible electroporation (IRE) of human localised renal cell carcinoma (RCC) in the IRENE Pilot Phase 2a Trial. Cardiovasc Intervent Radiol. 2015a.;39(2):239–250
Wendler JJ, Porsch M, Nitschke S, Köllermann J, Siedentopf S, Pech M, Fischbach F, Ricke J, Schostak M, Liehr UB. A prospective Phase 2a pilot study investigating focal percutaneous irreversible electroporation (IRE) ablation by NanoKnife in patients with localised renal cell carcinoma (RCC) with delayed interval tumour resection (IRENE trial). Contemp Clin Trials. 2015b;43:10–9. https://doi.org/10.1016/j.cct.2015.05.002. Epub 2015 May 9. PubMed PMID: 25962890
Whitson JM, Harris CR, Meng MV. Population-based comparative effectiveness of nephron-sparing surgery vs ablation for small renal masses. BJU Int. 2012;110(10):1438–43.
Wu F, Wang ZB, Chen WZ, Bai J, Zhu H, Qiao TY. Preliminary experience using high intensity focused ultrasound for the treatment of patients with advanced stage renal malignancy. J Urol. 2003;170(6 Pt 1):2237–40.
Yu J, Zhang G, Liang P, XL Y, Cheng ZG, Han ZY, Zhang X, Dong J, Li QY, MJ M, Li X. Midterm results of percutaneous microwave ablation under ultrasound guidance versus retroperitoneal laparoscopic radial nephrectomy for small renal cell carcinoma. Abdom Imaging. 2015;40(8):3248–56.
Zagoria RJ, Pettus JA, Rogers M, Werle DM, Childs D, Leyendecker JR. Long-term outcomes after percutaneous radiofrequency ablation for renal cell carcinoma. Urology. 2011; 77: 1393–7
Zlotta AR, Wildschutz T, Wood BJ, et al. Radiofrequency interstitial tumor ablation (RITA) is a possible new modality for treatment of renal cancer: ex vivo and in vivo experience. J Endourol. 1997;11:251–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Section Editor information
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this entry
Cite this entry
Schostak, M. et al. (2019). Treatment of Small Renal Masses. In: Merseburger, A., Burger, M. (eds) Urologic Oncology. Springer, Cham. https://doi.org/10.1007/978-3-319-42623-5_61
Download citation
DOI: https://doi.org/10.1007/978-3-319-42623-5_61
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-42622-8
Online ISBN: 978-3-319-42623-5
eBook Packages: MedicineReference Module Medicine