Abstract
Objective
To assess reduced volumes of contrast agent on image quality for coronary computed tomography angiography (CCTA) by using single-beat cardiac imaging with 320-slice CT.
Materials and methods
Forty consecutive male patients (mean age: 55.8 years) undergoing CCTA with body weight ≤85 kg, heart rate ≤65 bpm, and ejection fraction ≥55% were included. Image acquisition protocol was standardized (120 kV, 400 mA, and prospective ECG-triggered single-beat nonspiral CCTA). Patients were randomly assigned to one of four groups (G1: received 40 ml, G2: 50 ml, G3: 60 ml, G4: 70 ml). Groups were compared with respect to aortic attenuation, image noise, and image quality.
Results
CT values (mean ± standard deviation) in the aortic root were measured as 423 ± 38 HU in G1, and 471 ± 68, 463 ± 60, and 476 ± 78 HU in G2-4, respectively. There were no statistically significant differences in attenuation among the groups (P > 0.068). All 40 CT datasets were rated diagnostic, and image noise and image quality were not statistically different among groups.
Conclusion
Using 320-slice volume CT, diagnostic image quality can be achieved with 40 ml of contrast material in CCTA in patients with normal body weight, cardiac function, and low heart rate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tailored protocols for injection of contrast agents for cardiac and coronary computed tomography (CT) are essential to achieve optimal enhancement. A wide range of volumes and injection rates have been reported for coronary computed tomography angiography (CCTA) [1–5]. There is no available standard contrast protocol for CCTA of the coronary arteries although the need for less contrast material in CT systems with broader detector arrays and short acquisition times is anticipated.
A recently introduced 320-detector-row volume CT system has a detector width of 16 cm and can aquire a full cardiac CT dataset within a single heart beat. This represents a significant reduction in acquisition time compared to the 64-detector-row generation of CT systems, which typically acquire a dataset in 6–12 s [6, 7]. We hypothesized that the very fast, snap-shot-like, single-beat acquisition possible with the 320-detector-row CT system could be performed with a lower contrast dose than previously reported for 64-detector-row CT without adversely affecting image quality.
Our study was therefore designed to compare CCTA image quality across a range of contrast medium volumes in a homogeneous patient population with standardized examination parameters.
Materials and methods
Patients
Forty male patients were included in this prospective study. Patients ranged in age from 35 to 79 years (mean age: 56.8 years, median age: 58 years). Inclusion criteria were indication for coronary artery imaging using MDCT, male gender, body weight ≤85 kg, heart rate ≤65 beats per minute during CT data acquisition, and an ejection fraction of ≥55% as assessed by a standardized routine transthoracic echocardiography. Exclusion criteria were renal insufficiency with a serum creatinine level >1.5 mg/dl and contra-indications to iodinated contrast-enhanced computed tomography. In all patients, nitroglycerin was administered sublingually before the examination. Beta-blocking agents were administered orally to 25 patients before the examination in order to meet the heart rate inclusion criterion. Table 1 compares the patient’s body weight, body height, body mass index, and heart rate across the four patient groups. The study was approved by the local ethics committee, and informed consent was obtained from all patients.
Contrast medium injection protocols and CT acquisition
Each enrolled patient was randomly assigned to one of four contrast volume groups to create four groups of 10 patients. Total volume of contrast agent for each group was as follows: 40 ml (group 1, G1), 50 ml (group 2, G2), 60 ml (group 3, G3), and 70 ml (group 4, G4). Contrast medium (Iobitridol, Xenetix 350; Guerbet, Paris, France) was administered in all patients via an 18G IV cannula and using a dual-head–power injector (Dual Shot GX, Nemoto Kyorindo, Tokyo, Japan). Contrast material was injected at a flow rate of 5 ml/s followed by a 50 ml saline flush also injected at 5 ml/s. The delay to CT acquisition was determined using a bolus tracking technique (region of interest-based in the left atrium, attenuation threshold 200 HU, 6 s delay for delivery of the breath-hold command).
Prospectively ECG-triggered coronary artery CCTA was performed on a 320-slice CT system (Aquilion One, Toshiba, Nasu, Japan) using the following parameters: 120 kV tube voltage, 400 mA tube current, 350 ms gantry rotation time, 16 cm range. Data were acquired as targeted CCTA at 75% of the R-R interval using a single heart beat. The acquisition window ranged from 400 to 500 ms as determined by a test ECG before the examination. Images were reconstructed using a soft tissue kernel optimized for cardiac imaging (window center 75% of the R-R interval, image matrix 512 × 512, slice thickness 0.5 mm, interval 0.25 mm). The dose-length product (DLP) displayed on the system’s console was recorded. CT data sets were transferred to an off-line 3D workstation (Vitrea, Vital Images, Minnesota, USA) and further analyzed by two readers both experienced in cardiovascular radiology (10 and 4 years of experience).
Attenuation values and image noise
Attenuation values of vascular structures were measured in all patients by a single reader on axial images by using a manually defined circular ROI. Attenuation values were measured in the following structures: left atrium (LA), left ventricle (LV), ascending aorta (AAo), descending aorta (DAo), proximal right coronary artery (RCA), left main coronary artery (LMA), proximal left anterior descending artery (LAD), and proximal left circumflex artery (LCx). Attenuation values in the vessel lumen were measured in the most distal segment of LAD, LCX, and RCA in which measurements were not impaired by partial volume effects. Image noise of the coronary artery CT examination was assessed by measuring the standard deviation (SD) of the attenuation in an ROI placed in the AAo.
Image quality
Image quality was rated independently as diagnostic or nondiagnostic by both readers. A diagnostic examination allowed confident evaluation of obstructive coronary disease, whereas a nondiagnostic examination precluded a confident evaluation of obstructive coronary disease. All CCTA data sets were also assessed qualitatively by scoring the severity of motion or beam hardening artifacts as well as vessel attenuation in each coronary artery, including the marginal and diagonal branches. Each coronary segment was assigned a quality score on a rating system ranging from 1 (no motion artifacts, excellent visualization of vessel lumen) to 5 (massive motion artifacts, extensive disruption of vessel with nonvisualization of lumen).
Statistical analysis
Statistical analysis was performed using commercially available software (SPSS 15.0, SPSS, Chicago, IL). Baseline characteristics and attenuation values are expressed as the mean ± standard deviation (SD). The attenuation levels and image noise were compared among the groups using a t-test for independent samples. The two-sided Mann-Whitney U-test was used to compare image quality ratings among the different groups and baseline characteristics. The interobserver agreement for image quality ratings was calculated using kappa statistics. After Bonferroni correction, a P-value <0.016 was considered statistically significant.
Results
Coronary CTA was performed without any technical problems in all 40 patients. Baseline characteristics (Table 1) did not differ statistically significantly across the four groups (P > 0.12). The mean attenuation value in the AAo for G1–4 were 423 ± 38, 471 ± 68, 463 ± 60, and 476 ± 78 HU, respectively. G1 showed no statistically significantly different attenuation values in the AAo compared to G2 (P = 0.068). The attenuation value in the AAo was also not statistically different between G2 vs. G3 (P = 0.78), or G3 vs. G4 (P = 0.68). The attenuation values in the assessed coronary artery segments were lower in G1 compared to G2. However, the differences in attenuation values in the AAo and the evaluated coronary artery segments did not reach statistical significance (P > 0.025). The results of the analysis with respect to attenuation in the evaluated coronary artery segments and heart chambers are illustrated in Figs. 1 and 2.
Box plot illustrating attenuation values within the coronary arteries. The plot shows the range of data, the median value, and the upper and lower quartiles of the data sets. LMCA Left main coronary artery, LAD-p proximal left anterior descending artery, LAD-d distal left anterior descending artery, LCX-p proximal left circumflex artery, LCX-d distal left circumflex artery, RCA-p proximal right coronary artery, RCA-d distal right coronary artery
The mean noise value in the aortic root for the four groups was as follows: G1 21.9 ± 4.9 HU, G2 25.0 ± 4.9 HU, G3 27.0 ± 2.7 HU, and G4 25.9 ± 3.4 HU (P > 0.15 for all comparisons). Image quality was independently scored by both readers to be diagnostic in all 40 cases (100%; interobserver agreement, kappa = 1.0). There was no significant difference in image quality across groups receiving different contrast medium volumes. Table 2 summarizes the results of image quality ratings.
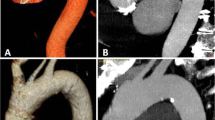
DLP of the coronary artery CCTA was recorded to range between 238.3 and 297.9 mGy·cm. Representative images and reconstructions are displayed in Figs. 3, 4, and 5.
Representative images and reconstructions of a patient in G1 (40 ml). The 55-year-old patient had a body weight of 77 kg, a body height of 1.79 m, a heart rate of 62 bpm, and a calculated mean attenuation in the ascending aorta of 410 HU. Depicted are 3D-rendered reconstructions, an axial image from the CCTA, and a curved multiplanar reconstruction of the right coronary artery
Image reconstructions of a 48-year-old patient in G1 (40 ml) with a body weight of 78 kg, a body height of 1.76 m, a heart rate of 58 bpm, and a calculated mean attenuation in the ascending aorta of 410 HU. A significant stenosis of the left anterior descending artery (LAD) with occlusion of the proximal D1 due to an atheromatous, noncalcified plaque is depicted by 3D-rendered reconstructions and a curved multiplanar reconstruction of the LAD. The attenuation of the examination is illustrated by an axial image from the CCTA
Image reconstructions of a 65-year-old patient in G2 (50 ml) with a body weight of 85 kg, a body height of 1.70 m, a heart rate of 55 bpm, and a calculated mean attenuation in the ascending aorta of 475 HU. The 3D-rendered reconstructions and a curved multiplanar reconstruction of the left anterior descending artery (LAD) illustrate atherosclerotic stenoses in the proximal and middle segment of the LAD. The attenuation of the examination is illustrated by an axial image from the CCTA
Discussion
Coronary CT angiography (CCTA) has benefited from rapid technological advancement in CT systems and is now recognized as a valuable noninvasive clinical tool to rule out coronary artery disease. The iodinated contrast agent used in CT imaging, including CCTA, has a dose-dependent association with contrast-induced nephropathy (CIN), which in turn is associated with increased morbidity and mortality [8, 9]. Despite a large number of studies and reviews on preventing CIN, the core recommendations of volume expansion, avoidance of nephrotoxic drugs, and, in particular, minimizing contrast dose have not changed [10–12]. Minimizing the volume of contrast medium used in CCTA is also important because patients with significant stenoses diagnosed on CCTA may require subsequent angioplasty during which they will be exposed to more contrast material.
Technical improvements of CT systems with broader detector arrays and faster image acquisition have been associated with a reduction in contrast medium volume from 160 ml on 4-slice CT systems to typically 75−100 ml for 64-slice systems [13–16]. The extremely short acquisition time (i.e., <1 s) of the prospective, ECG-triggered examination using the 320-slice CT system requires only a short window of coronary opacification. Contrast medium volumes of 40 ml produced similar image quality to larger volumes and were adequate for confident evaluation of the coronary tree.
Vascular attenuation is inversely related to a variety of anthropometric variables such as height, weight, body surface area (BSA), and body mass index (BMI) [17]. Nakaura et al. recommended calculating contrast medium volume and flow rate according to patient weight based on their results from 60 patients undergoing CCTA on a 64-slice system [18]. In our study we limited enrollment to male patients <85 kg in an attempt to increase the homogeneity of our study population and isolate differences in vascular attenuation to a difference in contrast medium volume. There were no significant differences in height, weight, BMI, or heart rate among groups receiving different contrast medium volumes in our study. Contrast protocol selection is a complex and essential component of diagnostic quality CCTA. Vascular attenuation is a product of not only the contrast volume, but the rate of administration, volume and rate of saline flush, and delay to CT acquisition. We chose to manipulate contrast medium volume while holding all other contrast and CT acquisition parameters fixed. For the sake of homogeneity, we did not adjust the contrast medium volume for patient weight, although we acknowledge this may be useful in extremes of body size.
Yamamuro et al. recently evaluated low contrast medium volume (40 vs. 50 ml) CCTA using a 64-slice system and were able to achieve mean attenuation values of more than 320 HU in both groups [19]. However, Yamamuro concluded that 0.9 ml/kg of contrast material was required for adequate attenuation. The mean body weight of his study population was only 58 kg. Translating these results to our patient population with a mean body weight ranging from 73.2 to 79.6 kg, calculated contrast medium volumes of 66–72 ml would have been required to achieve sufficient attenuation using a 64-slice CT system. The results of our study clearly show that a 320-slice CT system is capable of diagnostic image quality using contrast volumes of 40 ml. This result correlates to a respective mean 0.52 ml/kg contrast medium volume and must be considered superior to the one achieved in the study by Yamamuro (0.9 ml/kg).
Automated bolus-tracking with a fixed threshold level is necessary to achieve standardized, observer-independent CCTA examinations. In our study we used an attenuation trigger of 200 HU in the left atrium. We found that patient groups receiving 60 or 70 ml of contrast had mean attenuation values within the left atrium that were the same or higher than mean attenuation values in the ascending aorta. This suggests that for our study protocol (i.e., flow-rate, breath-hold delay, and bolus tracking), CT data were acquired while a portion of the contrast medium volume remained unused within the pulmonary vasculature or left heart chambers. A comparable effect might occur in the presence of reduced cardiac function and a fixed threshold level. Two techniques commonly used to avoid this effect are use of a test bolus and manual triggering. Using a test bolus requires an additional 10 ml of contrast, which is contrary to our study’s goal of contrast medium volume reduction. Manual triggering is operator-dependent and would have introduced bias into our results.
There are limitations to the study. The results of the study are only valid for the tested patient series and tested contrast agent with the respective iodine content. Targeted CCTA using a single beat is sufficient for coronary artery imaging at low radiation exposure, however, the evaluation of valve function or ejection fraction is not possible. Moreover low contrast medium volumes might impede the recently introduced assessment of myocardial enhancement. It should be noted that the results of our study reflect the specific injection parameters of our protocol and that by using 40 ml of contrast with different injection parameters, patient characteristics (i.e., heart rate, ejection fraction, obesity) could lead to reduced image quality. On the other hand, study designs manipulating other contrast injection variables may result in further reduction in contrast medium volumes (i.e., increasing contrast medium flow rate).
In conclusion, we compared four different volumes of contrast medium for coronary artery CCTA performed on a 320-slice CT system and found that 40 ml (mean 0.52 ml/kg) of contrast medium still produced diagnostic quality images in the tested series of patients. Further studies should evaluate alterations in higher injection flow rates to further reduce the necessary volume of contrast medium. Future work using 320-slice CT should be directed towards an individualization of coronary artery CT imaging and injection protocols to produce consistently high quality images with the lowest possible volume of contrast agent.
References
Roberts WT, Bax JJ, Davies LC (2008) Cardiac CT and CT coronary angiography: technology and application. Heart 94:781–792
Cademartiri F, Mollet NR, Runza G et al (2006) Improving diagnostic accuracy of MDCT coronary angiography in patients with mild heart rhythm irregularities using ECG editing. AJR Am J Roentgenol 186:634–638
Cademartiri F, Nieman K, van der Lugt A et al (2004) Intravenous contrast material administration at 16-detector row helical CT coronary angiography: test bolus versus bolus-tracking technique. Radiology 233:817–823
Becker CR, Hong C, Knez A et al (2003) Optimal contrast application for cardiac 4-detector-row computed tomography. Invest Radiol 38:690–694
Rist C, Nikolaou K, Kirchin MA et al (2006) Contrast bolus optimization for cardiac 16-slice computed tomography: comparison of contrast medium formulations containing 300 and 400 milligrams of iodine per milliliter. Invest Radiol 41:460–467
Miller JM, Dewey M, Vavere AL et al (2009) Coronary CT angiography using 64 detector rows: methods and design of the multi-centre trial CORE-64. Eur Radiol 19:816–828
Tatsugami F, Kanamoto T, Nakai G et al (2009) Reduction of the total injection volume of contrast material with a short injection duration in 64-detector row CT coronary angiography. Br J Radiol. doi:10.1259/bjr/23203690
From AM, Bartholmai BJ, Williams AW et al (2008) Mortality associated with nephropathy after radiographic contrast exposure. Mayo Clin Proc 83:1095–1100
Toprak O (2007) Conflicting and new risk factors for contrast induced nephropathy. J Urol 178:2277–2283
Thomsen HS (2008) Current evidence on prevention and management of contrast-induced nephropathy. Eur Radiol 17(Suppl 6):33–37
Thomsen HS, Morcos SK, Barrett BJ (2008) Contrast-induced nephropathy: the wheel has turned 360 degrees. Acta Radiol 49:646–657
McCullough PA (2008) Contrast-induced acute kidney injury. J Am Coll Cardiol 51:1419–1428
Johnson PT, Pannu HK, Fishman EK (2009) IV contrast infusion for coronary artery CT angiography: literature review and results of a nationwide survey. AJR Am J Roentgenol 192:W214–221
Husmann L, Herzog BA, Burkhard N et al (2009) Body physique and heart rate variability determine the occurrence of stair-step artefacts in 64-slice CT coronary angiography with prospective ECG-triggering. Eur Radiol 19:1698–1703
Aldrovandi A, Maffei E, Palumbo A et al (2009) Prognostic value of computed tomography coronary angiography in patients with suspected coronary artery disease: a 24-month follow-up study. Eur Radiol 19:1653–1660
Lund GK, Wegian E, Saeed M et al (2009) 64-Slice spiral computed tomography of the coronary arteries: dose reduction using an optimized imaging protocol including individual weight-adaptation of voltage and current-time product. Eur Radiol 19:1132–1138
Bae KT, Seeck BA, Hildebolt CF et al (2008) Contrast enhancement in cardiovascular MDCT: effect of body weight, height, body surface area, body mass index, and obesity. AJR 190:777–784
Nakaura T, Awai K, Yauaga Y et al (2008) Contrast injection protocols for coronary computed tomography angiography using a 64-detector scanner: comparison between patient weight-adjusted- and fixed iodine-dose protocols. Invest Radiol 43:512–519
Yamamuro M, Tadamura E, Kanao S et al (2007) Coronary angiography by 64-detector row computed tomography using low dose of contrast material with saline chaser: influence of total injection volume on vessel attenuation. J Comput Assist Tomogr 31:272–280
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hein, P.A., May, J., Rogalla, P. et al. Feasibility of contrast material volume reduction in coronary artery imaging using 320-slice volume CT. Eur Radiol 20, 1337–1343 (2010). https://doi.org/10.1007/s00330-009-1692-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-009-1692-z