Abstract
Obesity is a chronic disease that is now a global epidemic. The numbers of obese people are exponentially rising in Europe, and it is projected that in Europe by 2010 there will be 150 million obese people. The obesity-related health crisis does not only affect adults, with one in four European children now overweight. Radiologists, both adult and paediatric, need to be aware of the magnitude of the problem, and obese patients cannot be denied radiologic evaluation due to their size. Missed diagnosis, appointment cancellation and embarrassing situations for patients when they are referred for a radiological examination for which they are not suitable are all issues that can be avoided if careful provision is made to accommodate the needs of the obese patient requiring radiologic evaluation. This paper will discuss the epidemiology of obesity and the role of radiology in the assessment of obesity and disorders of fat metabolism. The limitations obesity poses to current radiological equipment and how the radiologist can optimise imaging in the obese patient will be described. Dose reference levels and dose control are discussed. Examples of how obesity both hinders and helps the radiologist will be illustrated. Techniques and pre-procedural preparation to help the obese patient in the interventional suite are discussed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obesity is one of the great public health challenges of the 21st century. The numbers of obese adults and children are exponentially rising in Europe following trends in the USA. It is projected that in Europe by 2010 there will be 150 million obese people [1]. The obese population of Europe has tripled over the last 20 years, with now half of all adults overweight and ten times as many children overweight than in the 1970s. The gravity of the situation prompted the world’s first anti-obesity charter to be created by 53 European countries in 2006 [2]. The goals of the charter were to recognise the obesity epidemic and to promote change to try and reverse the problem.
The combination of high caloric intake and low energy expenditure with genetic and hormonal factors in which we live is creating an epidemic of obese people with significant associated morbidities. Attitudes, equipment and expertise in the health-care sector need to adapt to this growing population of patients. The impact this enlarging population will have on the health sector is huge, with 6% of European health-care budgets currently spent on obesity-related disease [2].
Radiology departments are not exempt as there will be an increased demand for radiologic evaluation of obese patients. All too often, however, an obese patient is referred for examinations that are inappropriate, leading to missed diagnosis or appointment cancellation. For example, the referral of an obese man for abdomen ultrasound to evaluate for pancreatic lesion is unlikely to lead to a positive diagnosis as the pancreas may not even be seen. If the patient is referred subsequently or directly to CT, technical difficulties due to table weight and gantry diameter limits may prevent the patient from being examined. Image quality may be suboptimal due to artefact, and significant dose increases may be required. The psychosocial impact for the patient who arrives but is declared unsuitable for the machine is impossible to measure. It is the responsibility of radiologists to convey these difficulties to referring physicians to promote the appropriate selection of imaging investigations for the patient and clinical indication in question.
Within the department, standard weight limits and gantry diameters should be known to prevent the patient presenting for a radiological investigation (e.g. CT) and subsequently being declined due to their size. Familiarity with options to improve image quality will reduce the number of suboptimal studies, and these will be discussed. Significant dose increases are often required to improve image quality, and although this is necessary to achieve diagnostic quality images, radiation protection issues for both the patient, the radiologist and the ancillary staff must be carefully considered. Technological advances in US, fluoroscopy, CT and MRI and image optimisation suggestions will be described.
Radiological techniques, in particular MRI, are now at the forefront in the diagnosis and management of disorders of fat metabolism. The advent of cross-sectional imaging has also led to the quantification of body fat and correlation with risk of insulin resistance for an individual depending on their fat distribution.
In this paper the epidemiology of obesity, the utility of radiology in the diagnosis of fat disorders, the hindrance obesity poses to diagnostic imaging (Table 1) and imaging optimisation techniques will be discussed. Dose management in obesity will be addressed. How best to cope with the challenges of the obese patient who presents to the interventional suite will be described.
Epidemiology of the obesity epidemic
The International Taskforce on Obesity (IOTF) reviewed the available national data from European countries in 2002 and found that the prevalence of obesity in Europe was 15–20% [3], but the figures are rising each year. The most up-to-date IOTF data from May 2008 estimate that over 50% of Europeans are overweight (Table 2). The average body mass index in Europe is 26.5 kg/m2 and is classified according to the WHO as ‘overweight’. The gap between rates from available data in the old eastern European countries and Western European countries is closing. If current trends continue, by 2010 there will be 150 million obese adults and 15 million obese children in Europe [1].
The evolution of the epidemic was recently described by Ludwig in The New England Journal of Medicine [4]: in the 1970s there was an average weight increase that has now led to weight-related diseases emerging in the 2000s. For the future, we can expect the emergence of the third phase of the epidemic where serious life-threatening conditions will occur secondary to obesity. Ludwig described these phases of obesity with particular reference to obesity in children. The rising rate of obesity in children and adolescents is of great concern. One in four European children is overweight [3, 5]. The risk of a child becoming obese is increased if one of both parents is obese or if they belong to a lower socio-economic group. In all European countries surveyed by the WHO in 2001/2002, there were more overweight girls than boys. With the early onset of obesity, children are at risk of developing conditions previously considered ‘adult’ disorders, such as non-alcoholic fatty liver disease and type 2 diabetes [6]. The consequence of obesity-related disease in adolescents and young adults is the prospect of early morbidity and mortality in their lives (Olshansky et al. estimate a reduction in lifespan of 2–5 years [7]).
Evaluation of body fat
There are several ways to evaluate body fat. These include techniques based on either anthropometric (body mass index, waist circumference, skin fold thickness), scientific (biometric impedance, water displacement) or radiologic techniques (DEXA, CT, MRI). Obesity is defined by the WHO and National Institute of Health in terms of the ratio of body mass to body height (kg/m2). A body mass index of 25–30 kg/m2 is considered overweight; >30 kg/m2 is obese, with >40 kg/m2 defined as morbidly obese.
Epidemiological data have shown that increased BMI is a marker for increased risk of many diseases, in particular cardiovascular disease and diabetes [8]. Obese individuals are at risk of developing the ‘metabolic syndrome’. This syndrome is diagnosed in a patient with insulin resistance as well as two of the following: abdominal obesity, dyslipidaemia, hypertension, pro-thrombotic state or a pro-inflammatory state. The significance of identifying the disorder is to identify those at risk of cardiovascular disease and diabetes. The impact of obesity on the body is not confined to one system. Pulmonary disease, such as obstructive sleep apnoea, incidence of certain cancers, such as uterine, cervical and renal cancer, osteoarthritis, gout and venous stasis are all more common in obese patients. Radiologist will encounter many obese patients with these secondary problems in their daily practice. The presence of obesity should alert the radiologist to the increased risk of these conditions.
BMI as an index of obesity has its limitations. BMI provides an indirect measurement of body fat and is unable to differentiate between lean mass and fat mass or to characterise the distribution of body fat (predominantly subcutaneous or intra abdominal). The inability to define lean mass from fat mass can lead to lean muscular individuals being defined as obese. BMI must also be corrected for age, gender and ethnicity [9]. Middle aged and older people have greater fat deposits than younger people with less lean mass. For children the same index, the BMI, is used to assess body fat, but it is interpreted according to gender- and age-specific percentile charts. The distribution of fat is also dependant on gender [10], with women typically having the gynaecoid distribution of fat around the hips and men the android pattern where adiposity is predominantly central. Women also have a higher percentage of body fat [11]. The pattern of distribution of fat can impact image quality in ultrasound in particular, an ultrasound in an obese female with fat predominantly in the pelvic region will be better quality than a male patient who weighs the same amount, but has central fat.
Percentage body fat varies among different ethnic groups; the Asian population has a higher percentage of body fat than their Caucasian equivalents [12]. The ethnic difference is most likely explained by differences in trunk-length ratio and muscularity. BMI cutoffs are adjusted to allow for this, with lower levels being more significant in the Asian population.
Radiologic techniques such as DEXA, CT and MRI provide direct assessment of body fat and fat distribution. With the advent of cross-sectional imaging with computed tomography and magnetic resonance imaging, there is now greater understanding of the significance of visceral and subcutaneous fat [13]. It is felt that intra-abdominal and visceral fat carries a greater metabolic risk to the individual [14].
Computed tomographic (CT) imaging at a predetermined level in the abdomen (standard protocol is to select a 1-cm axial slice through the pedicles at L4/L5) utilising available software programmes (e.g. NIH Image™ or SliceOmatic™ on MRI and for CT: Fatscan™ software) can calculate percentages of fat distribution [15, 16] (Fig. 1).
Cross-sectional imaging in patients with neurologic disorders may incidentally detect replacement of muscle by fat. It has been shown that the replacement of muscle by lipid is a risk factor for insulin resistance, and this should be mentioned in reports (Fig. 2) [17]. Although CT has been shown to be an accurate means of calculating body fat, its distribution is limited by radiation dose.
Magnetic resonance imaging is radiation free, and rapid imaging protocols have been devised that provide automated assessment of body fat [18, 19]. A potential limitation of automated computer-assisted techniques for calculating body fat on MRI is the inclusion of bone marrow fat in the calculations. Bone marrow fat has not been shown to confer a risk of insulin resistance to the patient, and therefore it should not be included in calculations. Mantatzis et al. propose a method of anatomic segmentation to try and overcome this [20].
MRI has been shown to have a role in the diagnosis and management of patients with lipodystrophy syndromes. The commonest lipodystrophy syndromes seen in clinical practice are those that are inherited, such as the Donnegan-Kobberling variety, and those that are acquired, such as the lipodystrophy syndrome that occurs in HIV patients taking antiretroviral medications. The lipodystrophy syndrome is characterised by central adiposity, peripheral lipoatrophy and metabolic abnormalities. MRI imaging can be very useful in the radiologic assessment of PCOS (a component of the metabolic syndrome) where trans-abdominal ultrasound is not diagnostic due to obesity or trans-vaginal ultrasound is unsuitable due to age or other factors.
Obesity: The radiologic challenges and solutions
Plain film radiography
Standard cassette sizes are too small to cover the dimensions of an obese patient (14 × 17-inch cassette). If the area of interest is covered on the film, it can frequently be coned off due to magnification. A solution to this is to use multiple cassettes to achieve coverage. Two factors contribute to reduced image quality in the obese patient: attenuation of the X-ray beam by increased body fat causes contrast to be reduced and noise to be increased; secondly, increased exposure time results in a greater risk of motion artefact. Image quality can be improved manually by increasing the Kvp and mAs; for example, the standard chest X-ray dose is kVp of 90–95 with mAs of 2–2.5, but this should be increased to 100 and 4 for the obese patient [21]. In modern radiographic equipment, the ‘automated exposure control’ (AEC) serves as an automated way to control the dose received on the image receptor. Ideally, exposure is automatically terminated at a level when the predetermined receptor dose, corresponding to optimum image quality, has been reached. For obese patients, the AEC acts to increase exposure factors to achieve this level. In the event of failure of the AEC, a backup timer terminates the exposure. The maximum exposure before the backup timer is activated is 600 mAs or 6s (38). These levels are adequate for most patient sizes and studies. On some systems it is possible to set lower mAs values for dose termination. While this limits the level of overexposure to a patient in the event of an AEC failure, care must be taken that this setting is adjusted appropriately when imaging obese patients.
A grid is required to reduce scatter. Digital viewing permits adjustment of the window level and width to achieve improved contrast.
Fluoroscopy
With the advent of bariatric surgery, the utility of upper gastrointestinal barium series has been rediscovered. The two main types of weight reduction surgical interventions are restrictive or malabsoprtive, including the Roux-en-Y gastric bypass, laparoscopic adjustable gastric banding, vertical-banded gastroplasty, jejunoileal bypass, simple biliopancreatic diversion or biliopancreatic diversion with duodenal switch [22]. In symptomatic patients who have undergone bypass or stomach volume reduction surgery, upper GI series can provide useful information about the anatomy and any leaks, fistula or obstruction. Following gastric banding, it is recommended that the patient be referred for annual upper GI series [23]. Other indications include if the expected weight loss is not achieved or if the patient develops symptoms of bloating, vomiting or pain (Fig. 3). Radiologists need to be aware of the anatomy of the commonly used surgical techniques and commonly used devices [23, 24] (Fig. 4a and b).
CT images in a patient who presented with sepsis post-gastric banding surgery. (a) There is evidence of free intra-peritoneal air (arrow) with the inserted band seen in the stomach region (circle); (b) shows the subcutaneous port (circle), which is then attached by a small catheter to the gastric band. A fluid collection is seen anterior to the liver (arrow)
Fluoroscopy is also used in the operating theatre to guided screw placement, for example in orthopaedics. Handolin et al. found that they could not achieve sufficient contrast resolution in morbidly obese patients undergoing hip replacement, and injection of contrast into the hip joint was required to improve intraoperative visualisation of the femoral head [25].
Using fluoroscopy in the obese patient is limited by the table-to-image intensifier diameter and the table weight limits (45 cm and 159 kg) (Table 3). Newer flat-panel units allow girths of less than 60 cm and weights up to 317.5 kg. Digital detectors allow for greater table-to-detector distance and greater detector area.
Exposure factors are also under the control of AEC or automated brightness control (ABC) in fluoroscopy systems. Manual exposures are not permitted by many fluoroscopy systems. Some systems will, however, allow the operator to supplement the dose by selection of programs specifically adapted for a particular examination. If the system has reached the maximum exposure rate allowed, image brightness may also be increased by opening the aperture to the camera or by increasing the electronic gain in the video amplifiers: however, with exposure rates held constant, both these methods also increase image noise.
Interventional radiology
Poor image quality in interventional radiology fluoroscopic procedures on obese patients can lead to prolonged procedures. Using magnification, road maps and images fade and help, but the trade-off is the balance of dose from prolonged procedures to the increased dose utilised by these methods. The AEC in the system adapts to the increased mass and adjusts exposure settings for fluoroscopy. When a digital imaging is acquired, the dose per frame may be determined by the screening dose rates, and so increased dose per frame occurs. Software in the system can also allow the radiographer to increase the exposure. If these higher dose rates are selected for an obese patient, care must be taken to revert to standard settings when the next patient is on the table as no cue exists to prompt a dose reduction. High quality images will be seen by the operator, but these may be acquired at an unnecessarily high dose.
In the obese patient undergoing fluoroscopic-guided procedures, there can be high skin doses due to high absorption of low-dose photons at the skin surface [26]. Many of the documented skin injuries have occurred in obese patients, especially those with increased susceptibility due to diabetes. A solution to this problem is to rotate the beam to better distribute the dose. As with all patients, whether obese or not, keeping the tube at a safe distance from the patient, the image intensifier close to the patient and using pulsed fluoroscopy can help to reduce the dose. The increased dose utilised in obese patients undergoing prolonged procedures should be monitored. In the future, where high doses are used and the risk of skin burns and deterministic effects of radiation may be encountered, follow-up may be required. Departmental protocols that advise follow-up by a physician familiar with the clinical appearance of radiation burns may be indicated.
Ultrasound
Ultrasound is the radiological investigation most affected by obesity [21, 27]. The phrase ‘limited by body habitus’ is frequently found in ultrasound reports (Fig. 5). Increased fat leads to poor penetration of sound waves beyond the focal point and increased attenuation of the sound beam (by 0.63 dB/cm). Uppot et al. note that the distribution of body fat is significant when considering whether ultrasound images are going to be diagnostic in the obese patient: subcutaneous fat poses the greatest problem as it impacts the beam penetration en route to visualisation of the liver, for example. On the other hand, the pancreas will be difficult to visualise in someone with excess intra-abdominal or subcutaneous fat [21].
The advent of low-frequency curvilinear frequency probes (1-5 mHz) can allow better depth visualisation (up to 30 cm). New crystal designs that maximise the efficiency of the piezoelectric crystal are available. Tissue aberration correction technology allows the system to detect altered beam penetration through fat tissue and to correct the image created to achieve better contrast and fewer artefacts. Ultrasound techniques such as tissue harmonic imaging and pulse inversion harmonic imaging have been shown to have better imaging resolution and fewer artefacts in the obese patient [28, 29] (Fig. 6a and b). Improved ultrasound images in the obese patient can reduce overall examination time and sonographer fatigue and reduce subsequent referral for CT/MRI due to non-diagnostic ultrasound.
Computed tomography
As a rule of thumb for CT imaging, if the patient can fit in the scanner (aperture diameter 70 cm), the images are usually diagnostic. If necessary, the patient can be placed on the table feet first if their thoracic girth would prevent imaging of their abdomen. The standard CT scanner table weight limit is currently 205 kg; newer machines can accommodate weights of 308 kg with increased aperture diameters of 90 cm (Table 3). Goldsmith et al. described a novel idea for CT evaluation of the brain in obese patients who were unsuitable for standard machines. These obese patients stood behind the gantry and their head was placed prone into the cradle on the CT table; the image was acquired with the gantry moving in a caudo-cranial direction [30].
Fat can help in the assessment of intra-abdominal organs as it separates the intra-abdominal structures (Fig. 7). Clinical examination is difficult in the obese patient, and adenopathy, masses and hernias can be missed, making the value of radiologic evaluation even greater (Fig. 8). Excess mediastinal fat deposits can appear as mediastinal widening on chest X-ray. In the appropriate clinical context, this can raise the suspicion of mediastinal haematoma or aortic dissection, but CT can confirm that the widening is attributed to fat, not haematoma (Fig. 9a and b).
(a) Chest X-ray of a 65-year-old gentleman who presented with chest pain and low blood pressure shows a widened mediastinum. Clinicians in the emergency department rushed the patient to the CT scanner with the concern of a dissecting aneurysm. (b) Contrast-enhanced CT of the thorax reveals the apparent mediastinal widening is due to intra-mediastinal fat and not mediastinal haematoma or aortic dissection
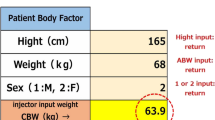
If an obese patient is suitable for CT, the two major issues are the increased dose they will suffer and the artefacts that will degrade their images. The exposure factors are selected by the radiographer in older units. In newer systems, tube current modulation is a very important way of dose control. This software adjusts the mA to the required level for the individual depending on the 3D mass. The artefacts that are seen are beam hardening due to disparity between girth and the field of view (Fig. 10) and increased noise due to poor beam penetration and beam scatter (Fig. 11). Beam hardening can obscure visualisation of organs of interest. A potential solution is to move the patient in the gantry to improve visualisation of the area [31]. Noise can be reduced by increasing the kvp (to 140) and the effective mAs. Thicker slices and thicker collimation can improve the signal-to-noise ratio [32]. Decreasing gantry speed and using tube current modulation can also reduce noise.
Obese patients are at high risk of cardiovascular disease, and the emergence of cardiac imaging protocols is allowing non-invasive cardiac assessment for these patients. Certain modifications must be made to optimise imaging in these patients. In obese patients weight-based contrast dose calculations (1 ml/kg) should be used to achieve diagnostic enhancement of the vasculature [33, 34]. The advent of dual-source CT in 2005 has allowed many morbidly obese patients to undergo cardiac CT who previously would have been unsuitable. Using a total of 160 KW of power from two independent ray sources enables better tissue penetration and less noise. Although the increased power can result in increased dose, the increased temporal resolution of dual-source CT (83 ms) means that patients are scanned much faster so the exposure time is less [35]. Inbuilt software, such as ECG gated modulation, helps in dose reduction.
Magnetic resonance imaging
MRI is faced by many limitations when the obese patient presents for imaging: the table weight limit, the aperture diameter, bore length and image quality (reduced contrast and signal-to-noise ratio, field of view limitations and artefacts). Standard bore magnets have aperture diameters of 60 cm with a table weight limit of 159 kg (Table 3). Many patients cannot fit these criteria and are referred for vertical-field open MRI with apertures of 40–45 cm and weight limits of up to 250 kg. Open/ vertical MRI systems have the advantage of horizontal diameter of the open machines as big as 160 cm, but the limitations of open MRI are the vertical aperture diameter of 45 cm (the full diameter of the aperture, less space available when you include the table) and lower Tesla magnets and weaker gradients (usually <1 T). Klein et al. found that although open MRI with a 0.35-T magnet could provide anatomic information about the heart, for perfusion or functional studies, higher field strengths were needed [36]. Weaker gradients of open MRI systems result in reduced signal-to-noise ratio (SNR). By increasing gradient strength, SNR can improve, but depth penetration is unchanged [37]. SNR is linearly proportional to voxel volume. Voxel volume depends on the field of view (FOV), slice thickness and the matrix size, all of which may be varied with patient size. As the voxel size increases, spatial resolution decreases. Signal strength and acquisition times may be increased to improve image quality. Increasing signal strength is limited by controls over radiofrequency power deposition. Systems will have a normal mode suitable for all patients, and a higher intensity mode (which may increase energy deposition up to 4 W/kg) defined as a first level control mode requiring medical supervision. For example, an MRI system may prompt the operator to increase signal intensity, but also flag the affect this will have on the specific absorption rate (W/kg). The operator has the option of accepting the increased intensity for the particular patient or adjusting other parameters such as TR or flip angle as appropriate. Increasing acquisition times in patients who are confined in a closed space may exacerbate problems for claustrophobic patients and may lead to increased problems with motion artefacts.
The challenge of balancing the space required to accommodate the patient without losing image quality has been embraced by technology with new designs allowing a 1.5-T magnet and shorter bore (125 cm and an aperture diameter of 70 cm). Shorter bore magnets allow the patient to lie with their head and shoulders outside the bore and are therefore better tolerated.
Larger field of view to image the obese patient results in loss of contrast-to-noise resolution and wrap-around artefacts when the field of view is exceeded. Standard closed-bore magnets allow a field of view of 40–50 cm with open magnets covering 35–40 cm. This can be too small, and in the obese patient the area of interest can exceed the field of view, and wrap-around artefact creeps in with a loss in CNR also. Multi-step image may be required to cover the area of interest, while respecting the field of view. New coil technology combined with moving table techniques can create a ‘virtual’ field of view of up to 205 cm [37]. The radio-frequency coils placed on the patient in the bore are also usually unsuitable for the obese patient, even making bigger coils a limited solution as with bigger coils there is a loss of SNR. New coil designs have increased the numbers of modular elements that wrap around the larger patient, and there is improved CNR [37].
It is important to remember that there is a risk to the obese patient of skin burns when their girth is such that their skin is very close to the gantry [38]. In an ill obese ICU patient who is clammy, for example, sweat on their skin surface can act as a conductor and increase the risk of burns. A cloth or cotton wool should be placed between their arms and the bore. Using saturation bands can reduce the noise created by excess subcutaneous fat [37].
Nuclear medicine
As with the other modalities, the two main issues are the physical problem of the obese patient on the equipment and the image quality problem if the patient is suitable for the equipment. Unlike CT and fluoroscopy, no automated system to ensure adequate exposure exists. In nuclear medicine a standard dose of isotope for the given study is injected, and the only variables are the scan time allowed and to what degree the individual attenuates the signal (depending on their mass, for example, low doses are given to children, but they can be good emitters as they have little fat/mass to attenuate the signal).
Doses of radiolabelled isotope should conform to published dose reference levels [38, 39]. In paediatric imaging, however, these doses are factored down to take account of the reduced body mass and to reduce the dose. There is no generally accepted corresponding method for increasing dose to larger patients. The standardised reference level is based on a 70-kg person; with the majority of Europeans now overweight, this standard level may be an underestimation of the ‘standard’ individual. Centres may have to consider creating local DRLs for obese patients in order to monitor dose control in this important and increasing demographic.
Using longer data acquisitions and varied positioning techniques (for example, the obese patient that exceeds table weight limits can be imaged sitting in their chair/bed), quality can be improved [41]. Longer data acquisitions, as for all radiological investigations, increase the chance of motion artefact. With weight-based increased dose administration, there is increased dose to the patient, the injector and associated staff involved in the imaging. In PET imaging, obesity causes increased scatter and photon attenuation [42]. A solution to the increased staff dose is to rotate staff so less time is spent with the patient [43]. Patient preparation can also take longer as obtaining intravenous access can be a challenge in the obese patient.
Managing the obese patient in the interventional room
The obese patient is a high-risk patient in the interventional suite. Transfer to the department on re-enforced beds and wheel chairs is required, and assistance is required for the transfer onto the fluoroscopy table. It is preferable if intravenous sedation is being used to sedate once the patient is on the table. It is important that the nursing staff and radiologists are aware of the increased risk of respiratory compromise in the obese patient and that continuous monitoring is performed with appropriate blood pressure cuffs. Lying the obese patient in a prone position can induce hypoxia, and consideration should be given to positioning the patient in a lateral decubitus position for procedures such as percutaneous nephrostomy [44]. Intravenous access can be difficult to obtain in the obese patient, and portable ultrasound may be required. Palpation of the femoral artery can be difficult due to excess fat in the inguinal region, but also due to over-hanging intra-abdominal fat, and the obese patient is at increased risk of pseudo aneurysm formation as a result [44]. Devices such as the KangaruWeb™, which is an apron that holds back the ‘apron’ of abdominal fat during the procedure, can be helpful. Standard needle lengths can be too short for the obese patient. Chan et al. noted injection granulomas in the buttocks of many obese patients undergoing pelvis CT. This incidental observation prompted a study of intra-muscular injections, and it was found that the likelihood of successful intramuscular delivery of medication with standard needle lengths was inversely proportional to the thickness of gluteal muscle fat (Fig. 12). This is of significance as the medication is designed with pharmacokinetics for intra-muscular delivery, not delivery into the subcutaneous fat [46]. Image guidance and longer spinal needles can be required to perform CSF sampling in an obese patient. Fluoroscopic guidance usually helps the physician when the blind approach has not been successful. Halder et al. found the only option for obtaining CSF from an obese patient in the intensive care unit was serial plain film image guidance as the patient was too obese for the fluoroscopy or CT table [47].
(a) Successful intramuscular deposition of medication has been achieved in a thin patient as indicated by a small air pocket in the glutueal muscle (arrow). (b) Increasd gluteal subcutaneous fat has resulted in the standard needle not reaching the gluteal muscle, and the medication has been delivered into the subcutaneous fat (arrow)
Conclusion
Obesity in Europe is an acute health issue that requires urgent attention. As well as governmental and community policies, local departmental policies must be adapted to be able to care for the increasing obese population. Attitudes and protocols in every radiology department must change to permit good treatment of every individual with weight-related diseases. Obese patients should not be denied radiologic evaluation due to their size. Although in the public sector it may not be practical and all departments will not have the new technological advances that have been shown to be able to image the obese patient, governments and health boards must ensure that when required the equipment is available in the same city or region. On a departmental level, familiarity with obesity-related diseases, obesity-related mimics, bariatric surgery anatomy and devices, image optimisation with available equipment and obesity-related risks and pitfalls in the interventional radiology patient as described in this paper is required.
Currently, dose increase is one of the main options to improve image quality in obese patients. The dose issue in this group needs careful control and adherence to the ALARA principle. At present, dose reference levels are standardised to a 70-kg person with those over 90 kg and less than 50 kg excluded. The average BMI of a European in 2008 is overweight, and this standardisation may need to be adjusted to take this change in demographics into account. Protocols exist for dose reduction in paediatrics, but not always for dose increases if an institution encounters large volumes of obese patients. In the future, this seems to be the reality we will encounter, and we need to be prepared.
References
WHO Global InfoBase online [online database]. Geneva, World Health Organization, 2007 (noncommunicable diseases, comparable estimates; http://www.who.int/ncd_surveillance/infobase/web/InfoBaseCommon, 7accessed 8 April 2007)
WHO, European Charter on Counteracting Obesity. EUR/06/5062700/8 http://www.euro.who.int/Document/E89567.pdf date of access 8th June 2008
Obesity in Europe, The Case For Action (2002) International Taskforce on Obesity and European Association for the Study of Obesity, London. http://www.iotf.org/media/euobesity.pdf date of access 8th June 2008
Ludwig DS (2007) Childhood obesity the shape of things to come. NEJM 357(23):2325–2327, Dec. 6
Dietz WH (1998) Health consequences of obesity in youth: Childhood predictors of adult disease. Pediatrics 101:518–525
Lobstein T, Frelut M-L (2003) Prevalence of overweight among children in Europe. Obesity Reviews 4(4):195–200
Olshansky SJ, Passaro DJ, Hershow RC et al (2005) A potential decline in life expectancy in the United States in the 21st Century. NEJM 352:1138–1145
National Institutes of Health and National Heart, Lung, and Blood Institute (1998) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. Obes Res 6(suppl 2):1S–209S
Snijder MB, Van Dam RM, Visser M, Seidell JC (2006) What aspects of body fat are particularly hazardous and how do we measure them. Int J Epidemiol 35(1):83–92, Feb, Epub 2005 Dec 8. Review
Rattarsan C, Leelawattana R, Soonthompun S, Setasuban W, Thamprasit A (2004) Gender differences of regional abdominal fat and their relationships with insulin sensitivity in healthy and glucose intolerant Thais. J Endocinol Metab 89:6266–6270
Shaw NJ, Crabtree NJ, Kibirige M, Fordham JN (2007) Ethnic and gender differences in body fat in British school children as measured by DXA. Arch Dis Child 92(10):872–875, Oct, Epub 2007 May 23
Gurrici S, Hartriyanti Y, Hautvast JG, Deurenberg P (2001) Relationship between body fat and body mass index: differences between Indonesians and Dutch Caucasians. Br J Nutr 85:239–242
Bjorntorp P (1988) The associations between obesity, adipose tissue distribution and disease. Acta Med Scand Suppl 1404–1411
Prineas RJ, Folsom AR, Kaye SA (1993) Central adiposity and increased risk of coronary disease mortality in older women. Ann Epidemiol 3:35041
Tokunaga K, Matsuzawa Y, Ishikawa K, Tarui S (1983) A novel technique for the determination of body fat by computed tomography. Int J Obes 7:437–445
Kobayashi J, Tadokoro N, Watanabe M, Shinomiya M (2002) A novel method of measuring intra-abdominal fat volume using helical computed tomography. Int J Obes Relat Metab Disord Mar 26(3):398–402
Maruyama Y, Mizuguchi M, Yaginuma T, Kusaka M, Yoshida H, Yokoyama K, Kasahara Y, Hosoya T (2008) Serum leptin, abdominal obesity and the metabolic syndrome in individuals with chronic spinal cord injury. Spinal Cord. [Epub ahead of print] Jan 2, doi:10.1038/sj.sc.3102171
Brennan DD, Whelan PF, Robinson K, Ghita O, O’Brien J, Sadleir R, Eustace S (2005) Rapid automated measurement of body fat distribution from whole-body MRI. AJR 185:418–423
Gerard EL, Snow RC, Kennedy DN, Frisch RE, Guimaraes AR, Barbieri RL, Sorensen AG, Egglin TK, Rosen R (1991) Overall body fat and regional fat distribution in young women: Quantification with MR imaging. AJR 157:99–104
Mantatzis M, Prassopoulos P (2007) Total body fat visceral fat subcutaneous fat bone marrow fat. What is important to measure. AJR 189:W386
Uppot RN (2007) Impact of obesity on radiology. Radiol Clin North Am 45(2):231–246, Mar, Review
Chalndler RC, Srinivas G, Chintapalli KN, Schweisinger WH, Prasad SR (2008) Imaging in bariatric surgery: A guide to postsurgical anatomy and common complications. AJR Am J Roentgenol 190(1):122–135, Jan, Review
Blachar A, blank A, Gavert N, Metzer U, Fluser G, Abu-Abeid S (2007) Laparoscopic adjustable gastric banding surgery for morbid obesity: imaging of normal anatomic features and post operative complications. AJR 188:472–479
Chandler RC, Srinivas G, Chintapalli KN, Schwesinger WH, Prasad SR (2008) Imaging in bariatric surgery: A guide to postsurgical anatomy and common complications. AJR Am J Roentgenol 190(1):122–135, Jan
Handolin LE, Hiltunin OJ (2006) Peroperative difficulties in fluoroscopy of the femoral head in massive obese patient: enhanced visualization by intra-articular contrast agent. Arch Orthop Trauma Surg 126(7):498–499, Sep, Epub 2006 Jun 21
Bryk S, Censullo M, Wagner L, Rossman L, Cohen A (2006) Endovascular and interventional procedures in obese patients: A review of procedural technique modifications and radiation management. J Vascular Interventional Radiol 1(17):27–33
Uppot RN, Sahani DV, Hahn PF, Kalra MK, Saini SS, Mueller PR (2006) Effect of obesity on image quality: 15-year longitudinal study for evaluation of dictated radiology reports. Radiology 240(2):435–439, Aug, Epub 2006 Jun 26
Hong HS, Han JK, Kim TK, Kim YH, Kim JS, Cha JH, Choi BI (2001) Ultrasonographic evaluation of the gallbladder: Comparison of fundamental tissue harmonic and pulse inversion harmonic imaging. Ultrasound Med 20(1):35–41, Jan
Rosenthal SJ, Jones PH, Wetzel LH (2001) Phase inversion tissue harmonic sonographic imaging: A clinical utility study. AJR Am J Roentgenol 176(6):1393–1398, Jun
Goldsmith P, Patel A, Farmer R, Wright G, Brown J (2008) A novel technique for CT imaging the brain of the obese patient. Clin Rad 62:575–576, May
Coulden RA, Dixon AK (1987) Avoidance of ring artifacts in lumbar spine computed tomography in obese patients. [Letter] British Journal of Radiology 60(713):518
Vannier MW, Johnson PJ, Dachman A et al (2005) Multi detector CT of massively obese patients. Presented at RSNA, Chicago
Bae KT, Seeck BA, Hildebolt CF, Tao C, Zhu F, Kanematsu M, Woodard PK (2008) Contrast enhancement in cardiovascular MDCT: effect of body weight, height, body surface area body mass index and obesity. AJR Am J Roentgenol 190(3):777–784, Mar
Bae KT, Tao C, Gürel S, Hong C, Zhu F, Gebke TA, Milite M, Hildebolt CF (2007) Effect of patient weight and scanning duration on contrast enhancement during pulmonary multidetector CT angiography. Radiology 242(2):582–589, Feb
Achenbach S, Anders K, Kalender WA (2008) Dual-source cardiac computed tomography: image quality and dose considerations. Eur Radiol 18(6):1188–1198, Jun, Feb 26 [Epub ahead of print]
Klein HM, Meyners W, Neeb B, Labenz J, Truümmler KH (2007) Cardiac magnetic resonance imaging using an open 0.35 T system. J Comput Assist Tomogr 31(3):430–434, May-Jun
Uppot RN, Sheehan A, Seethamraju R (2005) Obesity and MR imaging. MRI Hot Topics, Siemens Medical www.usa.siemens/medical date of access 8th June 2008
European Commission. Criteria for Acceptability of Radiological (including Radiotherapy) and Nuclear Medicine Installation. Radiation Protection No 91, 1997
IPEM Report 88, Guidance on the establishment and use of Diagnostic Reference Levels for medical X-ray examinations, 2004
Uppot RN, Sahani DV, Hahn PF, Gervais D, Mueller PR (2007) Impact of obesity on medical imaging and image-guided intervention. AJR Am J Roentgenol 188(2):433–440, Feb Review
Silverman DH, Ratib O, Czernin J (2005) Optimizing imaging protocols for overweight and obese patients: a lutetium orthosilicate PET/CT study. [Clinical Trial. Journal Article] J Nuclear Med 46(4):603–607
Halpern BS, Dahlbom M, Auerbach MA, Schiepers C, Fueger BJ, Weber WA, Silverman DH, Ratib O, Czernin J (2005) Optimizing imaging protocols for overweight and obese patients: a lutetium orthosilicate PET/CT study. J Nucl Med 46(4):603–607, Apr
Botkin CD, Osman MM (2007) Prevalence, challenges, and solutions for 18F-FDG PET studies of obese patients: a technologist’s perspective. J Nuclear Med Technol 2(35):80–83
Gofrit ON, Shapiro A, Donchin Y, Bloom AI, Shenfeld OZ, Landau EH, Pode D (2007) Lateral decubitus position for percutaneous nephrolithotripsy in the morbidly obese or kyphotic patient. J Endourology 16(6):383–386
Shindo S, Kato K, Motohashi S, Kaga S, Inoue H, Matsumoto M (2007) Delayed femoral pseudoaneurysm formation after percutaneous coronary intervention. Clin Imag 31(3):162–164
Chan V, Persaud T, Buckley O, Colville J, Torreggiani WC (2006) Are buttock injections truly intra muscular? Eur J Radiol 2158(3):480–484, Feb, Epub 2006
Halder S, Wimbush S (2006) Radiologically assisted cerebrospinal fluid sampling in a morbidly obese patient. Crit Care Resusc 8(4):394
Acknowledgements
Ms Deborah Prior to Clinical Specialist Radiographer, MRI Department, AMNCH Tallaght
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Buckley, O., Ward, E., Ryan, A. et al. European obesity and the radiology department. What can we do to help?. Eur Radiol 19, 298–309 (2009). https://doi.org/10.1007/s00330-008-1154-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-008-1154-z