Abstract
Purpose
To assess the accuracy of gadobenate-enhanced MRI for predicting microvascular invasion (MVI) in patients operated for hepatocellular carcinoma (HCC).
Methods
The 164 patients who met the inclusion criteria were assigned to one of two groups: the MVI-positive group and the MVI-negative group. Imaging results were compared between the two groups using the Kruskal test, chi-square test, independent sample t test, and logistic regression analysis.
Results
Differences in the capsule (p = 0.037) and margin (p = 0.004) of the tumor, rim enhancement (p = 0.002), peritumoral enhancement in the arterial phase (p < 0.001), and peritumoral hypointensity in the hepatobiliary phase (HBP) (p < 0.001) were statistically significant. The results of multivariate analysis identified rim enhancement in the arterial phase (odds ratio (OR) = 2.115; 95% confidence interval (CI), 1.002–4.464; p = 0.049) and peritumoral hypointensity in the HBP (OR = 5.836; 95% CI, 2.442–13.948; p < 0.001) as independent risk factors for MVI. Use of the two predictors in combination identified 32.79% (20/61) of HCCs with MVI with a specificity of 95.15% (98/103).
Conclusions
Rim enhancement in the arterial phase and peritumoral hypointensity in the HBP were identified as independent risk factors for MVI in patients with HCC.
Key Points
• Rim enhancement in the arterial phase and peritumoral hypointensity in the hepatobiliary phase were independent risk factors for microvascular invasion in patients with HCC.
• Use of the two predictors in combination had a sensitivity of 32.79% and a specificity of 95.15% for predicting microvascular invasion.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Microvascular invasion (MVI) is an important predictor of hepatocellular carcinoma (HCC) recurrence after surgical resection or liver transplantation, particularly recurrence during the early period [1,2,3,4,5]. Predicting MVI using preoperative imaging indicators would be of great clinical significance. Recent studies reported that certain imaging manifestations may help the preoperative diagnosis of MVI, including size, capsule, margin, signal intensity (SI) ratio of the tumor, apparent diffusion coefficient (ADC) values, peritumoral enhancement and rim enhancement in the arterial phase, and peritumoral hypointensity of the tumor in the hepatobiliary phase (HBP) of gadoxetate disodium–enhanced MRI [6,7,8,9,10,11,12,13,14]. An et al reported that both rim enhancement and peritumoral enhancement in the arterial phase are independent risk factors for MVI and HCC recurrence [7]. Lee et al [9] demonstrated that arterial peritumoral enhancement, non-smooth tumor margin, and peritumoral hypointensity on gadoxetic acid–enhanced HBP images were independent and significant predictors of MVI in HCC. However, there is no clinical consensus regarding the optimal imaging parameter for predicting MVI accurately.
Gadobenate dimeglumine (Gd-BOPTA) is a biphasic T1-weighted MRI contrast agent characterized by nonspecific distribution in the extracellular space and specific uptake in hepatocytes. This agent can be used not only for dynamic contrast–enhanced (DCE) MRI of the liver but also for specific imaging in the HBP within 40 to 120 min after being injected. However, no research on predicting MVI using Gd-BOPTA-enhanced MR imaging manifestations has been reported.
Here, we evaluated the diagnostic efficacy of Gd-BOPTA-enhanced MRI imaging signs for predicting MVI in patients operated for HCC.
Materials and methods
Patients
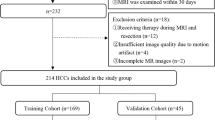
A retrospective study was performed including 463 patients who underwent MRI scan in Shanghai Eastern Hepatobiliary Hospital between September 2016 and June 2017.
The inclusion criteria were as follows: (1) 18–80 years old; (2) liver tumors of more than 1 cm in diameter as determined by MR images; (3) Gd-BOPTA-enhanced MRI scan including complete arterial phase, portal phase, delayed phase, and HBP examination recording; (4) surgical removal of the tumor; and (5) HCC diagnosed by postoperative pathology (Fig. 1).
MRI scan
MRI was performed with the GE Optima MR360 1.5 T with an 8-channel abdominal coil. All patients fasted for 4 h before the scan. Gd-BOPTA (MultiHance, Bracco) at 0.1 mmoL/kg was injected into patients’ median cubital veins at a flow rate of 2.0 mL/s with a high-pressure syringe. The enhanced scan of the arterial, portal, and delayed phases was performed at 22–25 s, 50–60 s, and 90–120 s after the injection of Gd-BOPTA, respectively. Scanning at the HBP in patients with normal liver function and those with impaired function was performed at 60 min and 120 min after the injection of the contrast agent, respectively. The definition of impaired liver function was performed based on the clinical assessment by the referring physicians.
Table 1 summarizes the scanners and scanning parameters. FIESTA, T1WI (in-phase/opposed-phase), and fat-suppressed T2-weighted images were acquired. Dynamic contrast–enhanced MRI was performed using Gd-BOPTA, and the 3D-LAVA (Liver Acquisition with Volume Acceleration) technique was used.
Clinical and imaging data analysis
Clinical data were obtained from the electronic patients’ records. The MR imaging manifestations were analyzed by two radiologists, both with more than 10 years of experience in abdominal imaging, working in consensus. The clinical parameters assessed included patient gender, age, protein induced by vitamin K absence/antagonist-II (PIVKA-II), alpha-fetoprotein (AFP), HBsAg, HBeAg, and cirrhosis. Imaging parameters included intratumoral fat, rim and peritumoral enhancement in the arterial phase, hypointensity, and peritumoral hypointensity in the HBP.
The Liver Imaging Reporting and Data System (2017) (LI-RADS-2017) was used as the reference standard for assessments of tumor size, capsule, and margins [15]. The size of a tumor was determined across the longest diameter of the largest plane of the mass including the capsule. Tumor margins were defined as smooth or non-smooth, with the latter demonstrating peritumoral buds on transverse and coronal HBP images [8]. The presence of intratumoral fat was defined as a fat fraction (FF) of > 5%, which was calculated using the following formula: FF = (in-phase − opposed-phase)/2 × in-phase [16]. The capsule refers to the smooth peripheral hyperenhancement in the portal venous or delayed phases [17]. Peritumoral enhancement in the arterial phase was defined as a crescent or polygonal enhanced region outside the margin of the tumor showing extensive contact with the margin and similar signal intensity to that of the normal liver parenchyma in the delayed phase [18]. Peritumoral hypointensity in the HBP refers to a wedge-shaped or flame-like hypointensity area outside the margin compared with that of the normal liver parenchyma [11].
Pathological analysis
All tumor sections were reexamined by an experienced pathologist with 21 years of experience in pathological diagnosis of liver cancers. The WHO Classification of Tumors of the Digestive System (2010) [19] defines MVI as the presence of cancer cell nests in the vascular lumen lined by endothelial cells under the microscope, which is dominated by branches of portal veins (including blood vessels inside the capsule). The cases were divided into MVI-positive and MVI-negative groups. Cirrhosis of the liver was diagnosed by the pathologist during the histopathological examination of hepatocellular carcinoma.
Statistical analysis
Categorical data were analyzed using the chi-square test or Fisher’s exact test, and continuous variables were analyzed using analysis of variance or the Kruskal-Wallis H test for variables with an abnormal distribution and homogeneity of variance. Univariate logistic regression was used to identify independent predictors of MVI. Variables identified as significant in the univariate analysis were included in the multivariate analysis model. After considering the effect of capsule, arterial rim enhancement, arterial peritumoral enhancement, tumor margin, peritumoral hypointensity in the HBP, and shape, the adjusted odds ratio (OR), and 95% confidence interval (CI) were estimated. All statistical tests were two-sided, and p values of < 0.05 were considered statistically significant. Data compilations and descriptive statistics were performed using SPSS 19.0 for Windows (IBM).
Results
Clinical data and laboratory examination
Overall, 164 patients met the inclusion criteria. The median interval between MRI examination and surgery was 9 days for all patients, and the longest interval was 16 days.
There were 125 patients in the normal liver function group and 39 patients in the impaired liver function group. The average age was 55.9 ± 10.31 years, and the male-to-female ratio was 139:25 (Table 2). There were 61 patients in the MVI-positive group and 103 in the MVI-negative group. In the MVI-positive group, the male-to-female ratio was 53:8, and the average age was 56.77 ± 10.12 years; in the MVI-negative group, the ratio was 86:17, and the average age was 55.38 ± 10.43 years. There were no statistically significant differences in the average age, male-to-female ratio, size and number of tumors, liver nodules, cirrhosis, and the levels of AFP and PIVKA-II in the serum between the two groups (p > 0. 05).
Gd-BOPTA-enhanced MR imaging manifestations
The differences in the shape of tumors and intratumoral fat between the two groups were not statistically significant (p = 0.166). There were statistically significant differences between the MVI-positive group and MVI-negative group in the capsule (16% vs. 31%, respectively, p = 0.037) and non-smooth margin (67% vs. 44%, respectively, p = 0.004) (Figs. 2 and 3) of tumors, rim enhancement (62% vs. 38%, respectively, p = 0.002; Fig. 4), and peritumoral enhancement (23% vs. 5%, respectively, p < 0.001) (Figs. 2 and 3, red arrow) in the arterial phase. In the HBP, there was a statistically significant difference in peritumoral hypointensity between the MVI-positive group and MVI-negative group (48% vs. 10%, respectively, p < 0.001), whereas the difference in intratumoral hypointensity in the HBP was not statistically significant (90% vs. 92%, respectively, p = 0.647).
HCC presenting with MVI in a 59-year-old man. a Unevenly high signals on T2WI; b, c Slight heterogeneous enhancement (black arrow) on the arterial phase with washout and non-smooth margin on the delayed phase. d Non-smooth tumor margin and peritumoral hypointensity (red arrow) in the hepatobiliary phase
HCC with MVI in a 48-year-old man. a The lesion is moderately hyperintense and well-delineated in the liver parenchyma on T2WI. b, c It shows clear homogeneous arterial phase hyperenhancement with washout on the delayed phase and enhancing capsule. d On the HBP image, the lesion is hypointense and well-delineated in liver parenchyma, and shows a peripheral tumor node
Multivariate analysis identified rim enhancement in the arterial phase (OR = 2.115; 95% CI, 1.002–4.464; p = 0.049) and peritumoral hypointensity in the HBP (OR = 5.836; 95% CI, 2.442–13.948; p = 0.001) as independent risk factors for MVI (Table 3).
The results of logistic regression analysis indicated that two imaging features could help predict MVI: the rim enhancement of the tumor in the arterial phase and peritumoral hypointensity in the HBP. The sensitivity, specificity, accuracy, PPV, and NPV of each feature and their combination for predicting MVI are listed in Table 4. When the two features were used simultaneously, they were combined in two ways as follows: either feature was positive for MVI (parallel connection) or both features were positive for MVI (serial connection). The parallel connection identified 78.69% (48/61) of HCCs with MVI with a specificity of 56.31%. The serial connection method identified 32.79% (20/61) of HCCs with MVI with a specificity of 95.15%. As shown in Table 4, the serial connection method had a higher specificity and PPV than the parallel connection method.
Discussion
The present study showed that rim enhancement in the arterial phase and peritumoral hypointensity in the HBP were independent risk factors for MVI in patients with HCC. MVI is an important factor in predicting the recurrence of HCC after surgical resection. Patient gender, age, tumor size, the levels of serum PIVKA-II and AFP, hepatitis B infection, and cirrhosis did not differ significantly between the MVI-positive and MVI-negative groups in our study. Biochemical indicators, diseases associated with HCC, and tumor size were not useful for predicting MVI before surgery. Large tumor size generally indicates that MVI is more likely to occur in HCC. However, the usefulness of tumor size alone for predicting MVI in HCC is controversial [6], and these conflicting results could be attributed to selection bias. In the present cohort, tumor lesions larger than 5 cm accounted for 64% (106/164). Future studies should include a larger number of patients with tumors of different sizes, which may increase the value of tumor size for predicting MVI.
Several studies have investigated ways to predict MVI using MR imaging manifestations, such as the diameter and margins of the lesion, enhancing mode, and DWI signals before surgical resection of HCC. The use of gadoxetic acid disodium, a hepatocyte-specific contrast agent, in the clinical setting led to studies investigating the effect of MR imaging manifestations (such as signal intensity and peritumoral hypointensity in the HBP) to try to predict the occurrence of MVI before surgical resection of HCC [6,7,8,9,10].
The HCC capsule as an imaging manifestation refers to the proliferating fibrous connective tissues encircling the tumor, which are caused by the growth of the tumor. The capsule is actually a “pseudo-capsule” because it does not contain epithelial tissues. One study [20] reported that the presence of a capsule in live tumors is an indicator of a poor prognosis, whereas another report [21] indicated that the fibrous “pseudo-capsule” may help limit the growth of cancers, thereby predicting a good prognosis. Our data indicated that capsules are more likely to occur in MVI-negative patients. The difference in the presence of a capsule was statistically significant between the two groups (p = 0.037). The results of univariate analysis demonstrated that the absence of a capsule is a risk factor for MVI (p = 0. 040). However, the results of multivariate analysis showed that it was not an independent risk factor (p = 0.550), namely, the absence of a capsule was not an indicator of the occurrence of MVI.
Previous studies [22,22,23,24,26] reported that the occurrence of MVI can be predicted by assessing the characteristics of the margin and that a non-smooth margin is an independent risk factor for MVI. In the present study, the results of univariate analysis indicated that a non-smooth margin is an indicator of MVI, whereas multivariate analysis showed that it is not an independent risk factor for MVI, which was similar to a previous report [27]. We classified tumors into round, oval, lobular, and irregular to explore the association between the shape of tumors and MVI. The results showed no statistically significant differences in the shape of tumors between the two groups (p = 0.964). The effect of tumor shape on predicting MVI needs to be further evaluated in future studies.
In the present study, there was no statistically significant difference in the lipid ratio between the two groups (p = 0.166). We speculate that MVI may be caused by insufficient peripheral arterial blood supply resulting from damaged peritumoral hepatocytes (as indicated by peritumoral hypointensity in the HBP) and obstructed drainage veins.
Rim enhancement of a tumor in the arterial phase indicated invasive growth in the absence of the capsule, the occurrence of MVI, and rapid growth with central necrosis. Peritumoral enhancement in the arterial phase indicated enhancement of the normal peritumoral hepatic parenchyma. This was caused by hemodynamic changes of the surrounding hepatic parenchyma, decreased blood supply in the portal vein, and increased blood supply in the arteries when the small peritumoral blood vessels are invaded by HCC. In the present study, the incidence of rim enhancement and peritumoral enhancement in the arterial phase was higher in the MVI-positive group than that in the MVI-negative group, and the difference was statistically significant (p = 0.002; p < 0.001). The results of univariate analysis identified the two predictors as risk factors for MVI (p = 0.003; p = 0.001); however, multivariate analysis indicated that rim enhancement, but not peritumoral enhancement, is an independent risk factor for MVI, which is not consistent with the findings of previous studies. Several studies have shown that peritumoral enhancement in the arterial phase is associated with MVI [18, 28]. An et al demonstrated that both rim enhancement and peritumoral enhancement in the arterial phase are independent risk factors for MVI and HCC recurrence [7]. Lee et al reported that peritumoral enhancement in the arterial phase is an independent risk factor for MVI, whereas rim enhancement is not [9]. These discrepancies could be attributed to sample bias or differences in sample size. Future studies should include additional cases with Gd-BOPTA-enhanced MRI data to clarify which clinical and imaging indicators are stable and reliable independent predictors of MVI.
Manifestations on the HBP images of Gd-BOPTA-enhanced MRI reflect the function of hepatocytes. HCC cells, which originate from hepatocytes, cannot absorb Gd-BOPTA in the HBP. This causes intratumoral hypointensity in this phase. In this study, the difference in the occurrence of intratumoral hypointensity in the HBP between the two groups was not statistically significant (55/61 vs. 95/103; p = 0.647), whereas the difference in the incidence of peritumoral hypointensity in the HBP was statistically significant (p < 0.001). Peritumoral hypointensity in the HBP suggested that the liver cells around the tumor were damaged and their metabolic function was impaired. Peritumoral hypointensity was more frequent in the MVI-positive group. The results of univariate and multivariate analyses showed that peritumoral hypointensity in the HBP was an independent risk factor for MVI, which is consistent with previous reports [9, 10].
Combined with the findings of previous studies, the present results indicated that rim enhancement in the arterial phase and peritumoral hypointensity in the HBP were independent risk factors for MVI in patients with HCC. Simultaneous use of the two features identified 32.79% (20/61) of HCCs with MVI with a specificity of 95.15% (98/103).
The present study had several limitations. Firstly, patients with multicentric (or very large) tumors who are not surgical candidates could not be included in the study, which may decrease the value of certain risk factors for predicting the incidence of MVI. This could explain the relatively low incidence of MVI in the present series. Secondly, we did not compare the two groups in terms of ADC values because of retrospective design; we failed to enforce the scanning of DWI data from all the patients with sufficient quality, in which 13 patients did not have DWI imaging during initial scan protocol for reasons like motion artifacts from inadequate breathholding. In addition, the relatively high incidence of rim enhancement in the arterial phase (77/164) in this study may have led to false ADC values. Moreover, the determination of accurate ADC values may be affected by the large average tumor size (40 mm), large areas of necrosis, cystic degeneration, and hemorrhage in the central areas of the large tumors with relatively small areas of intratumor parenchymal tissue. Relatively few patients can accurately measure ADC values and may introduce a selection bias. Finally, another limitation of the study was the lack of inter-observer evaluation. The original aim of this study was to verify that MVI has certain imaging signs; therefore, discrepancies between the observers’ first impressions were not recorded. The agreement between observers needs to be tested in future studies.
A larger sample and follow-up are needed to reduce the bias caused by the low rate of MVI-positive cases and to verify the association between the imaging manifestations and HCC prognosis and recurrence.
Conclusion
Rim enhancement in the arterial phase and peritumoral hypointensity in the HBP were identified as independent risk factors for MVI. When the two factors were used in combination, the specificity of MVI prediction in HCC reached 95.15%.
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- AFP:
-
Alpha-fetoprotein
- DCE:
-
Dynamic contrast-enhanced
- Gd-BOPTA:
-
Gadobenate dimeglumine
- HBP:
-
Hepatobiliary phase
- HCC:
-
Hepatocellular carcinoma
- MVI:
-
Microvascular invasion
- PIVKA-II:
-
Protein Induced by Vitamin K Absence or Antagonist-II
- SI:
-
Signal intensity
References
Banerjee S, Wang DS, Kim HJ et al (2015) A computed tomography radiogenomic biomarker predicts microvascular invasion and clinical outcomes in hepatocellular carcinoma. Hepatology 62:792–800
Lee S, Kim KW, Jeong WK et al (2019) Gadoxetic acid–enhanced MRI as a predictor of recurrence of HCC after liver transplantation. Eur Radiol 30:987–995
Wei Y, Huang ZX, Tang HH et al (2019) IVIM improves preoperative assessment of microvascular invasion in HCC. Eur Radiol 29:5403–5414
Feng ST, Jia YM, Liao B et al (2019) Preoperative prediction of microvascular invasion in hepatocellular cancer: a radiomics model using Gd-EOB-DTPA-enhanced MRI. Eur Radiol 29:4648–4659
Ahn SY, Lee JM, Joo I et al (2015) Prediction of microvascular invasion of hepatocellular carcinoma using gadoxetic acid-enhanced MR and (18) FFDG PET/CT. Abdom Imaging 40:843–851
Renzulli M, Brocchi S, Cucchetti A et al (2016) Can current preoperative imaging be used to detect microvascular invasion of hepatocellular carcinoma? Radiology 279:432–442
An C, Kim DW, Park YN, Chung YE, Rhee H, Kim MJ (2015) Single hepatocellular carcinoma: preoperative MR imaging to predict early recurrence after curative resection. Radiology 276:433–443
Ariizumi S, Kitagawa K, Kotera Y et al (2011) A non-smooth tumor margin in the hepatobiliary phase of gadoxetic acid disodium (Gd-EOB-DTPA)-enhanced magnetic resonance imaging predicts microscopic portal vein invasion, intrahepatic metastasis, and early recurrence after hepatectomy in patients with hepatocellular carcinoma. J Hepatobiliary Pancreat Sci 18:575–585
Lee S, Kim SH, Lee JE (2017) Preoperative gadoxetic acid–enhanced MRI for predicting microvascular invasion in patients with single hepatocellular carcinoma. J Hepatol 67:526–534
Kim JY, Kim MJ, Kim KA, Jeong HT, Park YN (2012) Hyperintense HCC on hepatobiliary phase images of gadoxetic acid-enhanced MRI: correlation with clinical and pathological features. Eur J Radiol 81:3877–3882
Kim KA, Kim MJ, Jeon HM et al (2012) Prediction of microvascular invasion of hepatocellular carcinoma: usefulness of peritumoral hypointensity seen on gadoxetate disodium-enhanced hepatobiliary phase images. J Magn Reson Imaging 35:629–634
Suh YJ, Kim MJ, Choi JY, Park MS, Kim KW (2012) Preoperative prediction of the microvascular invasion of hepatocellular carcinoma with diffusion-weighted imaging. Liver Transpl 18:1171–1178
Xu P, Zeng M, Liu K, Shan Y, Xu C, Lin J (2014) Microvascular invasion in small hepatocellular carcinoma: is it predictable with preoperative diffusion-weighted imaging? J Gastroenterol Hepatol 29:330–336
Okamura S, Sumie S, Tonan T et al (2016) Diffusion weighted magnetic resonance imaging predicts malignant potential in small hepatocellular carcinoma. Dig Liver Dis 48:945–952
Elasyes KM, Hooker JC, Agrons MM et al (2017) Version of LI-RADS for CT and MR imaging: an update. Radiographics. 37:1994–2017
Reeder SB, Sirlin CB (2010) Quantification of liver fat with magnetic resonance imaging. Magn Reson Imaging Clin N Am 18:337–357
Choi JY, Lee JM, Sirlin CB (2014) CT and MR imaging diagnosis and staging of hepatocellular carcinoma: part II. Extracellular agents, hepatobiliary agents, and ancillary imaging features. Radiology 273:30–50
Kim H, Park MS, Choi JY et al (2009) Can microvessel invasion of hepatocellular carcinoma be predicted by pre-operative MRI? Eur Radiol 19:1744–1751
Bosman F, Carneiro F, Hruban R (2010) WHO classification tumours of the digestive system. IARC Press, Lyon
Zhang J, Liu XJ, Zhang HP et al (2019) Texture analysis based on preoperative magnetic resonance imaging (MRI) and conventional MRI features for predicting the early recurrence of single hepatocellular carcinoma after hepatectomy. Acad Radiol 26:1164–1173
Ng IO, Lai EC, Ng MM, Fan ST (1992) Tumor encapsulation in hepatocellular carcinoma. A pathologic study of 189 cases. Cancer 70:45–49
Nakashima Y, Nakashima O, Tanaka M, Okuda K, Nakashima M, Kojiro M (2003) Portal vein invasion and intrahepatic micrometastasis in small hepatocellular carcinoma by gross type. Hepatol Res 26:142–147
Eguchi S, Takatsuki M, Hidaka M et al (2010) Predictor for histological microvascular invasion of hepatocellular carcinoma: a lesson from 229 consecutive cases of curative liver resection. World J Surg 34:1034–1038
Nagano Y, Shimada H, Takeda K et al (2008) Predictive factors of microvascular invasion in patients with hepatocellular carcinoma larger than 5 cm. World J Surg 32:2218–2222
Chou CT, Chen RC, Lee CW et al (2012) Prediction of microvascular invasion of hepatocellular carcinoma by preoperative CT imaging. Br J Radiol 85:778–783
Wu TH, Hatano E, Yamanaka K et al (2016) A non-smooth tumor margin on preoperative imaging predicts microvascular invasion of hepatocellular carcinoma. Surg Today 46:1275–1281
Hu HT, Wang Z, Huang XW et al (2018) Ultrasound-based radiomics score: a potential biomarker for the prediction of microvascular invasion in hepatocellular carcinoma. Eur Radiol 29:2890–2901
Miyata R, Tanimoto A, Wakabayashi G et al (2006) Accuracy of preoperative prediction of microinvasion of portal vein in hepatocellular carcinoma using superparamagnetic iron oxide–enhanced magnetic resonance imaging and computed tomography during hepatic angiography. J Gastroenterol 41:987–995
Acknowledgments
We would like to thank the whole study team at 4 hospitals, for continuous support.
Funding
This study has received funding from the Natural Science Foundation of Guangdong Province (2018A030313951), the Foundation of President of Nanfang Hospital (2017C011), the National Science and Technology Major Project (2018ZX10302207-004), the China Medical Research Fund of Guangdong Province (A2017496).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Chenguang Wang.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Professor Cairong Zhu kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was not required for this study because Gd-BOPTA had been widely used in MRI scan as a contrast agent.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, L., Yu, X., Wei, W. et al. Prediction of HCC microvascular invasion with gadobenate-enhanced MRI: correlation with pathology. Eur Radiol 30, 5327–5336 (2020). https://doi.org/10.1007/s00330-020-06895-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06895-6