Abstract
Objectives
Failed lumbar puncture (LP) is a common indication for referral for radiologically guided LP. This study aims to evaluate what percentage of the hospital population would fail an LP using a standard 9-cm needle because of obesity and a skin to subarachnoid space distance greater than 9 cm.
Methods
Images of 402 consecutive patients undergoing computed tomography of the abdomen and pelvis were reviewed. Skin to subarachnoid space distance was calculated using sagittal images. A survey was conducted among junior hospital doctors to assess their experience of performing lumbar puncture in obese patients.
Results
Four hundred patients were included. Fifty-five patients (13.8 %) had a skin to subarachnoid space distance greater than 9 cm. Intra-abdominal fat, subcutaneous fat and abdominal girth correlated with distance between the skin and subarachnoid space. Among junior doctors, 68.3 % (n = 41) reported LP failure on an obese patient; 78.4 % (n = 47) were unaware of the existence of a longer needle and 13.3 % (n = 8) had experience using a longer needle.
Conclusions
A significant proportion of the hospital population will fail LP with a standard length spinal needle. Selecting a longer needle may be sufficient to successfully complete LP in obese patients.
Key Points
• Lumbar puncture failure commonly leads to referral for an image-guided procedure
• Standard lumbar puncture may fail in 13.8 % of patients due to obesity
• 78.4 % of trainee doctors are unaware of the existence of longer spinal-needles
• Using longer spinal needles may allow successful LP in obese patients
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lumbar puncture (LP) is commonly performed by a variety of medical specialists, and in most cases is completed successfully. There is a subset of patients, however, including the obese and those with underlying anatomical spinal abnormalities, in whom LPs can be challenging. In these patients the procedure can lead to significant discomfort, is time consuming and is often ultimately unsuccessful. The standard needle used for LP is 9 cm in length. If the distance from the skin to the subarachnoid space is greater than 9 cm, the LP cannot usually be completed with a standard needle. There is a commercially available longer needle, which measures 15 cm and can be used instead of the 9-mm needle. From anecdotal experience of patients referred to the Radiology Department in our institution for image-guided LP, we postulated that a significant proportion of failed LPs in the general hospital population were caused by the use of too short a needle in obese patients. We aimed, using computed tomography (CT), to measure the skin to subarachnoid space distance in the lumbar region in a cohort of patients attending a university teaching hospital and to establish what percentage of these patients would fail a lumbar puncture if a “standard length” LP needle was used. We also performed a survey to analyse clinicians’ attitudes towards LPs in the obese population and to establish whether there is a good knowledge of LP needle lengths among those performing this procedure.
Materials and methods
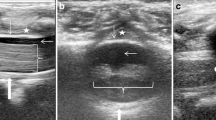
The images of the first 402 consecutive patients undergoing a CT of the abdomen and pelvis for any indication in our institution, commencing January 1st 2011, were selected for analysis. Images were performed using 264 slice multidetector CT (Toshiba Medical Systems, Otawara, Japan). Images were analysed using a Picture Archiving and Communications System (PACS) (Siemens, Erlangen, Germany). The distance from the skin to the subarachnoid space was calculated using a sagittally reconstructed image from each patient. A line was drawn from the skin to the subarachnoid space (Fig. 1). This line was drawn in an attempt to mimic the passage of a needle through the gap between the lumbar spinous processes. Subcutaneous fat was calculated at the level of the umbilicus. Intra-peritoneal fat was calculated at the level of the superior mesenteric artery by measuring the distance from the anterior abdominal wall peritoneum to the aorta. Due to the retrospective nature of the study, abdominal girth was estimated from the CT images. Girth was measured at the superior extent of the iliac crest to standardise between patients. The abdominal shape at this point was estimated as an ellipse. The major and minor axes of the ellipse were measured and the circumference of the ellipse calculated using the formula: \( \mathrm{Circumference}=2\uppi \sqrt{\raisebox{1ex}{$1$}\!\left/ \!\raisebox{-1ex}{$2$}\right.\left({\mathrm{a}}^2+{\mathrm{b}}^2\right)} \), where a represented the major axis and b the minor axis. One patient with a large volume of ascites, and one patient with a large volume of free intra-abdominal air were excluded from the study as accurate measurement of the intra-abdominal fat was not possible. Four hundred patients were included for data analysis.
Unless otherwise stated, data are represented as median (interquartile range [IQR]) and n represents the number of patients included in the analysis. Differences in distribution of clinical data were evaluated using a two-sided Fisher’s exact test for categorical variables and ANOVA for continuous variables. Multiple logistic regression analysis was performed to examine predictors of having a skin to subarachnoid space distance over 9 cm. Following univariate analysis, the variables which were statistically significant were used in a multivariate analysis. Correlations were calculated using the Spearman rank correlation test, and P < 0.05 was considered statistically significant. All calculations were done using SPSS version 12.0 (SPSS, Chicago, USA).
A written survey was administered to non-consultant hospital doctors NCHDs in our institution to assess their knowledge and practical experience of both performing lumbar puncture on obese patients and issues regarding needle length.
Results
In total there were 233 male (58.3 %) and 167 female (41.7 %) patients. The mean age was 56.8 ± 17 years. Of the total, 55 patients (13.8 %) had a skin to subarachnoid space distance greater than 9 cm (Table 1), suggesting likely failure with a standard length 90-mm spinal needle.
Women were significantly more likely than men to have a skin to subarachnoid space greater than 9 cm (19.1 % vs 9.9 %, P = 0.01, Fisher’s exact test). Those greater than 50 years of age were non-significantly less likely to have a skin to subarachnoid space greater than 9 cm (12.6 % vs 16.5 %, P = 0.337, Fisher’s exact test). Skin to subarachnoid space distance was highest at the L4/L5 interspace, 7.18 cm (range, 13.13-3.73) and lowest at the L2/L3 interspace, 6.32 cm (range, 12.69-3.61).
The distance between the peritoneum and aorta (intra-abdominal fat) correlated with the distance between the skin and subarachnoid space (r 2 = 0.357, P < 0.001, Spearman rank) (Fig. 2). Those with a skin to subarachnoid space distance greater than 9 cm had a greater peritoneum to aorta distance (9.4 [7.2-11.7] vs 12.0 [9.5-14.1], P < 0.001, ANOVA). The amount of subcutaneous fat correlated with the distance between the skin and subarachnoid space (r 2 = 0.497, P < 0.001, Spearman rank) (Fig. 3). Those with a skin to subarachnoid space distance greater than 9 cm had a greater amount of subcutaneous fat (1.9 [1.3-2.8] vs 3.3 [2.7-3.9], P < 0.001, ANOVA). Abdominal girth correlated with the distance between the skin and subarachnoid space (r 2 = 0.745, P < 0.001, Spearman rank) (Fig. 4). Those with a skin to subarachnoid space distance greater than 9 cm had a significantly greater abdominal girth (91.2 [82.3-98.3] vs 112.6 [105.9-119.8], P < 0.001, ANOVA).
In a multivariate analysis, having an abdominal girth over 100 cm increased the risk of having a skin to subarachnoid space distance over 9 cm (hazard ratio [HR], 32.7; 95 % confidence interval [CI], 13.66-78.21; P < 0.001) but being aged over 50 years (HR, 0.35; 95 % CI, 0.16-0.77; P = 0.009) and being male (HR, 0.33; 95 % CI, 0.16-0.66; P = 0.002) reduced the risk of having a skin to subarachnoid space distance over 9 cm (Table 2).
Sixty non-consultant hospital doctors (NCHDs) were asked to complete a survey, which was administered verbally and the results recorded by the investigators. Of these, 68.3 % reported LP failure on an obese patient; 71.6 % (n = 43) had referred an obese patient for image-guided LP after a clinically failed LP; 100 % (n = 60) routinely used 9-cm-long needles; 78.4 % (n = 47) were unaware of the existence of a longer needle; 13.3 % (n = 8) had experience using a longer needle.
Discussion
Obesity is one of the greatest threats to public health in the twenty-first century. In the USA, 33.8 % of the population are clinically obese [1], while the prevalence in the Irish population, in whom this study was conducted, is 24 % [2]. In addition to being a major risk factor for cardiovascular diseases and type two diabetes mellitus, obesity produces unique challenges in the practicalities of how medicine is physically performed. Surgeons, for example, have had to adapt techniques and equipment to allow surgery on obese patients, while radiology departments have become increasingly aware of the difficulties of imaging the overweight patient, both in terms of the size of radiological equipment needed and in increased radiation doses [3, 4].
Lumbar puncture is an important, commonly performed, diagnostic and therapeutic technique. The majority of LPs are successfully performed by clinicians, but obesity is a common contributing factor in failed procedures [5–8]. As the number of obese patients, which is currently predicted to grow by 1 % per annum, [3] continues to rise, the number of unsuccessful LPs in overweight patients is also likely to increase. Unsuccessful LPs, as might be expected, often take longer to perform and can result in significant patient discomfort. Anecdotally, it was noted in our institution that a large proportion of the patients referred to the radiology department for fluoroscopically guided LP were obese. When aided by image guidance, we also noted that in many of these patients a “standard” LP needle measuring 9 cm in length did not reach the subarachnoid space (Fig. 3). In many of these cases the use of a 15-cm spinal needle easily facilitated access to the subarachnoid space. Our results demonstrate that in a consecutive, unselected series of 400 patients, a 9-cm needle will be insufficient to reach the subarachnoid space in 13.8 % of cases. Our survey of clinicians’ knowledge of LP needle length revealed that there is also a marked lack of awareness among junior doctors as to the various lengths of LP needles available. In combination, these factors suggest that many patients undergo attempted LPs which are predestined to fail simply due to an incorrect choice of needle length.
The question therefore raised is: at what stage should clinicians consider using a longer LP needle? Unfortunately there is no definite answer to this, but there are several factors that clinicians can use to guide appropriate needle length selection. Our study uses the parameter of abdominal girth at the pelvic inlet to compare body size between patients, an easily clinically determinable measurement. Clearly there is no one girth above which we can say that the use of a longer needle is definitely necessary but our results do demonstrate certain trends. The current study demonstrated that having an abdominal girth over 100 cm increases the risk of having a skin to subarachnoid space distance over 9 cm by 32.7-fold, suggesting abdominal girth may be used as a clinical guide in choosing needle length. Body fat distribution is also likely to play an important role in the depth of LP needle required. In our study, women were significantly more likely to have a skin to subarachnoid distance greater than 9 cm. This likely relates to the typical female fat distribution, which causes fat to be preferentially distributed subcutaneously in the gluteal region, rather than the android intra-abdominal pattern of fat distribution [9]. In addition, when grouped by lumbar inter-space we found that the skin to subarachnoid depth increased in the lower lumbar region, peaking at the L4/5 interspace (Table 3). Using higher lumbar interspaces to perform LPs in overweight patients might therefore be beneficial. The skin to subarachnoid distance is lowest at the L2/3 interspace.
In the obstetric population there have been several attempts made to delineate the anatomical factors that affect the skin to the epidural space distance. Basic parameters such as age and height do not correlate with epidural depth [10]. However, waist circumference, waist circumference/height ratio, body mass index and weight have all been shown to correlate with epidural depth. The former three parameters have a significantly higher predictive value than weight alone [11].
Anaesthetists performing epidural anaesthesia have also attempted to develop models to successfully predict how deep the epidural space is using both image-guided and mathematical techniques. Image-derived estimates appear to be reliable predictors of epidural depth. Axial CT images used to trigonometrically calculate epidural depth correlate with actual epidural depths when measured clinically, albeit that CT overestimates the depth slightly (by a mean of 0.26 cm in one study) [12, 13]. The overestimation by CT is likely a result of different patient positioning during the two procedures. The curved position that a patient adopts during an LP for epidural block tends to tauten the skin, likely reducing the skin to epidural distance. Ultrasound has also found utility in the estimation of epidural depth in obese obstetric patients. Balki et al. [14] used ultrasound to determine that the mean estimated depth at L3/4 in their population was 6.3 cm, while the mean actual depth was 6.6 cm; both of these measurements having statistically significant correlation.
Several investigators have proposed mathematical methods to predict epidural depth. Ravi et al. have calculate the epidural space depth in a given patient as: a + b[BMI], where a is the constant =17.7966 and b is a regression coefficient = 0.9777 [10], while Craig et al. [15] used the formula 0.03 × height (cm) to estimate the mean depth of needle insertion for LP in children. Segal et al. [16] used a model containing variables including weight, height, body mass index, age, parity and interspace to predict epidural depth to within 8 mm; whereas Stamatakis et al. [17] used the same parameters to derive similar a mathematical predictors of epidural depth. Such predicting mechanisms, while useful, are clearly not a substitute for clinical judgement and experience, but, along with awareness of this issue, might aid in correct selection of LP needle length.
There are some limitations to our study. The supine position in which CT is performed is different to the decubitus or sitting position in which an LP is performed. It is inevitable that the fat distribution in the lumbar region is different in these positions. Indeed, as discussed above, the CT measurement in the supine position is likely to overestimate the clinical depth slightly. Even when adjusted for the 0.26-cm difference between CT predicted measurement and actual depth (as determined by Carnie et al. [12]), 12.5 % of our population have a skin to subarachnoid distance greater than 9 cm. The survey with regards to knowledge about longer needle lengths was only performed amongst junior doctors, excluding the more experienced practitioners in our institution. This is likely to have affected the results. However, we felt that junior doctor were much more likely to be performing this procedure in an acute setting and that therefore the results hold validity. One important factor influencing LP failure which was not assessed is the presence of spinal degenerative disease. Alterations in local anatomy caused by spinal osteoarthritis can lead to difficulty in completing LPs. In addition, obesity is a well established risk factor for spinal osteoarthritis, particularly facet joint degenerative change [18].
Obesity is a rapidly growing public health problem. It has a multifaceted effect on the provision of healthcare. The choice of alternate equipment to treat obese patients is one example of how health services have had to adapt to the challenge posed by the obesity epidemic. Our results demonstrate that there is a significant proportion of the general hospital population in whom LP is not possible with a standard length needle. The results also indicate that there is a lack of awareness among junior clinicians of this issue. LP failure in obese patients may be multi-factorial. Difficulty with patient positioning and loss of normal anatomical landmarks are also complicating factors [5, 6]. However, we feel that the simple step of selecting a longer spinal needle would be sufficient in many cases to successfully complete this important diagnostic and therapeutic procedure without causing undue discomfort or stress to the patient. The potential impact of physician education and wider use of longer LP needles on the rate of LP failure could be the subject of future, prospective studies.
Abbreviations
- LP:
-
Lumbar puncture
- HR:
-
Hazard ratio
- NCHD:
-
Non-consultant hospital doctors
References
http://www.cdc.gov/obesity/data/trends.html. Accessed 05/02/2012
http://www.iuna.net/wp-content/uploads/2010/12/National-Adult-Nutrition-Survey-Summary-Report-March-2011.pdf, accessed 05/02/2012
Campbell N, Buckley O, McGlone B, O’Shea D, Torreggiani WC (2009) Obesity in Ireland in 2008: what radiological equipment is available to image the obese patient? Ir Med J 102:116–117
Buckley O, Ward E, Ryan A, Colin W, Snow A, Torreggiani WC (2009) European obesity and the radiology department. What can we do to help? Eur Radiol 19:298–309
Palmer SK, Abram SE, Maitra AM, von Colditz JH (1983) Distance from the skin to the lumbar epidural space in an obstetric population. Anesth Analg 62:944–946
Clinkscales CP, Greenfield MLVH, Vanarase M, Polley LS (2007) An observational study of the relationship between lumbar epidural space depth and body mass index in Michigan parturients. Int J Obstet Anesth 16:323–327
Gerig HJ, Kern F (1985) Success and failure rate in peridural anesthesia. A 1-year study. Reg Anesth 8:25–32
Le Coq G, Ducot B, Benhamou D (1998) Risk factors for inadequate pain relief during epidural analgesia for labor and delivery. Can J Anaesth 45:719–723
Dixon AK (1983) Abdominal fat assessed by computed tomography: sex difference in distribution. Clin Radiol 34:189–191
Ravi KK, Kaul TK, Kathuria S, Gupta S, Khurana S (2011) Distance from skin to epidural space: correlation with body mass index (BMI). J Anaesthesiol Clin Pharmacol 27:39–42
Bahk JH, Kim JH, Lee JS, Lee SC (1998) Computed tomographic study of lumbar (L3-4) epidural depth and its relationship to physical measurements in young adult men. Reg Anesth Pain Med 23:262–265
Carnie J, Boden J, Gao Smith F (2002) Prediction by computerised tomography of distance from skin to epidural space during thoracic epidural insertion. Anaesthesia 57:701–704
Kao MC, Tsai SK, Chang WK, Liu HT, Hsieh YC, Hu JS, Mok MS (2004) Prediction of the distance from skin to epidural space for low-thoracic epidural catheter insertion by computed tomography. Br J Anaesth 92:271–273
Balki M, Lee Y, Halpern S, Carvalho JC (2009) Ultrasound imaging of the lumbar spine in the transverse plane: the correlation between estimated and actual depth to the epidural space in obese parturients. Anesth Analg 108:1876–1881
Craig F, Stroobant J, Winrow A, Davies H (1997) Depth of insertion of a lumbar puncture needle. Arch Dis Child 77:450
Segal S, Beach M, Eappen S (1996) A multivariate model to predict the distance from the skin to the epidural space in an obstetric population. Reg Anesth 21:451–455
Stamatakis E, Moka E, Siafaka I, Argyra E, Vadalouca A (2005) Prediction of the distance from the skin to the lumbar epidural space in the Greek population, using mathematical models. Pain Pract 5:125–134
Kalichman L, Guermazi A, Li L, Hunter DJ (2009) Association between age, sex, BMI and CT-evaluated spinal degeneration features. J Back Musculoskelet Rehabil 22:189–195
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Halpenny, D., O’Sullivan, K., Burke, J.P. et al. Does obesity preclude lumbar puncture with a standard spinal needle? The use of computed tomography to measure the skin to lumbar subarachnoid space distance in the general hospital population. Eur Radiol 23, 3191–3196 (2013). https://doi.org/10.1007/s00330-013-2909-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-013-2909-8