Abstract
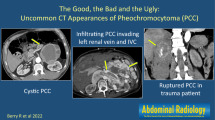
The purpose of this study was to retrospectively evaluate the enhancement washout and other imaging features of pheochromocytomas on delayed contrast-enhanced CT. Twenty-four patients with 31 pathologically confirmed pheochromocytomas were examined using unenhanced, early and delayed contrast-enhanced CT. The range of their APEW (absolute percentage of enhancement washout) or RPEW (relative PEW) values was analyzed. The other CT features including cystic or necrotic change, calcification, and hemorrhage were also determined by a pathologic correlation. Of the 31 pheochromocytomas, 10 (32%) had APEW values of 60% or less and RPEW values of 40% or less. Fourteen (45%) had APEW values >60% and RPEW values >40%. CT showed cystic or necrotic changes in 11 pheochromocytomas (35%) and calcification (10%) in 3. Nineteen pheochromocytomas showed cystic or necrotic changes on early contrast-enhanced CT, but eight of these lesions showed late enhancement on delayed contrast-enhanced CT, which pathologically corresponded to myxoid degeneration. The unenhanced CT showed hemorrhage in 23 pheochromocytomas, but the pathology examinations showed hemorrhage in 15 lesions. Many pheochromocytomas can be misdiagnosed as adenomas on CT due to the high enhancement washout values. Delayed contrast-enhanced CT can detect myxoid degeneration with late enhancement, which is seen as a cystic or necrotic change on early contrast-enhanced CT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pheochromocytomas are rare adrenal medullary tumors arising from chromaffin cells that metabolize and release catecholamines. These tumors are mainly symptomatic, manifesting clinically as hypertension, headache, palpitation, and diaphoresis [1, 2]. Inappropriate or delayed diagnosis of pheochromocytomas may result in hypertensive crisis. However, some pheochromocytomas, up to 4% of all adrenal incidentalomas, do not cause hyperadrenergic symptoms and are detected incidentally on routine abdominal CT [3].
Recently Szolar et al. reported that the absolute and relative washout values of a pheochromocytoma were significantly lower than those of adrenal adenomas and that the sensitivity and specificity for a diagnosis of adenomas were both 100% compared with those for a diagnosis of pheochromocytomas [4]. On the other hand, there are several reports showing that a few pheochromocytomas had such high washout values on delayed contrast-enhanced CT that they mimicked adenomas [5–9]. These studies included a small number of pheochromocytomas and did not adequately evaluate their imaging features of the CT images.
The purpose of this study was to retrospectively evaluate the enhancement washout and other imaging features of pathologically confirmed pheochromocytomas on delayed contrast-enhanced CT.
Materials and methods
The institutional review board approved this retrospective study, and informed consent was waived.
Patients
Between August 2002 and October 2006, this study included 53 patients with 60 adrenal pheochromocytomas, all of which were pathologically confirmed after an adrenalectomy (Fig. 1). The patients consisted of 21 males and 32 females ranging in age from 19 to 77 years (mean age, 48.8 years). Among these patients, 29 were excluded because they had not undergone delayed contrast-enhanced CT, but only abdominal CT (n=28), MRI (n=5), or both (n=4) prior to surgery. The remaining 24 patients (10 men and 14 women aged 19–77 years; mean age, 52 years) with 31 pheochromocytomas underwent multi-phase CT scans including unenhanced, early and delayed contrast-enhanced phases.
Thirty-one pheochromocytomas were between 1.6 and 11.8 cm in size (mean ± standard deviation, 4.4 ± 2.4 cm). The maximum diameter was measured for the lesion size at the axial CT image. Twelve lesions occurred bilaterally in five patients. Of these five patients, four had eight lesions that were clinically diagnosed as multiple endocrine neoplasia (MEN) type IIa and one had four lesions. A single pheochromocytoma was found in 19 patients. Twenty pheochromocytomas arose from the right adrenal gland and 11 arose from the left adrenal gland. Fourteen patients had hyperadrenergic symptoms including one of headache, palpitation, and sweating in addition to hypertension [10]. Ten patients were clinically asymptomatic and their pheochromocytomas were detected incidentally on the abdominal ultrasound or CT that had been performed for other unrelated reasons. However, the biochemical tests in all the patients revealed abnormally elevated catecholamine levels. None of these pheochromocytomas showed any malignant change including metastasis, invasion and abnormal mitosis on both the pathology and follow-up examinations.
CT protocol
The CT examinations were performed with either LightSpeed Qxi (GE Medical Systems; Milwaukee, WI) in 15 patients, LightSpeed Ultra 8 (GE Medical Systems) in 5 patients, LightSpeed ultra 16 in 3 patients, or Brilliance 40 (Philips Medical System, Best, the Netherlands) in 1 patient. The patients underwent unenhanced CT and two-phase contrast-enhanced CT scans. The early and delayed contrast-enhanced CT scans were obtained 1 min and 15 min after administering the contrast material, respectively, which was the same as that reported by Caoili et al. [7].
The imaging parameters for the unenhanced and contrast-enhanced CT scans included 2.5–5 mm collimation, 0.75, 0.875, or 0.926: 1 pitch, 120 kVp and 180–240 mA. The contrast-enhanced CT scans were obtained after an intravenous bolus injection of 120 ml iopromide (Ultravist 370; Schering, Germany) using a power injector at a rate of 3.0 ml/s. The same slice collimation was used to acquire the unenhanced, early and delayed contrast-enhanced CT in the same patient.
Image interpretation
The CT images were reloaded onto the Picture Archiving and Communication System (Centricity, GE Medical System) and were reviewed by B.K.P. and C.K.K., who were experienced in interpretation of cross-sectional imaging for 7 years and 5 years, respectively. These radiologists were unaware of the clinical and pathologic findings, and they interpreted CT images in consensus. First, a round or ovoid region of interest (ROI) was placed in the tumor area showing the strongest enhancement on the image of early contrast-enhanced CT. The ROI was then placed in the same area of the unenhanced and delayed contrast-enhanced CT images. Calcification, blood vessels and necrotic or cystic areas within the lesion were avoided. The CT number of ROI was measured three times and averaged. The absolute and relative percentage of enhancement washout was then calculated in the same manner as the study reported by Caoili et al. [7]. The absolute percentage of enhancement washout (APEW) was defined as follows:
The relative percentage of enhancement washout (RPEW) was defined as follows:
The CT number of pheochromocytomas was finally obtained at each phase of CT scans, and the range of their APEW or RPEW values was analyzed. We determined how many pheochromocytomas satisfied the criteria of an APEW of 60% or less and an RPEW of 40% or less.
The other CT imaging features were evaluated to determine if there were cystic or necrotic changes, calcification, and hemorrhage. Cystic or necrotic changes were defined as a non-enhancing area of water density at the images of both the early and delayed contrast-enhanced CT scans. Calcification was defined as a hyperdense focus, which was apparently similar to the bone on unenhanced CT. Hemorrhage was defined when the lesion had a higher attenuation area on unenhanced CT than the adjacent renal parenchyma. These radiology findings were retrospectively correlated with those of the pathology reports, and representative slides were reviewed if there were discordant features between the radiology and pathology examinations.
Results
Thirty-one pheochromocytomas measured 41 ± 10 HU (range, 19–58 HU) on unenhanced CT, 114 ± 31 HU (range, 66–183 HU) on early contrast-enhanced CT, and 66 ± 11 HU (range, 50–102 HU) on delayed contrast-enhanced CT. None of pheochromocytomas measured 10 HU or less in CT number.
Figure 2 shows the distribution of APEW or RPEW values of the 31 pheochromocytomas. The APEW values of the 31 pheochromocytomas were 62 ± 31% (range, −88–90%) and the RPEW values were 38 ± 22% (range, −55%–68%). Of the 31 pheochromocytomas, 20 (65%) had APEW values >60% with a range of 62–90% (74 ± 8.4%), and 11 (35%) had APEW values 60% or less with a range of −88–59 (39 ± 43%) (Figs. 3 and 4). With the exception of a pheochromocytoma of −88%, ten lesions had an APEW value of 60% or less (52 ± 7.3%, range 39–59%). Fifteen (48%) had RPEW values >40% with a range of (53 ± 8.8%, range 43–68%), and 16 (52%) had RPEW values of 40% or less (25 ± 23%, range −55–39%) (Figs. 3 and 4). With the exception of a pheochromocytoma of −55%, 15 lesions had a RPEW of 40% or less (30 ± 7.8%, range 15–39%).
Percentage of the enhancement washout values of the pheochromocytomas on delayed contrast-enhanced CT. The box plots illustrate the absolute (APEW) and relative (RPEW) percentage of enhancement washout values of the pheochromocytomas. The two outliers (APEW =−88% and RPEW =−55% in case of Fig. 4) are not shown. Fourteen (45%) of the 31 pheochromocytomas have APEW values >60% and RPEW values >40%, mimicking adenoma
A 37-year-old man presented with hypertension and headache. a–c Right adrenal pheochromocytoma (arrow) measured 32 HU, 174 HU, and 55 HU on the unenhanced, early and delayed contrast-enhanced CT images, respectively. The APEW and RPEW values of this tumor are calculated to be 84% and 68%, respectively. The open arrow (b and c) indicates a non-enhancing area on early contrast-enhanced CT, but shows late enhancement on the delayed enhanced CT. d Microscopic examination shows (hematoxyline-eosin staining, ×200) abundant vessels between the tumor nests, apparently related to the rapid enhancement washout on the CT images
A 70-year-old man with an asymptomatic pheochromocytoma. a–b Left adrenal pheochromocytoma (arrow) shows a non-enhancing area on the early contrast-enhanced CT image, but late enhancement of the corresponding area on delayed contrast-enhanced CT image. The tumor has an APEW value of −88% and a RPEW value of −55%. c Microscopic examination (hematoxylin-eosin staining, ×10) shows myxoid degeneration (arrowheads) between the tumor nests without cystic or necrotic changes. In addition, there are many fewer tumor vessels than those shown in Fig. 3, which is apparently related to the low enhancement washout and late enhancement on the delayed enhanced CT. The adrenal cortex is indicated by “C”
Table 1 shows the number of pheochromocytomas at delayed contrast-enhanced CT according to the APEW or RPEW values. Adenoma-like enhancement washout (APEW >60% and RPEW >40%) was observed in 14 (45%) pheochromocytomas, whereas a nonadenoma-like enhancement pattern (APEW 60% and RPEW 40%) was observed in 10 (32%). Figure 3 shows many vessels between the tumor cells, which is related to the high enhancement washout. However, Fig. 4 shows many fewer tumor vessels than Fig. 3. Of the 31 pheochromocytomas, 21 (68%) had an APEW value >60% or a RPEW value >40%.
Nineteen (61%) pheochromocytomas showed non-enhancing areas at early contrast-enhanced CT, but only 11 (35%) of these lesions showed the same cystic or necrotic changes at delayed contrast-enhanced CT (Fig. 5). In 5 of the eleven pheochromocytomas, the non-enhancing areas on the early contrast-enhanced CT had decreased in extent or number on the delayed contrast-enhanced CT (Figs. 3 and 4). The pathology examinations demonstrated the corresponding areas to contain myxoid degeneration between the tumor cells (Fig. 4). The non-enhancing areas of the remaining eight pheochromocytomas showed late enhancement at the delayed contrast-enhanced CT (Figs. 3 and 4). Therefore, cystic or necrotic changes were noted in 35% (11/31) of all the lesions on the CT images, which was equivalent to those on pathologic examination. Eight pheochromocytomas measured <3 cm in the maximum diameter and did not show any cystic or necrotic changes, whereas all lesions (n=6) 5.6 cm or higher except for one had these features. Unenhanced CT showed calcification in three lesions (10%). However, no calcification was noted on pathologic reports because this feature on CT images was located focally and was not detected on the representative pathology slides. The unenhanced CT showed hemorrhage in 23 (74%) of the 31 pheochromocytomas, but the pathologic examinations demonstrated hemorrhage in only 15 tumors: true positive, 13; true negative, 8; false positive, 10 lesions; false negative, 2 lesions.
A 52-year-old man with an asymptomatic pheochromocytoma. a–b Both the early and delayed contrast-enhanced CT images show a lobulating non-enhancing area within the left pheochromocytoma (arrow), indicative of cystic or necrotic changes. c The cut surface of the gross specimen shows a large cystic or necrotic area (asterisk) that correlates well with the CT features
Discussion
Some pheochromocytomas are clinically asymptomatic and thus may be found incidentally on abdomen CT [3, 5, 11]. Up to 10% of patients with pheochromocytomas were reported to be clinically silent [12]. Therefore, an awareness of the CT features of pheochromocytomas is of critical importance in the evaluation or differentiation of adrenal masses. Several studies analyzed the enhancement washout patterns of adrenal masses and demonstrated successful differentiation of adenomas from nonadenomas [7, 13–15]. Szolar et al. reported that pheochromocytomas showed similar washout characteristics to those in adrenal metastasis and had significantly lower enhancement washout than adrenal adenomas [4]. When the adenomas were compared with pheochromocytomas at an optimal cut-off value of 50% APEW and 40% RPEW on contrast-enhanced CT performed 10 min after injecting the contrast material, the sensitivity and specificity for a diagnosis of adenoma were both 100%. The reason for this is the lack of overlap between the APEW and RPEW values of these two adrenal tumors. However, a few pheochromocytomas were reported to show early strong enhancement and rapid contrast material washout, which mimicked adenomas [5–9]. In particular, Park et al. reported that the pheochromocytoma was the most common adenoma-mimicker, which reduced the diagnostic accuracy for adenoma using delayed contrast-enhanced CT [9]. The studies of Blake et al. and Park et al. suggested that these pheochromocytomas with adenoma-like washout profiles have an abundant capillary network within the tumor, leading to avid enhancement on the early contrast-enhanced CT [5, 9]. The mean CT numbers of the pheochromocytomas shown in our study were greater than those of the lipid-poor adenomas reported by Caoili et al. at all phase CT images [7]. In particular, there was a striking difference between the mean CT numbers of pheochromocytomas shown in our study and those of lipid-poor adenomas reported by Caoili et al. at the early contrast-enhanced CT images [7]. The early contrast-enhanced CT in the figures shown by Szolar et al. might be delayed and be scanned in the cortico-medullary phase compared with that shown in our study, which always showed the cortical phase [4]. Kalra et al. reported that the rapid enhancement washout in a pheochromocytoma might be associated with a rich cystoplasmic lipid [8]. However, there were no pheochromocytomas measuring 10 HU or less on the unenhanced CT and containing lipid degeneration on pathology examination as well.
Cystic or necrotic changes tend to occur as pheochromocytomas increase in size. Motta-Ramirez et al. reported these features in 32 (97%) out of 33 pheochromocytomas undergoing CT [10]. However, they performed contrast-enhanced CT only in the portal phase and did not conduct delayed contrast-enhanced CT. In our study, cystic or necrotic changes were observed only in 11 of 19 pheochromocytomas that had non-enhancing areas on early contrast-enhanced CT. Eight pheochromocytomas had pathologically myxoid changes between the tumor cells, resulting in late enhancement on delayed contrast-enhanced CT. Therefore, delayed contrast-enhanced CT should be performed to determine the presence or absence of cystic or necrotic changes in pheochromocytomas. The unenhanced CT sensitivity for a hemorrhage was relatively high, but its specificity was quite low. The CT density of the lesions depends on the level of cellularity, water content, as well as hemorrhage. Therefore, caution should be taken when interpreting the tumor hyperdensity on unenhanced CT images, and MRI might better depict the hemorrhage within the tumor than CT.
Our study had several limitations. First, our study was performed retrospectively, and hence there was some selection bias. A prospective study might be needed to support the data in the future. Second, a pathologic correlation was not completely performed because only photographic pictures of the gross specimens, representative slides for microscopic exams, and pathologic reports were available. For these reasons, the tumor calcifications were not detected on the pathology examinations, but on unenhanced CT even though these features were extremely small in size and number. Third, various CT units were used to evaluate the adrenal pheochromocytomas. However, these CT scanners were under daily quality control, and their image quality was strictly assessed by experienced radiologists.
In conclusion, most pheochromocytomas have high enhancement washout values, which are similar to those of adenomas, and may be misdiagnosed as a nonfunctioning adenoma in clinically asymptomatic cases. Delayed contrast-enhanced CT can detect the myxoid degeneration with late enhancement that is observed as cystic or necrotic changes on early contrast-enhanced CT.
References
Witteles RM, Kaplan EL, Roizen MF (2000) Sensitivity of diagnostic and localization tests for pheochromocytoma in clinical practice. Arch Intern Med 160:2521–2524
Lucon AM, Pereira MA, Mendonca BB, Halpern A, Wajchenbeg BL, Arap S (1997) Pheochromocytoma: study of 50 cases. J Urol 157:1208–1212
Cook DM, Loriaux DL (1996) The incidental adrenal mass. Am J Med 101:88–94
Szolar DH, Korobkin M, Reittner P, Berghold A, Bauernhofer T, Trummer H, Schoellnast H, Preidler KW, Samonigg H (2005) Adrenocortical carcinomas and adrenal pheochromocytomas: mass and enhancement loss evaluation at delayed contrast-enhanced CT. Radiology 234:479–485
Blake MA, Kalra MK, Maher MM, Sahani DV, Sweeney AT, Mueller PR, Hahn PF, Boland GW (2004) Pheochromocytoma: an imaging chameleon. Radiographics 24 Suppl 1:S87–S99
Blake MA, Krishnamoorthy SK, Boland GW, Sweeney AT, Pitman MB, Harisinghani M, Mueller PR, Hahn PF (2003) Low-density pheochromocytoma on CT: a mimicker of adrenal adenoma. AJR Am J Roentgenol 181:1663–1668
Caoili EM, Korobkin M, Francis IR, Cohan RH, Platt JF, Dunnick NR, Raghupathi KI (2002) Adrenal masses: characterization with combined unenhanced and delayed enhanced CT. Radiology 222:629–633
Kalra MK, Blake MA, Boland GW, Hahn PF (2005) CT features of adrenal pheochromocytomas: attenuation value and loss of contrast enhancement. Radiology 236:1112–1113
Park BK, Kim B, Ko K, Jeong SY, Kwon GY (2006) Adrenal masses falsely diagnosed as adenomas on unenhanced and delayed contrast-enhanced computed tomography: pathological correlation. Eur Radiol 16:642–647
Motta-Ramirez GA, Remer EM, Herts BR, Gill IS, Hamrahian AH (2005) Comparison of CT findings in symptomatic and incidentally discovered pheochromocytomas. AJR Am J Roentgenol 185:684–688
Young WF Jr (2007) Clinical practice. The incidentally discovered adrenal mass. N Engl J Med 356:601–610
Bravo EL, Gifford RW Jr (1984) Current concepts. Pheochromocytoma: diagnosis, localization and management. N Engl J Med 311:1298–1303
Szolar DH, Kammerhuber FH (1998) Adrenal adenomas and nonadenomas: assessment of washout at delayed contrast-enhanced CT. Radiology 207:369–375
Pena CS, Boland GW, Hahn PF, Lee MJ, Mueller PR (2000) Characterization of indeterminate (lipid-poor) adrenal masses: use of washout characteristics at contrast-enhanced CT. Radiology 217:798–802
Korobkin M, Brodeur FJ, Francis IR, Quint LE, Dunnick NR, Londy F (1998) CT time-attenuation washout curves of adrenal adenomas and nonadenomas. AJR Am J Roentgenol 170:747–752
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, B.K., Kim, C.K., Kwon, G.Y. et al. Re-evaluation of pheochromocytomas on delayed contrast-enhanced CT: washout enhancement and other imaging features. Eur Radiol 17, 2804–2809 (2007). https://doi.org/10.1007/s00330-007-0695-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-007-0695-x