Abstract
Objectives
To measure the frequency of infraorbital nerve enlargement (IONE) on magnetic resonance imaging (MRI) in European patients suffering from an IgG4-related ophthalmic disease (IgG4-ROD) as compared to patients suffering from non-IgG4-related ophthalmic disease (non-IgG4-ROD).
Methods
From January 2006 through April 2015, 132 patients were admitted for non-lymphoma, non-thyroid-related orbital inflammation. Thirty-eight had both pre-therapeutic orbital MRI and histopathological IgG4 immunostaining. Fifteen patients were classified as cases of IgG4-ROD and 23 patients as cases of non-IgG4-ROD. Two readers performed blinded analyses of MRI images. The main criterion was the presence of an IONE, defined as the infraorbital nerve diameter being greater than the optic nerve diameter in the coronal section.
Results
IONE was present in 53% (8/15) of IgG4-ROD cases whereas it was never present (0/23) in cases of non-IgG4-ROD (P < 0.0001). IONE was only present in cases where, on MRI, the inflammation of the inferior quadrant was present and in direct contact with the ION canal.
Conclusions
In European patients suffering from orbital inflammation, the presence of IONE on an MRI is a specific sign of IgG4-ROD. Recognition of this pattern may facilitate the accurate diagnosis for clinicians and allow for the adequate management and appropriate care of their patients.
Key points
• IONE on an MRI is a specific sign of IgG4-ROD.
• IONE recognition allows for a quicker diagnosis and appropriate management.
• IONE appears when inflammation is in direct contact with the ION canal.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
IgG4-related disease (IgG4-RD) is a rare systemic condition that was identified relatively recently [1, 2]. The estimated prevalence of IgG4-RD in Japan ranges from 0.28 to 1.08 per 100,000 inhabitants [2]. IgG4-RD has been found responsible for fibroinflammatory lesions of numerous organs and anatomical regions such as the pancreas, liver, biliary tract, salivary glands, lymph nodes, orbits, kidneys, and lungs [1–6]. Two main pathological signs characterise IgG4-RD: a dense lymphoplasmacytic infiltrate by cells expressing IgG4 and storiform fibrosis [7]. The pathophysiology of IgG4-RD is still poorly understood. It is most plausibly an autoimmune disease involving both humoral and cellular immunity [5]. The orbital part of IgG4-RD is known as an IgG4-related ophthalmic disease (IgG4-ROD). IgG4-ROD concerns 4%-34% of patients suffering from IgG4-RD [8–10], the orbital region being the first most frequent site of the head and neck region to be involved in IgG4-RD [11]. A non-negligible part (6%-40%) of orbital inflammation cases formerly considered idiopathic are in fact cases of IgG4-ROD [8, 12–14]. IgG4-ROD usually presents with an involvement of the lacrimal gland (dacryoadenitis), extraocular muscles (myositis), and/or the intraorbital fat. It is currently noted that IgG4-RD has a particular tropism for cranial nerves [15–17]. Recent publications indicate a close association between the infiltration of the branches of the trigeminal nerve, particularly its infraorbital branch, and the diagnosis of IgG4-ROD [6, 18–21]. The infraorbital nerve enlargement (IONE) is considered a key sign of IgG4-ROD, according to the Japanese Study Group for IgG4-ROD [22]. Other radiological features of IgG4-ROD are non-specific and appear comparable to any other orbital inflammation. Therefore, IONE appears particularly promising to identify IgG4-ROD.
However, most studies conducted to date mainly included Asian patients, and the reproducibility of those findings in other ethnic groups remains unproven. The aim of our study was to evaluate the prevalence of IONE in European patients with histologically proven IgG4-ROD as compared with non-IgG4-related ophthalmic disease (non-IgG4-ROD).
Materials and methods
Study design and setting
We conducted a retrospective systematic chart review in a tertiary referral centre specialising in ophthalmology diseases.
Ethical approval, patient information, and consent
This study was prospectively approved by our institutional Research Ethics Board and adhered to the tenets of the Declaration of Helsinki. All patients were contacted at the time of the study and informed in writing of its aims and methods. They were given the opportunity to express their refusal to have their medical records used for the study.
Patients
We aimed at reviewing the medical charts and magnetic resonance imaging (MRI) of adult patients suffering from orbital inflammation treated in our centre from January 2006 through April 2015.
Inclusion criteria were:
-
Patient aged 18 and older
-
The presence of a clinical orbital inflammation: mass/swelling, pain, exophthalmos, visual loss, ptosis, or diplopia.
-
The presence of at least one pretherapeutic MRI confirming the inflammation of one or more orbital structures: the lacrimal gland, fat, muscles, or ION. The mandatory minimal MRI protocol included the following sequences: T1- and T2-weighted MR image, in the transverse and coronal plane, and a fat-suppressed T1-weighted MR image in the coronal plane obtained after intravenous administration of a gadolinium chelate.
-
Completion of at least one orbital biopsy with a pathologic examination and an immunohistochemical screen for IgG4.
Exclusion criteria were:
-
Clinical and biological signs of thyroid-associated orbitopathy
-
Histologically proven lymphoma
-
A pretherapeutic MRI that is insufficient for an adequate interpretation
-
The absence of IgG4 testing in the pathology examination
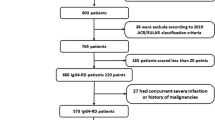
A flowchart illustrating the selection of patients is shown in Table 1. From January 2006 through April 2015, 1438 patients consulted in our hospital for orbital inflammation. We excluded 987 patients with thyroid-associated orbitopathy and 319 patients with histologically proven lymphoma. Out of the remaining 132 patients, 94 did not meet the inclusion criteria. Finally, 38 patients were included in the study.
Review of clinical charts
All patients’ medical charts were systematically reviewed to retrieve the following clinical data:
-
The laterality of orbital inflammation (left, right, or bilateral)
-
The presence or absence of each of the following clinical signs: a mass, swelling, visual loss, diplopia, ptosis, and exophthalmos
Review of histopathological data
The pathology slides of each patient were re-read by two senior pathologists and each patient was subsequently classified as either with IgG4-ROD or with non-IgG4-ROD, in compliance with the 2011 Umehara diagnostic criteria (9). Patients with lymphoplasmacytic infiltrate consisting of more than ten cells expressing the IgG4 by high-power field (HPF, 0.196 mm2) and a cell ratio of IgG4+ cells/IgG+ cells >40% were classified as cases of IgG4-ROD. Other patients were classified as cases of non-IgG4-ROD.
Review of MR imaging
The 38 patients’ MRIs were blinded for clinical and pathological data and read independently and in random order by two radiologists. One radiologist was a senior neuroradiologist specialising in orbital imaging with 7 years of experience (*BLINDED*) and the other radiologist was a general radiologist with 5 years of experience (*BLINDED*). Discrepancies were resolved by consensus.
Our primary MRI criterion was the presence of infraorbital nerve enlargement (IONE), defined as an infraorbital nerve that is larger than the optic nerve on a coronal section [20].
The following MRI characteristics were assessed:
-
The presence of mild infraorbital nerve enlargement (MIONE) defined as a larger coronal section of the ION in comparison with contralateral ION, but with the coronal section of the ION remaining smaller than or equal to that of the optic nerve;
-
The T1, T2, and diffusion-weighted imaging signal of the orbital lesion and ION defined as hypointense, isointense, or hyperintense compared with a healthy extraocular muscle signal as reference;
-
The ION enhancement (rated from 0 to 3 as follows: 0 if no enhancement is noted, 1 if enhancement is lower than healthy extraocular muscles, 2 if it has the same enhancement as the extraocular muscles, 3 if the enhancement is higher than the extraocular muscles);
-
The pattern of contrast enhancement: is it affecting the whole nerve or only its periphery?
-
The presence of infiltration of the orbital fat;
-
The presence of myositis;
-
The presence of a dacryoadenitis;
-
The presence of an involvement of the orbital apex;
-
The presence of an involvement of any other branches of the trigeminal nerve.
-
The orbital quadrant predominantly affected by the inflammation: external superior quadrant, internal superior quadrant, external inferior quadrant, internal inferior quadrant;
-
The presence of a contact between the orbital inflammatory changes and the ION;
-
The presence of a maxillary sinus disease.
Statistical analysis
Data were analysed using the R software package [23]. The two groups of patients (IgG4-ROD and non-IgG4-ROD) were compared in univariate analyses for patients’ characteristics, clinical items, and MRI criteria. Fisher’s exact test was used for nominal variables, the Kruskal-Wallis rank sum test was used for ordinal variables, and the Student’s test was used for continuous variables. P-values below 0.05 were considered significant. Subsequently, a multivariate model was developed using recursive partitioning to predict patients’ diagnoses (IgG4-ROD or non-IgG4-ROD) from a combination of MRI signs. Inter-observer agreement for MRI reading was assessed using non-weighted kappa statistics and interpreted according to Landis and Koch [24].
Results
Demographic and clinical characteristics
Thirty-eight patients were included in the study, of whom 15 had a definite diagnosis of IgG4-ROD and 23 had non-IgG4-ROD. Demographic and clinical data are presented in Table 2. In the non-IgG4-ROD group, 18 patients had idiopathic orbital inflammation, 2 had sarcoidosis, and 3 had Sjögren syndrome. The median age was 47 years. There was no difference between the two groups in either demographic characteristics or clinical signs. Out of 38 MRIs, 30 had been performed at our centre, with a 3-T Philips INGENIA or a 1.5-T Philips ACHIEVA imager with a 32-channel head coil (Philips Medical Systems, Best, The Netherlands). Eight other MRIs had been performed in other facilities with a 1.5-T imager.
Infraorbital nerve involvement
IONE was present in eight (53%) IgG4-ROD patients (as shown in Fig. 1) whereas it was not present in non-IgG4-ROD patients; the difference was highly significant (P < 0.0001). The sensitivity, specificity, positive predictive value, and negative predictive value of IONE for IgG4-ROD were 53%, 100%, 100%, and 77%, respectively.
Orbital MRI coronal T2 sections (a) and T1 Fat Sat (b) after injection of gadolinium in a patient with IgG4-ROD, showing an infraorbital nerve enlargement and enhancement (white star). It shows thickening, T2 hyperintensity and enhancement of the right lateral rectus and inferior rectus muscles (white arrowhead) as well as orbital fat inflammation (black arrowhead)
MIONE was present in three patients, all of them non-IgG4-ROD (P = 0.011) (as shown in Fig. 2).
Considering post-contrast sequences, IgG4-ROD patients were significantly more likely to present with ION enhancement (P < 0.05). IgG4-ROD patients were significantly more likely to present with an enhancement of the whole nerve: 6/7 (86%) versus only 1/3 (33%) patients in the non-IgG4-ROD group (P = 0.01). The remaining patients had only peripheral enhancement.
Localisation of inflammation and IONE
In the IgG4-ROD group, the localisation of the inflammation (superior versus inferior quadrants) was strongly associated with IONE (P < 0.001): 8/10 80% patients with an involvement of one lower orbital quadrant had an IONE (as shown in Fig. 1) whereas IONE was never present in cases with inflammation involving only an upper quadrant (as shown in Fig. 3). Moreover, IONE was strongly associated with the presence of a “contact” between orbital inflammation and the infraorbital canal (P < 0.00001): contact was present in all IONE cases and not present in non-IONE cases. There was no significant extraocular nerve or trigeminal nerve branch enlargement by the “contact” of inflammation.
Involvement with other trigeminal branches
The involvement of any other branch of the trigeminal nerve was significantly higher in IgG4-ROD patients (P < 0.005). The frequency of the isolated involvement of the frontal or mandibular branches of the trigeminal nerve was not different between IgG4-ROD and non-IgG4-ROD patients (as shown in Fig. 4).
MRI T2 orbital coronal sections of IgG4-ROD patients show perineural spread along the frontal branch of the ophthalmic nerve (V1) (white star) (a), along the maxillary branch of the trigeminal nerve into the foramen rotundum (V2) (white arrowhead) (b) and along the mandibular branch of the trigeminal nerve into the foramen ovale (V3) (white arrow) (c)
Signal and morphological characteristics
IgG4-ROD inflammatory lesions were significantly less likely to present with T2 hyperintensity (P < 0.01) and significantly more likely to present with T2 isointensity (P < 0.02). There was no difference of signal—in either T1 or diffusion-weighted imaging sequences—between IgG4-ROD and non-IgG4-ROD. There was also no difference between the two groups regarding morphological characteristics (as shown in Table 3).
Maxillary sinus disease
Nine (60%) IgG4-ROD patients presented with a maxillary sinus disease versus 7 (30%) non IgG4-ROD patients, but this was not significant (P = 0.37).
Multivariate analysis
The recursive partitioning procedure led to a simple two-branch decision tree: if IONE was present, then we could predict an IgG4-ROD aetiology; if IONE was not present, then we could not predict a non-IgG4-ROD aetiology. No other MRI criterion added predictive value in a multivariate model.
Inter-observer agreement
The two blinded readers assessing IONE and MIONE had excellent (k = 1) and good (k = 0.78) inter-observer agreement respectively.
Discussion
Comparison with literature
IONE appeared to be a specific sign to diagnose IgG4-ROD in European patients suffering from orbital inflammation. Most data published so far on IgG4-ROD pertain to Asian patients, especially Japanese patients. The literature analysis showed the preponderance of Asian series related to IgG4-ROD, especially Japanese series representing 41.9% of the articles and 86.6% of patients versus only 9.3% of studies and 4.1% of patients for the European series [11]. More generally, the Asian series-to-Western series ratio was around 2.4 to 1 [8]. The largest non-Asian series included 27 North-American patients [21]. Despite the ethnic differences, our results were consistent with the main study that investigated IONE [20], reporting 40.9% of IONE in 16 patients with IgG4-ROD, and slightly higher than those of other Japanese and American series with a prevalence ranging from 23.8% to 32% [6, 18, 19, 21, 25]. We had less bilateral and lacrimal gland involvement and a higher incidence of inferior locations of inflammation compared to the literature [8, 21]. We also had fewer maxillary sinus diseases than the 89% reported in the literature [21], and there was no significant difference between IgG4-ROD and non-IgG4-ROD in our series. The prevalence of the involvement of any other branch of the trigeminal nerve was 87% in our study, higher than the 24%-42.3% reported in the literature [6, 18, 19, 25]. However, the involvement of branches of the trigeminal nerve may be inconspicuous, such as the frontal nerve, or the maxillary nerve in the foramen rotundum. Previous studies were not specifically designed to search for a trigeminal nerve involvement [6, 18, 19, 21], which may have led to an underestimation. We did not find any IONE in the non-IgG4-ROD patients compared to 50% in an Anglo-Australian series [17]. In this series, all patients presented with an orbital benign lymphoid hyperplasia, a diagnostic entity histologically considered as IgG4-ROD [12, 14]. The comparison with previous studies is presented in Table 4.
Choice of diagnostic criteria
The comparison with literature data remains challenging because of the constantly evolving nature of this disease. The diagnostic criteria for IgG4-ROD are still currently being defined, and none of the four sets of diagnostic criteria proposed to date have been validated [7, 22, 26, 27]. We decided to use the Japanese consensus by Umehara [7], which considers patients fulfilling the criteria for the defined or probable IgG4-ROD to be positive. This agreement established a cut-off at ten cells expressing IgG4 by HPF for the diagnosis—this threshold being relatively low compared to other studies’ cut-off at up to 100 [26]. The choice of this criterion was motivated by the fact that it had been used in other similar series, thus allowing for the comparability of our results [12, 20, 28–30]. They fulfil the last criteria specifically proposed for IgG4-ROD, requiring the presence of an orbital mass and/or swelling associated with a lymphoplasmacytic infiltrate composed either by >50 IgG4 + cells/HPF or by a ratio IgG4/IgG >40% [22].
Contact between inflammation and ION
We have studied the strong correlation between IONE and the presence of a “contact” with the orbital inflammation, which has never been described in the literature to our knowledge. In our series, all patients with IgG4-ROD presenting with orbital inflammation in contact with the ION canal had IONE. On the contrary, there was no IONE in patients presenting with IgG4-related inflammation away from the ION canal, like in dacryoadenitis. The IgG4-RD is known for its neural tropism, and it seems that neural infiltration occurs by direct contiguity with the orbital inflammation [6]. The tropism of the IgG4-RD for peripheral nerves had already been highlighted in several papers, with a prevalence of around 6% [25, 31]. Periorbital nerve infiltration, especially infra- and supraorbital nerves, accounted for two-thirds of the neural involvements and were always associated with IgG4-ROD in Inoue’s series [25].
Differential diagnoses and pitfalls
IgG4-ROD is not the only orbital disease presenting with IONE. Differential diagnoses include aggressive tumours [32] and neurogenic tumours [33], with a distinct clinico-radiological presentation. Diagnosis may be challenging in cases of lymphoma, with a clinical presentation very close to orbital inflammations. However, they present with a strongly restricted apparent diffusion coefficient on an MRI [34]. Thus, we deliberately chose to exclude orbital lymphoma from our study in order to have a homogeneous population with orbital inflammation. In this study, none of the orbital inflammations presented with diffusion restriction visible via MRI. Finally, some specific orbital inflammatory diseases such as sarcoidosis may be responsible for perineural spread [35]; we did not observe any IONE in our series, but our series was underpowered in this regard, with only two cases of sarcoidosis-related orbital inflammation.
In this study, we observed MIONE in 3/23 non-IgG4-ROD patients. On the contrary, all IgG4-ROD patients presenting with IONE had an obvious enlargement of the ION with a coronal section of the ION larger than that of the optic nerve whereas no IgG4-ROD patient had a MIONE. These cases of MIONE are probably related to non-specific inflammatory changes rather than perineural spread as observed in the IgG4-ROD cases and should be interpreted with caution. Some authors measured the infraorbital canal and suggested a cut-off of 3.3 mm to define IONE [19], but we believe that IONE can easily be assessed visually [20]. Thus, even radiologists who are not specialised in orbital imaging can easily recognise IONE as a key sign and alert the clinician.
Limits of the study
Our study suffers several limitations. First, this is a retrospective, single-centre study, with a relatively small number of patients, thus limiting its statistical power. Second, a significant number of patients were excluded, with possible selection bias. Third, the examinations performed were not homogeneous. MRIs were not performed on the same machine or at the same field level. Nevertheless, we have retained the IONE as the primary endpoint, which is less dependent on image quality. Fourth, clinical and biological data such as serum IgG4 levels were missing for some patients. However, all patient records indicated that histological and immunohistochemical analyses were conducted according to international recommendations [7, 22].
Clinical relevance
IgG4-ROD patients often present with a subacute or insidious onset, with the symptoms of orbital mass effect developing gradually, often with minimal or no signs of inflammation. The reported mean duration of symptoms is often long, ranging from 4 to 61 months [14]. In the current practice, the early establishment of an appropriate treatment is essential to prevent irreversible damage such as a steady decrease in visual acuity or ocular dryness related to fibrosis [36]. The therapeutic protocols are different between idiopathic orbital inflammation and IgG4-ROD, making the distinction between these entities essential. Systemic corticosteroids remain the recommended treatment but carry a high recurrence rate [36]. Biotherapy with an anti-CD20 monoclonal antibody (rituximab) appeared to be effective [37].
Changes in the current practice
Identifying an IONE is essential for clinicians, especially because no other clinical or imaging findings help to differentiate IgG4-ROD from other orbital inflammatory diseases. Infraorbital nerve enlargement is a distinct, specific sign to predict IgG4-related aetiology in European patients suffering from orbital inflammation. A quicker diagnosis should allow for a more accurate management of patients with a quicker appropriate treatment and may contribute to an improved functional outcome of these patients. Further studies are needed to confirm the usefulness of this key sign in larger European populations.
Abbreviations
- IgG4-ROD:
-
IgG4-related ophthalmic disease
- non-IgG4-ROD:
-
non-IgG4-related ophthalmic disease
- MRI:
-
Magnetic resonance imaging
- ION:
-
Infra-orbital nerve
- IONE:
-
Infra-orbital nerve enlargement
- MIONE:
-
Mild infra-orbital nerve enlargement
References
Hamano H, Kawa S, Horiuchi A et al (2001) High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med 344:732–738
Umehara H, Okazaki K, Masaki Y et al (2012) A novel clinical entity, IgG4-related disease (IgG4RD): general concept and details. Mod Rheumatol Jpn Rheum Assoc 22:1–14
Yamamoto M, Ohara M, Suzuki C et al (2004) Elevated IgG4 concentrations in serum of patients with Mikulicz’s disease. Scand J Rheumatol 33:432–433
Kitagawa S, Zen Y, Harada K et al (2005) Abundant IgG4-positive plasma cell infiltration characterizes chronic sclerosing sialadenitis (Küttner’s tumor). Am J Surg Pathol 29:783–791
Stone JH, Zen Y, Deshpande V (2012) IgG4-related disease. N Engl J Med 366:539–551
Katsura M, Mori H, Kunimatsu A et al (2012) Radiological features of IgG4-related disease in the head, neck, and brain. Neuroradiology 54:873–882
Umehara H, Okazaki K, Masaki Y et al (2012) Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol Jpn Rheum Assoc 22:21–30
Wu A, Andrew NH, McNab AA, Selva D (2015) IgG4-related ophthalmic disease: pooling of published cases and literature review. Curr Allergy Asthma Rep 15:27
Wallace ZS, Deshpande V, Stone JH (2014) Ophthalmic manifestations of IgG4-related disease: single-center experience and literature review. Semin Arthritis Rheum 43:806–817
McNab AA, McKelvie P (2015) IgG4-related ophthalmic disease. Part I: background and pathology. Ophthal Plast Reconstr Surg 31:83–88
Mulholland GB, Jeffery CC, Satija P, Côté DWJ (2015) Immunoglobulin G4-related diseases in the head and neck: a systematic review. J Otolaryngol Head Neck Surg. doi:10.1186/s40463-015-0071-9
Deschamps R, Deschamps L, Depaz R et al (2013) High prevalence of IgG4-related lymphoplasmacytic infiltrative disorder in 25 patients with orbital inflammation: a retrospective case series. Br J Ophthalmol 97:999–1004
Lindfield D, Attfield K, McElvanney A (2012) Systemic immunoglobulin G4 (IgG4) disease and idiopathic orbital inflammation; removing “idiopathic” from the nomenclature? Eye 26:623–629
Andrew NH, Sladden N, Kearney DJ, Selva D (2015) An analysis of IgG4-related disease (IgG4-RD) among idiopathic orbital inflammations and benign lymphoid hyperplasias using two consensus-based diagnostic criteria for IgG4-RD. Br J Ophthalmol 99:376–381
Wallace ZS, Khosroshahi A, Jakobiec FA et al (2012) IgG4-related systemic disease as a cause of “idiopathic” orbital inflammation, including orbital myositis, and trigeminal nerve involvement. Surv Ophthalmol 57:26–33
Katsura M, Morita A, Horiuchi H et al (2011) IgG4-related inflammatory pseudotumor of the trigeminal nerve: another component of IgG4-related sclerosing disease? AJNR Am J Neuroradiol 32:E150–E152
Hardy TG, McNab AA, Rose GE (2014) Enlargement of the Infraorbital Nerve. Ophthalmology 121:1297–1303
Sogabe Y, Ohshima K, Azumi A et al (2014) Location and frequency of lesions in patients with IgG4-related ophthalmic diseases. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Für Klin Exp Ophthalmol 252:531–538
Takano K, Yajima R, Seki N et al (2014) A study of infraorbital nerve swelling associated with immunoglobulin G4 Mikulicz’s disease. Mod Rheumatol Jpn Rheum Assoc 24:798–801
Ohshima K-I, Sogabe Y, Sato Y (2012) The usefulness of infraorbital nerve enlargement on MRI imaging in clinical diagnosis of IgG4-related orbital disease. Jpn J Ophthalmol 56:380–382
Tiegs-Heiden CA, Eckel LJ, Hunt CH et al (2014) Immunoglobulin G4-related disease of the orbit: imaging features in 27 patients. AJNR Am J Neuroradiol 35:1393–1397
Goto H, Takahira M, Takahira M et al (2015) Diagnostic criteria for IgG4-related ophthalmic disease. Jpn J Ophthalmol 59:1–7
R Core Team (2014) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org/
Landis JR, Koch GG (1977) An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 33:363–374
Inoue D, Zen Y, Sato Y et al (2012) IgG4-Related perineural disease. Int J Rheumatol 2012:1–9
Deshpande V, Zen Y, Chan JK et al (2012) Consensus statement on the pathology of IgG4-related disease. Mod Pathol 25:1181–1192
Khosroshahi A, Wallace ZS, Crowe JL et al (2015) International Consensus Guidance Statement on the Management and Treatment of IgG4-Related Disease. Arthritis Rheumatol Hoboken NJ 67:1688–1699
Plaza JA, Garrity JA, Dogan A et al (2011) Orbital inflammation with IgG4-positive plasma cells: manifestation of IgG4 systemic disease. Arch Ophthalmol Chic Ill 129:421–428, 1960
Sato Y, Ohshima K, Ichimura K et al (2008) Ocular adnexal IgG4-related disease has uniform clinicopathology. Pathol Int 58:465–470
Matsuo T, Ichimura K, Sato Y et al (2010) Immunoglobulin G4 (IgG4)-positive or -negative ocular adnexal benign lymphoid lesions in relation to systemic involvement. J Clin Exp Hematop JCEH 50:129–142
Soussan M, Medjoul A, Badelon I et al (2014) IgG4-related diffuse perineural disease. Neurology 83:1877–1878
Chong VF, Fan YF (1997) Pterygopalatine fossa and maxillary nerve infiltration in nasopharyngeal carcinoma. Head Neck 19:121–125
Nager GT (1984) Neurinomas of the trigeminal nerve. Am J Otolaryngol 5:301–333
Hiwatashi A, Yoshiura T, Togao O et al (2014) Diffusivity of intraorbital lymphoma vs. IgG4-related DISEASE: 3D turbo field echo with diffusion-sensitised driven-equilibrium preparation technique. Eur Radiol 24:581–586
Shah R, Roberson GH, Curé JK (2009) Correlation of MR imaging findings and clinical manifestations in neurosarcoidosis. AJNR Am J Neuroradiol 30:953–961
Yu W-K, Kao S-C, Yang C-F et al (2015) Ocular adnexal IgG4-related disease: clinical features, outcome, and factors associated with response to systemic steroids. Jpn J Ophthalmol 59:8–13
Carruthers MN, Topazian MD, Khosroshahi A et al (2015) Rituximab for IgG4-related disease: a prospective, open-label trial. Ann Rheum Dis 74:1171–1177
Acknowledgments
The scientific guarantor of this publication is Augustin Lecler, MD. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. One of the authors has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Methodology: retrospective, diagnostic or prognostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Soussan, J.B., Deschamps, R., Sadik, J.C. et al. Infraorbital nerve involvement on magnetic resonance imaging in European patients with IgG4-related ophthalmic disease: a specific sign. Eur Radiol 27, 1335–1343 (2017). https://doi.org/10.1007/s00330-016-4481-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4481-5