Abstract
Background
Disadvantages of fluoroscopically guided lumbar puncture include delivery of ionizing radiation and limited resolution of incompletely ossified posterior elements. Ultrasound (US) allows visualization of critical soft tissues and the cerebrospinal fluid (CSF) space without ionizing radiation.
Objective
To determine the technical success and safety of US-guided lumbar puncture in pediatric patients.
Materials and methods
A retrospective review identified all patients referred to interventional radiology for lumbar puncture between June 2010 and June 2017. Patients who underwent lumbar puncture with fluoroscopic guidance alone were excluded. For the remaining procedures, technical success and procedural complications were assessed. Two hundred and one image-guided lumbar punctures in 161 patients were included. Eighty patients (43%) had previously failed landmark-based attempts.
Results
One hundred ninety-six (97.5%) patients underwent lumbar puncture. Five procedures (2.5%) were not attempted after US assessment, either due to a paucity of CSF or unsafe window for needle placement. Technical success was achieved in 187 (95.4%) of lumbar punctures attempted with US guidance. One hundred seventy-seven (90.3%) were technically successful with US alone (age range: 2 days-15 years, weight range: 1.9-53.1 kg) and an additional 10 (5.1%) were successful with US-guided thecal access and subsequent fluoroscopic confirmation. Three (1.5%) cases were unsuccessful with US guidance but were subsequently successful with fluoroscopic guidance. Of the 80 previously failed landmark-based lumbar punctures, 77 (96.3%) were successful with US guidance alone. There were no reported complications.
Conclusion
US guidance is safe and effective for lumbar punctures and has specific advantages over fluoroscopy in pediatric patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lumbar puncture is an established technique for cerebrospinal fluid (CSF) collection, intrathecal pressure measurement, and delivery of intrathecal therapy. CSF analysis and opening pressure measurements play an integral role in diagnosing a variety of diseases [1, 2]. Lumbar puncture also serves as a means to administer medications intrathecally, particularly in chemotherapy [3]. Landmark-based lumbar puncture without image guidance is the standard of care. When landmark-based lumbar puncture attempts fail, patients are referred for image-guided lumbar puncture, which traditionally has been performed under fluoroscopic guidance [4].
Although fluoroscopic guidance has been shown to decrease the rate of traumatic lumbar punctures compared to landmark-based ones, there are several disadvantages to fluoroscopy in the pediatric population [5]. Fluoroscopy allows for visualization of bony spinal landmarks, but it does not allow direct visualization of the thecal sac, conus medullaris or nerve roots. Given variability in anatomy and location of the conus medullaris in pediatric patients and the potentially collapsed thecal sac following failed lumbar puncture attempts, direct visualization of spinal anatomy is optimal. Furthermore, while incompletely ossified posterior elements limit the utility of fluoroscopy in infants, this expands the acoustic window with ultrasound (US). Finally, fluoroscopy delivers ionizing radiation. Although deterministic effects of radiation exposure from imaging have not been established, prior investigations have shown that pediatric patients are exposed to greater risk from ionizing radiation [6].
US has been used as an alternate means of image guidance in many interventional procedures. However, there is limited data reporting the utility of US for image-guided lumbar puncture [7, 8]. Increasing experience with US guidance has increased our utilization of US for lumbar puncture guidance. This retrospective review assesses the safety and efficacy of real-time US-guided lumbar punctures in pediatric patients.
Materials and methods
A retrospective study was conducted at a single institution by identifying all patients who underwent lumbar punctures with intraprocedural US imaging between June 2010 and June 2017. The study was approved by the hospital’s Institutional Review Board with waiver of informed consent. All patients were referred to interventional radiology for image-guided lumbar punctures, either due to a history of prior failures or anticipated difficulty with landmark-based lumbar punctures. All patients were between the ages of 0 and 18 years. Patients who underwent lumbar puncture with fluoroscopic guidance alone were not included in the study.
All procedures were performed by one of seven board-certified interventional radiologists or an interventional radiology physician assistant, ranging in experience from 1 to 25 years. The choice of image guidance between US and fluoroscopy was at the discretion of the interventional radiologist. Initially, US was primarily used for patients younger than 6 months. As institutional experience grew, US guidance was expanded to older, larger patients. There was no specific age or weight limit, and some providers attempted US-guided lumbar puncture in patients up to 65 kg. If the thecal sac or needle trajectory could not be well-visualized sonographically, then the procedure was attempted with fluoroscopic guidance.
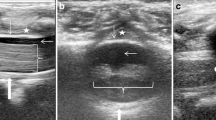
Patients were brought to the interventional radiology suite and were placed in the lateral decubitus position. US visualization of the thecal sac below the level of the conus was performed using a Philips iU22 US machine with C8-5, L9-3 or L15-7 transducers (Philips Healthcare, Eindhoven, The Netherlands), depending on patient body habitus and operator preference. Transverse (Fig. 1) or sagittal (Fig. 2) views with variable obliquities were chosen to optimize an unobstructed needle trajectory including thecal sac visualization. In patients in whom the thecal sac was visualized with appreciable CSF, lumbar puncture was carried out under US guidance. After standard sterile preparation and delivery of local anesthesia, a 22-gauge Quincke spinal needle (Becton Dickinson, Franklin Lakes, NJ, USA) was advanced under real-time, in-plane needle visualization. In patients younger than 6 months of age with nonossified or partially ossified posterior elements, the thecal sac was visualized in its entirety and the needle was visualized from skin entry into the thecal sac. In patients older than 6 months, complete or nearly complete primary ossification of the posterior elements obscured the thecal sac (Fig. 3). Probe position and beam angulation adjustments allowed thecal sac visualization through the interlaminar space in either transverse (Fig. 3) or oblique sagittal orientations (Fig. 4).
US-guided lumbar puncture in a 24-day-old, 2 kg boy. a Transverse US image at the level of L1 demonstrates the conus medullaris (bracket) with small anechoic cerebrospinal fluid (CSF) space (asterisk). A translaminar view was achieved due to minimal ossification of the posterior elements (arrowheads). b Transverse US image at L3-L4 demonstrates a large CSF space (asterisk) below the conus medullaris with anteriorly layering nerve roots of the cauda equina (arrowheads). c Transverse US image demonstrates a posterolateral spinal needle approach and the needle tip (arrow) within the thecal sac
US-guided lumbar puncture in a 23-day-old, 4 kg boy with concern for meningitis. a Sagittal US image at the level of L4-5 demonstrates an adequate quantity of cerebrospinal fluid within the thecal sac (asterisk) with anteriorly layering nerve roots of the cauda equine (arrowheads). b Sagittal US image demonstrates an inferior approach spinal needle and the tip (arrow) within the thecal sac
US-guided lumbar puncture in a 5-year-old, 18 kg girl with acute vomiting and ataxia. a Transverse US image at the level of L4 demonstrates obstructed visualization of the thecal sac by ossified spinous process (open arrow) and bilateral laminae (white arrows). b The US probe is moved inferiorly to the level of L4-5, achieving unobstructed visualization of the thecal sac through the interlaminar space
US-guided lumbar puncture in a 10-year-old, 24 kg boy with acute paralysis and suspected demyelinating disease. a Paramedian oblique sagittal US image at the level of L4-5 demonstrates largely unobstructed visualization of the thecal sac (asterisk). b Paramedian oblique sagittal US image at the level of L4-5 demonstrates an inferior approach spinal needle and tip (arrow) within the thecal sac
In patients younger than 2 months, lumbar puncture was performed with local anesthesia only, unless there had been problems with prior attempts using only local anesthesia. Patients older than 15 years were considered for local anesthesia only, at the discretion of the parents and referring provider. All other patients underwent the procedure with anesthesia assistance, either monitored anesthesia care or general anesthesia, at the anesthesiologist’s discretion.
Baseline demographics, procedural data, outcomes and complications were assessed retrospectively. Baseline demographics included age and weight on the date of the procedure. Procedural data included prior landmark-based attempts and type of anesthesia. Primary outcome measure was technical success, as defined by the return of CSF from the spinal needle and successful delivery of intrathecal medication when applicable. Secondary outcome measures included traumatic lumbar punctures, defined as more than 500 red blood cells (RBCs)/mm3 in the first vial of CSF [9]. Patient records were reviewed for complications including bleeding and CSF leak reported up to 1 week after the procedure.
Results
During the study period, 161 patients were referred to interventional radiology for a total of 201 lumbar punctures for which US guidance was considered. Results are summarized in Table 1 and Fig. 5. The median age was 125 days (range: 2 days-17.7 years). Of the 201 lumbar punctures referred to interventional radiology, 107 (53%) were in patients younger than 6 months, while 94 (47%) were in patients older than 6 months. Results for patients 6 months of age and younger are summarized in Tables 2 and 3, respectively. One hundred and seven cases (54.5%) were performed with anesthesia assistance, either under monitored anesthesia care or general anesthesia at the anesthesiologist’s discretion. There were no reported complications up to 1 week after the procedure.
One hundred and four cases were referred for diagnostic lumbar puncture; 9 were for therapeutic lumbar puncture, 16 were for both diagnostic and therapeutic lumbar puncture and 2 were for myelography. Of the therapeutic lumbar punctures, five were referred for intrathecal Spinraza administration for spinal muscular atrophy and four were referred for idiopathic intracranial hypertension. All patients with both diagnostic and therapeutic lumbar punctures were referred for malignancy and intrathecal chemotherapy. The two myelograms were referred for evaluation of brachial plexus injuries.
Five lumbar punctures (3%) were not attempted after initial US evaluation. The most common reason for not attempting the procedure was a paucity of CSF seen on the initial US (n=4) (Fig. 6). In two of these cases, the patients were admitted overnight for intravenous hydration and subsequently had successful US-guided lumbar punctures. In two other patients, lumbar puncture was initially requested as part of the sepsis work-up, but both patients clinically improved after discontinuing antibiotics, so repeat lumbar puncture was not requested. In the fifth patient, lumbar puncture was not attempted due to a concerning rash overlying the spine.
US images in a 14-day-old, 4 kg girl with neonatal fever and five failed bedside attempts. Transverse (a) and sagittal (b) US images at the level of L3-4 demonstrate a paucity of cerebrospinal fluid in the thecal sac with crowding of the nerve roots below the conus (arrowhead) and an overlying epidural fluid collection (arrow), presumed to represent an epidural hematoma. Lumbar puncture was not attempted, and the patient was transferred back to the clinical service for hydration. The patient clinically improved off antibiotics, so a repeat attempt at lumbar puncture was not performed
One hundred and seventy-seven lumbar punctures (90.3%) were technically successful with US alone. Three cases (1.5%) were unsuccessful with US guidance due to limited visualization of the thecal sac (n=2) or limited visualization of the needle (n=1), but they were subsequently successful with fluoroscopic guidance. In three cases (1.5%), attempts under both US and fluoroscopic guidance were unsuccessful, which was attributed to a paucity of CSF in all cases.
In patients younger than 6 months of age, 97 (95%) lumbar punctures were technically successful with US alone (median age: 27 days [range: 2-176 days] and median weight: 3.9 kg [range: 2.9-10 kg]). In two failed attempts with US guidance, fluoroscopic guidance was attempted as the needle was not well visualized sonographically. In both of these cases, fluoroscopic lumbar puncture was also unsuccessful. In the other three cases of failed image-guided lumbar puncture, the thecal sac and needle were well-visualized sonographically, so fluoroscopic guidance was not attempted. Lumbar puncture failure was attributed to a paucity of CSF in these cases.
In patients older than 6 months, 80 (85%) were technically successful with US alone (median age: 4.3 years [range: 0.5-15 years] and median weight: 14.6 kg [range: 6.3-53.1 kg]). In 10 cases (5.1%), US was used for guidance and subsequent fluoroscopy was used to confirm needle placement. Fluoroscopy was also used for confirmation in some initial patients, as operator expertise with US guidance was still being acquired. In 4 cases with failed US guidance, lumbar puncture was always subsequently attempted with fluoroscopic guidance and completed successfully in 3 cases (75%). One case was unsuccessful with both US and fluoroscopic guidance, which was attributed to a paucity of CSF.
Eighty-three cases (41%) were referred for prior failed bedside lumbar puncture. Three of these cases were evaluated with US, but were not attempted due to a paucity of CSF. Seventy-seven (96.3%) of the subsequently attempted lumbar punctures were technically successful with US guidance alone. Of the 177 technically successful cases with US guidance alone, 42 (24%) were notable for traumatic lumbar punctures based on >500 RBCs/mm3 in the first vial of CSF. Thirty-nine (93%) of those with >500 RBCs/mm3, however, had previously undergone prior failed landmark-guided lumbar puncture attempts. All traumatic lumbar punctures had adequate CSF for culture.
Discussion
Methods for US-assisted and US-guided lumbar puncture have been previously described in both the pediatric emergency medicine and interventional radiology literature [10, 11]. However, there is limited data on the use of real-time US guidance for lumbar puncture, with notable absence of a large clinical series. Coley et al. [7] performed US-guided lumbar puncture in 19 neonates and infants, demonstrating a technical success rate of 58%. Wang et al. [8] performed US-guided lumbar puncture in 9 pediatric patients, demonstrating a technical success rate of 100%. Our study is the largest to date, demonstrating a technical success rate of 90% with US guidance alone, and a technical success rate of 85% in patients older than 6 months with US guidance alone. An additional 10 cases (5.1%) were successfully guided by US but subsequently confirmed by fluoroscopy, occurring early in the series, likely reflecting operator learning curve. Furthermore, our study demonstrates a technical success rate of 93% in cases with previously failed bedside landmark-based attempts.
Our study also demonstrates the value in US evaluation of the thecal sac before lumbar puncture. This pre-procedure assessment allows for evaluation of spinal anatomy and quantification of CSF prior to puncture. In our series, this assessment also prevented five patients from unnecessary attempts due to a paucity of CSF. In two of these cases, this led to the patients being admitted for intravenous hydration, which aided in subsequent successful lumbar punctures. Experience gained over the course of the study period has resulted in further local practice change with increased use of pre-sedation US for patients with prior failed attempts, either by the proceduralist or with formal spinal US when conditions allow.
US imaging of the neonatal spine provides a largely unobstructed evaluation of the spinal canal contents, which is useful for both diagnosis and procedural guidance. While increased depth and partial structural obscuration by posterior element ossification in older and larger patients, visualization for procedural guidance often remains sufficient (Figs. 3 and 4). Where previous studies have predominately focused on neonatal populations, we report high technical success in a wide patient age range of 2 days to 15 years and predict future studies will confirm body habitus to be a more important predictor of feasibility than age.
This study has limitations. Selection bias related to retrospective study design may artificially inflate the technical success rate. Additionally, there is potential selection bias in the analysis, not capturing older patients who went directly to fluoroscopically guided lumbar puncture. Because of the young age and low average body weight of patients in this study, with excellent sonographic visualization of the thecal sac, the technical success reported in this series may not be reproducible in older, larger patients. Furthermore, fluoroscopic guidance has been nearly completely replaced by US guidance in younger children at our institution, which prevents direct comparison between the two modalities. The retrospective assessment of patient charts potentially led to the incomplete capture of complications. We assume major complications requiring additional treatment would not go undocumented but acknowledge that minor complications associated with lumbar punctures, such as self-limited positional headache, may be underreported. Limited communicative capacity of many of our younger patients may also have resulted in lower apparent complications.
Conclusion
This study demonstrates that real-time US-guided lumbar puncture is a safe and effective method for performing pediatric lumbar punctures. US guidance has many advantages over traditional fluoroscopic guidance, including the ability to evaluate the thecal sac prior to puncture, to directly visualize the thecal sac and conus medullaris in real time, and to verify needle placement, all without exposure to ionizing radiation. Given its safety and high technical success rate, US guidance should be considered for image-guided lumbar puncture in pediatric patients.
References
Avery RA (2014) Reference range of cerebrospinal fluid opening pressure in children: historical overview and current data. Neuropediatrics 45:206–211
Bonadio W (2014) Pediatric lumbar puncture and cerebrospinal fluid analysis. J Emerg Med 46:141–150
Pui CH, Howard SC (2008) Current management and challenges of malignant disease in the CNS in paediatric leukaemia. Lancet Oncol 9:257–268
Cauley KA (2015) Fluoroscopically guided lumbar puncture. AJR Am J Roentgenol 205:W442–W450
Eskey CJ, Ogilvy CS (2001) Fluoroscopy-guided lumbar puncture: decreased frequency of traumatic tap and implications for the assessment of CT-negative acute subarachnoid hemorrhage. AJNR Am J Neuroradiol 22:571–576
Brenner DJ, Hall EJ (2007) Computed tomography — an increasing source of radiation exposure. N Engl J Med 357:2277–2284
Coley BD, Shiels WE, Hogan MJ (2001) Diagnostic and interventional ultrasonography in neonatal and infant lumbar puncture. Pediatr Radiol 31:399–402
Wang PI, Wang AC, Naidu JO et al (2013) Sonographically guided lumbar puncture in pediatric patients. J Ultrasound Med 32:2191–2197
Mazor SS, McNulty JE, Roosevelt GE (2003) Interpretation of traumatic lumbar punctures: who can go home? Pediatrics 111:525–528
Kim S, Adler DK (2014) Ultrasound-assisted lumbar puncture in pediatric emergency medicine. J Emerg Med 47:59–64
Muthusami P, Robinson AJ, Shroff MM (2017) Ultrasound guidance for difficult lumbar puncture in children: pearls and pitfalls. Pediatr Radiol 47:822–830
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Pierce, D.B., Shivaram, G., Koo, K.S.H. et al. Ultrasound-guided lumbar puncture in pediatric patients: technical success and safety. Pediatr Radiol 48, 875–881 (2018). https://doi.org/10.1007/s00247-018-4091-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4091-2