Abstract
A large number of small renal masses (SRMs) with size less than 4 cm are being identified due to advances in diagnostic imaging. As the natural history of these tumours remains unknown, there is no reliable way to predict their behaviour or future growth. Although, partial nephrectomy is the gold standard for treatment of these tumours, ablative non-surgical therapies such as cryoablation and radiofrequency ablation provide a less invasive option of treatment with comparable oncological outcomes. In this systematic review, the principle, indications, methods of treatment, oncological control, complication and renal function of ablative therapies are critically reviewed. Cryotherapy utilizes the principle of inducing tissue destruction by freezing and thawing using argon and helium gasses, respectively. Radiofrequency ablation (RFA) works on the principle of tissue heating. Ablative treatments are particularly useful in the elderly patients, those with comorbidities or in patients with SRMs in solitary kidneys or renal impairment. Ablative therapies have less procedure-related complications and have promising medium-term oncological outcome. Longer-term results are accumulating. Cryotherapy may be a better modality for oncological control than RFA. Ablative therapy has emerged as a viable treatment options for SRMs with recurrence free survival rates approaching that of extirpative surgery. However, there is no consensus in the literature on the best selection criteria and this needs further refinement. Prospective long-term data with regards to oncological control is still needed
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Due to the advances in diagnostic imaging, there has been an increase in identifying localized small renal masses (SRM) of less than 4 cm (stage T1) [1]. The natural history of SRMs is largely unknown [2]. The median radiological rate of growth for SRMs according to a meta-analysis by Chawla et al. was 0.28 cm/year [3]. Partial nephrectomy (PN) remains the gold standard for treatment of SRMs with oncological outcome comparable to radical nephrectomy but with better preservation of the renal function [4–6]. Laparoscopic partial nephrectomy, however, is technically more demanding with a steep learning curve and has a significant complication rate [7]. Robotic partial nephrectomy has made partial nephrectomy easier [8]. The procedure, however, still has a learning curve and warm ischemia time to cope with making it difficult in patients with comorbidities [9]. Ablative therapy provides a less-invasive treatment option in this group of patients with reasonable oncological control comparable to partial nephrectomy [10].
The two most popular ablative therapy techniques are cryoablation and radiofrequency ablation (RFA). Other emerging techniques include high-intensity focused ultrasound (HIFU), interstitial laser ablation and microwave thermotherapy. While there have been large data about the usefulness and limitations of RFA and cryotherapy, the other technologies lack clear evidence currently and can largely be considered to be experimental and evolving [11]. This review mainly examines the role of cryotherapy and RFA in the management of SRMs.
Cryotherapy
Cryotherapy works on the principle of tissue destruction by freezing and thawing using vacuum-insulated liquid argon gas system. It uses rapid cooling of the tip of the cryoprobe by compressed argon gas expanding from its liquid form through the narrow orifice of the probe to a gaseous state. This can focus a very low temperature on a certain spot of the kidney tissue to freeze the tumour [12]. The cooling phase is followed by a thawing phase where helium gas is passed in the same way through the probe to induce thawing [13]. At the cellular level, cryoablation induces acute and delayed tissue damage. The acute effect takes place at −5 °C as ice forms in the extracellular space changing the osmotic gradient and draws the water from inside the cells to the extracellular space leading to protein denaturation through the resulted changes in the intracellular PH and composition [14, 15]. Irreversible damage of the cell membrane occurs when the temperature reaches −20 °C as ice forms in both the intra and extracellular spaces. However, it is believed that the important mechanism of action of cryoablation is the delayed effect resulting from damaging the microvasculature of the renal parenchyma [16]. In the majority of the time, repeated cycles of freezing and thawing enhances tissue destruction with some evidence from animal model experiments showed that double freezing led to large areas of tissue destruction compared to single freezing [17]. During treatment, the temperature achieved is typically between −20 and −40 °C or lower.
Indications
The tumour characteristics for cryotherapy and partial nephrectomy are the same. The typical tumour is situated in the periphery of the kidney, small (<4 cm), exophytic, solid and well-circumscribed. However, cryoablation is particularly useful in elderly patients or those who have significant comorbidity. The technique may also be considered in small lesions of a solitary or transplant kidney; conditions such as tuberous sclerosis or Von Hipple-Lindau’s disease [18]. Some centres are routinely considering cryotherapy as another option for SRMs and discussing with the patients. With experience and with the availability of laparoscopic ultrasound probe cystic and solid lesion such as a Bosniak 4-type tumours are also treated. We advocate that all cases of SRMs are discussed and evaluated in the cancer multidisciplinary setting and appropriate treatment is suggested to an individual patient [19].
Techniques of Cryotherapy
Cryotherapy can be performed either by surgical approach or by percutaneous radiological techniques. The process of delivery of the gasses and the control mechanisms are all computerized.
Surgical Techniques
Laparoscopic approach is the common surgical technique employed for cryotherapy and this could be either trans or retroperitoneal. The transperitoneal technique is ideal for anterior tumours. Hilar lesions, which are a relative contraindication to laparoscopic/robotic partial nephrectomy, can also be cryoablated. Under general anaesthetic, the patient placed in the lateral position, laparoscopic ports are inserted and pnuemoperitoneum is secured. Similar to laparoscopic nephrectomy, the large bowel is mobilized medially to expose the Gerota’s fascia, which is opened to unveil the tumour. Intraoperative ultrasound imaging is obtained using a laparoscopic ultrasound probe to confirm the position and the dimensions of the tumour. Tumour biopsies are taken and the cryotherapy needles (probes) are placed into the tumour. The number of needles and the depth of placement are dependent on the size of the tumour. Temperature probes are placed to measure the freezing temperature achieved, one is placed in the centre of the tumour and the other about a centimetre beyond the tumour circumference. Typically, two freezing cycles with Argon and two thaw cycles with helium gas are achieved. The tumour is frozen and spectacular white mound is usually seen in laparoscopy (Fig. 1). After the procedure, the needles are removed and any bleeding is controlled by compression, which is usually effective. There are, however, minor variations with regards to the calibre of the needles and the techniques between different machines. Open surgical cryoablation can also be done if necessary.
Percutaneous Approach
Percutaneous techniques are developing rapidly and the numbers of patients treated are increasing. [20]. This is ideal for tumours, located in the posterior or inferior aspect of the kidney. Many centres still do them under general anaesthetic, as it is uncomfortable for patients to lie for long periods of time for the treatment. Techniques such as saline dissection to displace the bowel, adjacent to kidney, has paved the way for treating anterior and superior pole renal tumours safely and effectively by expert interventional radiologists (Figs. 2 and 3). The technique is usually CT-guided and less commonly is carried out using the MRI or ultrasound guidance. As will be expected, it is associated with lesser hospital stay than laparoscopy and is safer for patients with comorbidities. New imaging modalities are being researched to help improving probe placement and real-time intraoperative monitoring. For instance, real-time virtual ultrasonography (RVS) is an emerging modality that utilizes pre-operative CT scan data concomitantly with real-time intraoperative ultrasonography. It is an attempt to mitigate the deficiencies of the conventional ultrasound imaging such as limited visibility and inability of the ultrasound waves to travel through the ice resulting from the cryoablation [21].
Complications
One of the advantages of cryoablation is that it is minimally invasive and associated with less number of complications compared to open or laparoscopic partial nephrectomy and the majority of them are minor. In a multi-centre study published from Laguna et al. in which 148 cryoablations were performed in 144 patients, the majority of their reported perioperative complications were classified as Clavien–Dindo score 1 or 2 [22]. Complications reported included minor renal lacerations and bleeding from the needle placement site. The risk of renal fracture could be reduced with perpendicular placement of the needles and avoiding removal of them before complete thawing. The skin around the probe insertion site should be protected with gauze or insulating gel. In another study [23] of 139 patients, the most common minor complication was pain and paraesthesia at the site of the probe insertion. The rate of major complication was 1.8 % and included ileus, haemorrhage, conversion to open surgery, scarring with ureteropelvic junction obstruction and urinary leakage. More recently, the European Renal Cryoablation Group (EuRECA) published its retrospective review of 650 patients. The distribution of post-operative complications based on Clavien–Dindo, classification were grade I–II in 74 patients (11.3 %) and grade III–V in 20 patients (3.1 %) [24]. As established in laparoscopic partial nephrectomy, Radius, Endophytic, Nearness to collecting system, Anterior/posterior and Location (RENAL) nephrometry scores are also studied in laparoscopic cryoablation. As would be expected, the increasing RENAL score was associated linearly with the development of post-procedure complications in patients undergoing laparoscopic cryotherapy. This tool is considered useful in risk stratification but further work is necessary [25].
Follow-up
There is no single accepted protocol for follow-up following ablative therapy. Computed tomography (CT) scanning after the administration of contrast is the standard imaging modality. Cryoablation of renal tumour is considered a success if it does not enhance on imaging and shows regression in its size [11]. In our centre, we scan the ablated patients with contrast CT at 3 and 6 months after the procedure followed by imaging at six monthly intervals thereafter. Other centres use slightly differing protocols. Long-term follow-up is of paramount importance to make sure that therapy is successful with regression of tumour size and there is no recurrence. Contrast enhancement of tumour or increase in its size, are indicative of local recurrence. On the other hand, rim enhancement in a previously cryoablated tumour does not always mean the presence recurred especially if there is no increase in size [23]. However, if there is no satisfactory regression or whenever recurrence is suspected, image-guided biopsy is indicated [26].
Oncological Outcome
Both medium- and long-term data are showing that the oncological success for ablative therapy is promising with high efficiency and low morbidity. The 5- and 10-year cancer survival rates were 93 and 81 %, respectively [27]. Johnson and associates recently published their data of 112T1 SRM treated with laparoscopic cryoablation and followed up for more than 5 years. With the mean follow-up of 98 months, the cancer-specific survival was 98.5 % and progression-free survival 91 % and overall survival was 78 % [28]. The overall lower survival was thought to be due to comorbidities of these patients. The rate of treatment failure for cryoablation according to a meta-analysis ranged from 4.6 to 5.2 % and metastatic progression ranged from 1 to 1.2 % [29]. In the study by the EuRECA group of 650 patients, the estimated 3-, 5- and 8-year disease-free survival was 94, 92 and 79 %. The estimated 3-, 5- and 8-year cancer-specific survival was 99.4, 98.9 and 98.9 %. The estimated 3-, 5- and 8-year overall survival was 93.5, 86.3 and 66.5 %, respectively. On the whole, cryoablation appears to be a reasonable option with satisfactory outcomes especially in patients with comorbidities [24]. Recently, Zargar et al. performed a systematic review of cryotherapy of small renal masses and concluded that cryoablation had excellent functional outcome and low rate of complications. However, they suggested that patient selection criteria and oncological outcomes needed further study [10]. EuRECA is collecting prospective data from across Europe and will be able to throw more light in the coming years.
Renal Function Preservation
Renal function is not compromised and this is one of the advantages of the ablation techniques. There appears to be no detrimental loss of renal function even in patients with a single kidney. A recently published retrospective analysis by Woldu and colleagues concluded that ablative therapy modalities including cryoablation and RFA were associated with less renal parenchymal volume (RPV) loss compared to partial nephrectomy with its three modalities (open, laparoscopic and robot-assisted) [30]. It was also shown that renal function was maintained in patients with chronic kidney disease after they had cryoablation [31, 32]. There appears to be no detrimental loss of renal function even in patients with a single kidney in patients who had cryotherapy by laparoscopic technique [33] or by imaging-guided percutaneous treatment [32]. This point was also reiterated by the systematic review by Zarga et al. [10].
Radiofrequency Ablation
Radiofrequency ablative therapy was used to treat liver lesions and was first used in kidneys in 1997 [34]. It is mostly applied percutaneously, although, it can also be used laparoscopically [35]. In this technique, electrodes are inserted into the tumour and high-frequency electrical current is passed creating heat, which destroys the cancer cells. The tumour tissue along with a small margin around it is ablated by immediate direct cellular damage and delayed microvascular injury leading to permanent denaturation of the tissue protein. The tissue temperature has to be between 50 and 100 °C for adequate tissue destruction. A temperature of 105 °C or above will lead to patchy tissue damage. The main advantage of RFA is that it can be performed percutaneously under sedation avoiding the morbidity associated with general anaesthesia, laparoscopy and surgery (Fig. 4) However, the problem with the technique in real-time imaging using CT, MRI or ultrasound is considered unreliable [12] due to similarity between ablated tumour and normal tissue. Similar to cryotherapy, successfully ablated tumour show lack of enhancement on contrast imaging and regression in size in subsequent follow-up.
Oncological Outcome of RFA
Radiofrequency ablation is similar to cryotherapy in the lack of long-term data of their outcome. The recurrence-free survival rate was 90.3 % in a study that followed up SRMs in single kidneys treated with RFA for over 40 months [36]. Stern et al. published in their study disease-specific survival following RFA in T1a lesions of 93.4 % with a mean follow-up of 30 months. This was the same outcome for tumours of the same stage treated with partial nephrectomy [37]. In a large study of 243 procedures with a mean follow-up of 27 months, Tracey et al. [38] observed a 90 % 5-year recurrence-free survival in histologically proven renal cell cancer. Ramirez et al. [35] analysed the long-term oncological outcome of their SRMs treated with RFA. Seventy-nine patients had 111 renal masses treated over a 10-year period with a median follow up of 59 months. The estimated 5-year recurrence-free survival was 93.3 %, with a complication rate of 8.8 % of which 3.8 % were considered major. Psutka et al. [39] studied the long-term oncological outcomes for patients, with T1 renal cell cancers treated by RFA. This group had 185 patients, who were further categorized as T1a and T1b tumours. There were 143T1 tumours and 42 patients had T1b tumours. Tumour stage was the only significant predictor of disease-free survival in a multivariate analysis. At a median follow-up of 6.4 years, 93 % of T1a tumours and 76 % of T1b tumours were disease-free. There were six recurrences in the T1a group (4.2 %) and six in the T1b group (14.3 %) and the median time to recurrence was 2.5 years.
Which Is Better—Cryotherapy or RFA?
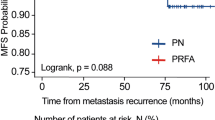
With both the ablative techniques well established, it is always a debate as to which of the modalities is better. As most of the RFA is performed under local anaesthetic with image guidance, it is suitable for patients who have comorbidity. Percutaneous cryotherapy is also evolving, although many groups still tend to do them under general anaesthetic. As discussed above, cryotherapy demonstrates observable treatment changes during the procedure, which is spectacular under laparoscopy. The oncological outcomes seem to favour cryotherapy over RFA. Available medium- and long-term data shows that cryoablation may have better tumour control and less risk of recurrence. Kunkel et al. showed in their meta-analysis of patients who had RFA and cryoablation for small renal tumours that pre-treatment biopsy was done more frequently in tumours treated with cryotherapy (82.3 %) than those treated with RFA (62.2 %) (P < 0.0001). They also showed that significantly higher number of tumours treated with RFA needed repeat ablations compared to cryotherapy (8.5 and 1.3 %, respectively) (P < 0.0001). In addition, the rate of local tumour progression was significantly higher for RFA (12.9 %) than for cryoablation (5.2 %) (P < 0.0001). RFA-treated group demonstrated more metastatic progression (2.5 %) than for cryoablation group [20]. In another meta-analysis, the same authors compared the outcome of nephron-sparing surgery, cryoablation and radiofrequency ablation in 99 studies that included 6471 renal masses. The SRMs treated with radiofrequency ablation showed a local recurrence rate of 11.7 % compared to 4.6 and 2.6 % for the masses treated with cryoablation and nephron sparing surgery, respectively [29]. Thompson et al. recently published retrospective analysis of 1803 CT1 renal masses treated in the Mayo clinic over a period of 11 years. The study included 1057 tumours treated with laparoscopic partial nephrectomy (PN), 187 treated with cryotherapy and 180 with radio frequency ablation (RFA). Their results showed that recurrence-free survival was similar in all the three treatment groups. The overall survival was superior in the PN group and metastasis-free survival was significantly lower in the RFA group [40]. That said, there was a selection bias with younger patient offered PN and it was an unmatched retrospective analysis [41].
High-Intensity Focused Ultrasound
This treatment modality utilizes the thermal effect resulted from focused high-intensity ultrasonic waves to induce coagulative necrosis in the target tissues. It also has a direct mechanical destructive effect coming from bubble implosion. Although the technique is completely non-invasive, high-intensity focused ultrasound (HIFU) ablation has disadvantages that include difficulty in localization of the lesions due to overlying rib and respiratory movement and has complications including bowel injury and skin burns [42].
Conclusion
Ablative therapy has emerged as a viable treatment options for SRMs with recurrence-free survival rates approaching that of extirpative surgery. The complication rate is minimal. Although PN remains the gold standard for treatment, ablation therapy could be a particularly useful alternative in patients who are not fit enough to have PN due to their comorbidities or when preservation of renal function is critical as in patients with single kidneys. Short- and medium-term follow-up data shows us that oncological outcomes of ablative therapy are promising. New technologies are being developed to aid accurate probe insertion, real-time monitoring and energy delivery to improve their efficacy. However there is no consensus in the literature on the best selection criteria and this needs further refinement. Prospective long-term data with regards to oncological control is still needed. Other ablation therapy modalities such as Cyber Knife, Interstitial LASER coagulation and Microwave thermotherapy remain largely experimental with lack of data to support their use at the time being.
References
Chow WH, Devesa SS, Warren JL, Fraumeni JF (1999) Rising incidence of renal cell cancer in the United States. JAMA 281(17):1628–1631
Crispen PL, Uzzo RG (2007) The natural history of untreated renal masses. BJU Int 99(5 Pt B):1203–1207. doi:10.1111/j.1464-410X.2007.06811.x
Chawla SN, Crispen PL, Hanlon AL, Greenberg RE, Chen DYT, Uzzo RG (2006) The natural history of observed enhancing renal masses: meta-analysis and review of the world literature. J Urol 175(2):425–431. doi:10.1016/S0022-5347(05)00148-5
Lee CT, Katz J, Shi W, Thaler HT, Reuter VE, Russo P (2000) Surgical management of renal tumors 4 cm. Or less in a contemporary cohort. J Urol 163(3):730–736
Lau WK, Blute ML, Weaver AL, Torres VE, Zincke H (2000) Matched comparison of radical nephrectomy vs nephron-sparing surgery in patients with unilateral renal cell carcinoma and a normal contralateral kidney. Mayo Clin Proc 75(12):1236–1242
McKiernan J, Simmons R, Katz J, Russo P (2002) Natural history of chronic renal insufficiency after partial and radical nephrectomy. Urology 59(6):816–820
Gill IS, Kavoussi LR, Lane BR, Blute ML, Babineau D, Colombo JR, Novick AC (2007) Comparison of 1,800 laparoscopic and open partial nephrectomies for single renal tumors. J Urol 178(1):41–46
Hadjipavlou M, Khan F, Fowler S, Joyce A, Keeley FX, Sriprasad S (2016) Partial vs radical nephrectomy for T1 renal tumours: an analysis from the British Association of Urological Surgeons Nephrectomy Audit. BJU Int 117(1):62–71
Gill IS (2003) Minimally invasive nephron-sparing surgery. Urologic Clin North Am 30(3):551–579
Zargar H, Atwell TD, Cadeddu JA, Jean J, Janetschek G, Kaouk JH, Matin SF, Polascik TJ, Zargar-Shoshtari K, Thompson RH (2016) Cryoablation for small renal masses: selection criteria, complications, and functional and oncologic results. Eur Urol 69(1):116–128
Khan F, Sriprasad S, Keeley FX (2012) Cryosurgical ablation for small renal masses, current status and future prospects. Brit J Med Surg Urol 5:S28–S34
Sriprasad S. and Marsh H. (2011). The management of small renal tumours by ablative therapies. INTECH Open Access Publisher
Rewcastle JC, Sandison GA, Saliken JC, Donnelly BJ, McKinnon JG (1999) Considerations during clinical operation of two commercially available cryomachines. J Surg Oncol 71(2):106–111
Acker JP, Larese A, Yang H, Petrenko A, McGann LE (1999) Intracellular ice formation is affected by cell interactions. Cryobiology 38(4):363–371. doi:10.1006/cryo.1999.2179
Bischof JC, Smith D, Pazhayannur PV, Manivel C, Hulbert J, Roberts KP (1997) Cryosurgery of dunning AT-1 rat prostate tumor: thermal, biophysical, and viability response at the cellular and tissue level. Cryobiology 34(1):42–69. doi:10.1006/cryo.1996.1978
Daum PS, Bowers WD, Tejada J, Hamlet MP (1987) Vascular casts demonstrate microcirculatory insufficiency in acute frostbite. Cryobiology 24(1):65–73
Clarke DM, Robilotto AT, Rhee E, VanBuskirk RG, Baust JG, Gage AA, Baust JM (2007) Cryoablation of renal cancer: variables involved in freezing-induced cell death. Technol Cancer Res Treat 6(2):69–79
Janzen N, Zisman A, Pantuck AJ, Perry K, Schulam P, Belldegrun AS (2002) Minimally invasive ablative approaches in the treatment of renal cell carcinoma. Current Urol Rep 3(1):13–20
Chodez M, Fiard G, Arnoux V, Descotes J-L, Long J-A (2015) Ablative treatments in localised renal cancer: literature review in 2014. Progrès en urologie : journal de l’Association française d'urologie et de la Société française d'urologie 25(9):499–509
Kunkle DA, Uzzo RG (2008) Cryoablation or radiofrequency ablation of the small renal mass: a meta-analysis. Cancer 113(10):2671–2680. doi:10.1002/cncr.23896
Autorino R, Haber G-P, White MA, Stein RJ, Kaouk JH (2010) New developments in renal focal therapy. J Endourol/Endourological Soc 24(5):665–672. doi:10.1089/end.2009.0643
Laguna MP, Beemster P, Kumar V, Kumar P, Klingler HC, Wyler S, de la Rosette JJ (2009) Perioperative morbidity of laparoscopic cryoablation of small renal masses with ultrathin probes: a European multicentre experience. Eur Urol 56(2):355–361
Lokken RP, Gervais DA, Arellano RS, Tuncali K, Morrison PR, Tatli S et al (2007) Inflammatory nodules mimic applicator track seeding after percutaneous ablation of renal tumors. AJR Am J Roentgenol 189(4):845–848. doi:10.2214/AJR.07.2015
Nielsen TK, Lagerveld BW, Keeley F, Lughezzani G, Sriprasad S, Barber NJ, Hansen LU, Larcher A, Guazzoni G, Van Der Zee JA, Ismail M (2016) 1094 outcomes after laparoscopic assisted renal cryoablation: a retrospective EuRECA multinational analysis. Eur Urol Suppl 3(15):e1094–e1094a
Sisul DM, Liss MA, Palazzi KL, Briles K, Mehrazin R, Gold RE, Masterson JH, Mirheydar HS, Jabaji R, Stroup SP, James OL (2013) RENAL nephrometry score is associated with complications after renal cryoablation: a multicenter analysis. Urology 81(4):775–780
Beemster P, Phoa S, Wijkstra H, de la Rosette J, Laguna P (2008) Follow-up of renal masses after cryosurgery using computed tomography; enhancement patterns and cryolesion size. BJU Int 101(10):1237–1242. doi:10.1111/j.1464-410X.2007.07437.x
Berger A, Kamoi K, Gill IS, Aron M (2009) Cryoablation for renal tumors: current status. Curr Opin Urol 19(2):138–142. doi:10.1097/MOU.0b013e328323f618
Johnson S, Pham KN, See W, Begun FP, Langenstroer P (2014) Laparoscopic cryoablation for clinical stage T1 renal masses: long-term oncologic outcomes at the Medical College of Wisconsin. Urology 84(3):613–618. doi:10.1016/j.urology.2014.03.055
Kunkle DA, Egleston BL, Uzzo RG (2008) Excise, ablate or observe: the small renal mass dilemma—a meta-analysis and review. J Urol 179(4):1227–1233 . doi:10.1016/j.juro.2007.11.047discussion 1233–4
Woldu SL, Thoreson GR, Okhunov Z, Ghandour R, Rothberg MB, RoyChoudhury A et al (2015) Comparison of renal parenchymal volume preservation between partial nephrectomy, cryoablation, and radiofrequency ablation using 3D volume measurements. J Endourol/ Endourological Soc 29(8):948–955. doi:10.1089/end.2014.0866
Michaels MJ, Rhee HK, Mourtzinos AP, Summerhayes IC, Silverman ML, Libertino JA (2002) Incomplete renal tumor destruction using radio frequency interstitial ablation. J Urol 168(6):2406–2409 . doi:10.1097/01.ju.0000037915.89846.b6discussion 2409–10
Altunrende F, Autorino R, Hillyer S, Yang B, Laydner H, White MA et al (2011) Image guided percutaneous probe ablation for renal tumors in 65 solitary kidneys: functional and oncological outcomes. J Urol 186(1):35–41. doi:10.1016/j.juro.2011.03.024
Khan F, Mahmalji W, Madaan S, Dickinson IK, Keeley FX, Lagerveld BW, Sriprasad S, (2013). Multi-institutional analysis of renal function following cryoablation of small renal masses in solitary kidneys. In BJU INTERNATIONAL (Vol. 111, pp. 37–37). 111
Weight CJ, Fergany AF, Gunn PW, Lane BR, Novick AC (2008) The impact of minimally invasive techniques on open partial nephrectomy: a 10-year single institutional experience. J Urol 180(1):84–88. doi:10.1016/j.juro.2008.03.049
Ramirez D, Ma YB, Bedir S, Antonelli JA, Cadeddu JA, Gahan JC (2014) Laparoscopic radiofrequency ablation of small renal tumors: long-term oncologic outcomes. J Endourol 28(3):330–334
Levinson AW, Su L-M, Agarwal D, Sroka M, Jarrett TW, Kavoussi LR, Solomon SB (2008) Long-term oncological and overall outcomes of percutaneous radio frequency ablation in high risk surgical patients with a solitary small renal mass. J Urol 180(2):499–504 . doi:10.1016/j.juro.2008.04.031discussion 504
Stern JM, Svatek R, Park S, Hermann M, Lotan Y, Sagalowsky AI, Cadeddu JA (2007) Intermediate comparison of partial nephrectomy and radiofrequency ablation for clinical T1a renal tumours. BJU Int 100(2):287–290. doi:10.1111/j.1464-410X.2007.06937.x
Tracy CR, Raman JD, Donnally C, Trimmer CK, Cadeddu JA (2010) Durable oncologic outcomes after radiofrequency ablation. Cancer 116(13):3135–3142
Psutka SP, Feldman AS, McDougal WS, McGovern FJ, Mueller P, Gervais DA (2013) Long-term oncologic outcomes after radiofrequency ablation for T1 renal cell carcinoma. Eur Urol 63(3):486–492
Thompson RH, Atwell T, Schmit G, Lohse CM, Kurup AN, Weisbrod A et al (2015) Comparison of partial nephrectomy and percutaneous ablation for cT1 renal masses. Eur Urol 67(2):252–259. doi:10.1016/j.eururo.2014.07.021
Kutikov A, Smaldone MC, Uzzo RG (2015) Focal therapy for treatment of the small renal mass: dealer’s choice or a therapeutic gamble? Eur Urol 67(2):260–261. doi:10.1016/j.eururo.2014.08.034
Marberger M, Schatzl G, Cranston D, Kennedy JE (2005) Extracorporeal ablation of renal tumours with high-intensity focused ultrasound. BJU Int 95(Suppl 2):52–55. doi:10.1111/j.1464-410X.2005.05200.x
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Farrag, K., Sriprasad, S. Non-Surgical Ablative Therapy for Management of Small Renal Masses—Current Status and Future Trends. Indian J Surg Oncol 8, 39–45 (2017). https://doi.org/10.1007/s13193-016-0598-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-016-0598-x