Abstract
The lower the heart rate the better image quality in multislice computed tomography (MSCT) coronary angiography. We prospectively assessed the influence of heart rate on per-patient diagnostic accuracy and image quality of MSCT coronary angiography and compared adaptive multisegment and standard halfscan reconstruction. A consecutive cohort of 126 patients scheduled to undergo conventional coronary angiography was examined with 16-slice CT. For all heart rate groups, per-patient diagnostic accuracy was significantly higher for multisegment than halfscan reconstruction with values of 95 vs. 79% (p < 0.05, <65 bpm, 38 patients), 85 vs. 66% (p < 0.05, 65–74 bpm, 47 patients), and 78% vs. 41% (p < 0.001, >74 bpm, 41 patients). Differences in diagnostic accuracy between adjacent heart rate groups were only significant for halfscan reconstruction for the comparison between the 65–74 and >74 bpm group (p < 0.05). The vessel lengths free of motion artifacts were significantly longer with multisegment reconstruction in all heart rate groups and for all coronary arteries (p < 0.005). For noninvasive MSCT coronary angiography, both per-patient diagnostic accuracy and image quality decline with increasing heart rate, and multisegment reconstruction at high heart rates yields similar results as standard halfscan reconstruction at low heart rates.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Multislice computed tomography (MSCT) recently emerged as a reliable modality for noninvasive coronary angiography [1–6]. However, as a result of its limited temporal resolution, the quality of MSCT varies with the heart rate, and per-segment and per-vessel diagnostic accuracies are reduced at higher heart rates [7–9]. The relation between the most important level of analysis-per-patient diagnostic accuracy-and heart rate has not been analyzed thus far. Beta blockers are administered to reduce heart rates in 50–100% of the patients enrolled in clinical studies [4, 10–12]. Since beta blockers are contraindicated for instance in patients with moderate to severe asthma it would be an important advance if their use could be reduced or avoided. The results of a small retrospective study suggest that multisegment reconstruction has the potential to dispense with routine beta blocker administration [13]. We prospectively assessed the influence of heart rate on diagnostic accuracy and image quality of MSCT coronary angiography and compared adaptive multisegment and standard halfscan reconstruction of MSCT data sets at different heart rates.
Materials and methods
Population
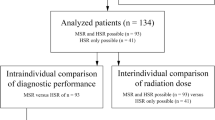
A total of 126 patients with suspected coronary artery disease underwent MSCT and conventional coronary angiography (95 men, 31 women; 64 years ± 8) within 5 days as part of a prospective trial of noninvasive coronary angiography [2]. Inclusion and exclusion criteria as well as further patient characteristics can be found in the main study report [2]. The patients were divided into three heart rate groups according to their average heart rates during MSCT scanning (<65, 65–74, and >74 bpm). These thresholds (65 and 74) were chosen because above 65 bpm beta blocker administration is commonly recommended [4, 14, 15], and at 75 bpm there is synchronous movement of the gantry and the heart (Fig. 1). No beta blockers were given to allow for the normal distribution of heart rates across the standard range. The institutional review board approved the study, and all patients gave written informed consent.
Length of the image acquisition window at a gantry rotation time of 400 ms with standard halfscan reconstruction (dashed line) and multisegment reconstruction (solid line). Please note that the difference in the length of the image acquisition window between both reconstruction approaches increases with the heart rate
CT data acquisition
Scanning was performed on an MSCT scanner with 0.5-mm collimation using 16 simultaneous data channels (Aquilion 16, Toshiba Medical Systems, Japan) with retrospective ECG-gating, 400-ms gantry rotation time, 120 kV, 300 mA, and 0.2 pitch [2]. Sublingual nitroglycerin was given sublingually (5 mg isosorbide dinitrate) to increase the coronary artery diameters and to facilitate image assessment [16].
CT image reconstruction
Images were reconstructed with standard halfscan reconstruction based on data from a 180° gantry rotation (minimum length of the image acquisition window: 200 ms) and with adaptive multisegment reconstruction using segments from up to four consecutive heartbeats (minimal length of the image acquisition window: 50 ms) at 10% intervals throughout the cardiac cycle [13, 17]. The number of segments available for multisegment reconstruction increases with heart rate. With halfscan reconstruction the length of the image reconstruction window remains constant at 200 ms, whereas it has a minimum length of 50 ms with multisegment reconstruction (Fig. 1). There is synchronous movement of the gantry and the heart at certain heart rates (43, 50, 60, 75, and 100 bpm), resulting in a temporal resolution with multisegment reconstruction that is not different from that achieved with standard halfscan reconstruction (Fig. 1). The reconstructed phase during the R-R interval with the least motion for each coronary artery was used for assessment.
Conventional coronary angiography
Conventional coronary angiography was performed after MSCT using standard techniques (Integris 3000, Philips Medical Systems, Best, the Netherlands) with the transfemoral approach. Quantitative coronary angiography was performed using two orthogonal projections to identify significant diameter reductions (at least 50%) in all 15 coronary artery segments [18] by an experienced reader blinded to the results of MSCT. The diameter of the reference vessel on conventional coronary angiography had to measure at least 1.5 mm for a stenosis to be included in the analysis, thus covering all stenoses that might be a target for revascularization.
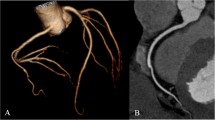
Data and image analysis
The results of conventional coronary angiography served as the reference standard for assessing the diagnostic accuracy and nondiagnostic rate (number of nonassessable studies) of MSCT at different heart rates and using the two reconstruction algorithms in a per-patient analysis. All 15 coronary artery segments according to the classification of the American Heart Association with a diameter of at least 1.5 mm constituted the basis of analysis [18]. If one of the four main coronary arteries contained more than one significant stenosis, the most proximal significant stenosis identified by conventional angiography was used as the anatomic basis for analysis of that vessel [12]. All coronary arteries were analyzed for significant coronary stenoses using axial, coronal, and sagittal images, curved multiplanar reformations, and 3D reconstructions. Images were assessed by one experienced blinded reader unaware of the clinical and conventional angiographic data in a randomized fashion (for the CT reconstruction techniques) using an automatic vessel detection tool (Vitrea 2, Version 3.3, Vital Images, Plymouth, MN) as described [19]. For each data set, overall image quality was rated on a five-point scale (1, nonassessable; 2, poor; 3, moderate; 4, good; 5, very good). The coronary vessel lengths and the vessel lengths free of motion artifacts as a measure of image quality were assessed as described previously [20].
Statistical analysis
All data are expressed as mean ± SD. A contingency analysis with a χ2 or Fisher exact test was used to compare the per-patient diagnostic accuracy, per-patient nondiagnostic rate, and per-vessel nondiagnostic rate of MSCT using 2-by-3 cell matrices as recently described [21, 22]. If at least one coronary artery segment was deemed to be nondiagnostic and there was no coronary stenosis detected in the respective patient, the patient was considered to be nondiagnostic. Thus, patients with only partially adequate coverage of the coronary artery tree and no significant stenosis in any other vessel were considered nondiagnostic (nonassessable image quality) according to the intention-to-diagnose design [23]. The paired and unpaired t test was used to compare the coronary vessel lengths and the image acquisition window for both reconstruction algorithms. Friedman’s test for paired samples and the Kruskal-Wallis-test for unpaired samples were applied to identify differences in overall image quality between the reconstruction algorithms and the heart rate groups, respectively. A p < 0.05 was considered statistically significant. Statistical analysis was performed using SPSS version 12.0 (SPSS Inc., Chicago, IL).
Results
Both MSCT and conventional coronary angiography were successful in all 126 patients. Heart rates were < 65 bpm in 38 patients, 65–74 in 47 patients, and >74 in 41 patients. The average heart rates in these three groups were 57.8 ± 6.4 bpm (range: 35–64), 69.6 ± 3.0 (range: 65–74), and 82.7 ± 6.9 (range: 75–102), respectively. Patient characteristics such as weight, body-mass index, age, and risk factors were not significantly different among the three heart rate groups.
Image quality
The overall image quality of MSCT examinations declined with increasing heart rate, but the differences were significant only for halfscan reconstruction (3.2 ± 1.4 vs. 2.7 ± 1.4 vs. 2.0 ± 1.3, Fig. 2). Multisegment reconstruction yielded significantly (p < 0.001) superior overall image quality compared with halfscan reconstruction in all three heart rate groups, with scores of 3.9 ± 1.1 vs. 3.2 ± 1.4 (<65 bpm), 3.4 ± 1.2 vs. 2.7 ± 1.4 (65–74 bpm), and 3.2 ± 1.3 vs. 2.0 ± 1.3 (>74 bpm, Fig. 2). In no case did the multisegment reconstructions have poorer image quality than the standard halfscan reconstructions. Overall image quality with multisegment reconstruction in the high heart rate group (>74 bpm, 3.2 ± 1.3) was comparable to results obtained with halfscan reconstruction in patients with low heart rates (<65 bpm, 3.2 ± 1.4). This can be explained by the significantly (p < 0.001) shorter image acquisition windows with multisegment reconstruction in all heart rate groups compared with halfscan reconstruction 170 ± 21 ms vs. 200 ms (<65 beats), 137 ± 26 ms vs. 200 ms (65–74 beats), and 132 ± 43 ms vs. 200 ms (>74 bpm). These results are illustrated by representative cases with different heart rates in Figs. 3, 4, and 5.
Comparison of overall image quality of MSCT coronary angiography (from 1= nonassessable to 5= very good) obtained using multisegment and halfscan reconstruction in the three heart rate groups. There was a trend towards reduced overall image quality at higher heart rates with significance only for halfscan reconstruction (p < 0.002). For all three heart rate groups, overall image quality was significantly superior for multisegment reconstruction compared with standard halfscan reconstruction (*p < 0.001). Note that image quality with multisegment reconstruction at high heart rates (>74 bpm) was comparable to results obtained using standard halfscan reconstruction at low heart rates (<65 bpm). Also the difference between both reconstruction approaches increased with the heart rate
Comparison of conventional coronary angiography (a) of the left anterior descending coronary artery (LAD) and left circumflex coronary artery (LCX) with MSCT coronary angiography using multisegment (b) and standard halfscan reconstruction (c) in a 64-year-old female patient with a heart rate of 84 bpm during the scan. Note that at this high heart rate with halfscan reconstruction significant motion artifacts (arrows) even limit the analysis of the left coronary artery system, which is known to exhibit less motion than the right coronary artery [39–42]. The length of the image acquisition window for multisegment and halfscan reconstruction in this patient was 96 and 200 ms, respectively
MSCT coronary angiographies demonstrating absence of stenoses using multisegment (a and c) and halfscan reconstruction (b and d) of the left coronary artery (a and b) and the right coronary artery (RCA, c and d) in a 68-year-old male patient with a heart rate of 64 bpm. At this low heart rate significant motion artifacts are present only along the right coronary artery with halfscan reconstruction (arrows in D) due to a longer image acquisition window (200 vs. 132 ms), while there is motionless depiction of the left coronary artery with both reconstruction approaches
Differences between multisegment (a) and halfscan reconstruction (b) for MSCT coronary imaging can be subtle but relevant as in this 60-year-old female patient with a heart rate of 67 bpm and a pseudostenosis with halfscan reconstruction in the LAD resulting from a motion artifact due to lower temporal resolution (acquisition windows of 118 vs. 200 ms)
In the high heart rate group (>74 bpm) the entire vessel lengths depicted were significantly longer with multisegment reconstruction (Table 1). In contrast, the vessel lengths free of motion artifacts were significantly longer with multisegment reconstruction in all heart rate groups and for all coronary arteries (Table 1).
Diagnostic accuracy
The per-patient diagnostic accuracy of MSCT decreased with increasing heart rate, while the nondiagnostic rate rose with increasing heart rate (Fig. 6). Differences between adjacent heart rate groups were significant for halfscan reconstruction for the comparison of per-patient accuracy between the 65–74 and >74 bpm groups [66% (31/47) vs. 41% (17/41), p < 0.05]. For all three heart rate groups, per-patient diagnostic accuracy was significantly higher for multisegment than halfscan reconstruction with values of 95 vs. 79% (36/38 vs. 30/38, p < 0.05), 85 vs. 66% (40/47 vs. 31/47, p < 0.05), and 78% vs. 41% (32/41 vs. 17/41, p < 0.001, Fig. 6a), respectively. In addition, there was a significantly lower per-patient nondiagnostic rate for multisegment compared with halfscan reconstruction for the three heart rate groups with values of 3 vs. 18% (1/38 vs. 7/38, p < 0.05), 9 vs. 34% (4/47 vs. 16/47, p < 0.01), and 20 vs. 49% (8/41 vs. 20/41, p < 0.01, Fig. 6b), respectively. The diagnostic accuracy and nondiagnostic rate with multisegment reconstruction at high heart rates (above 74 bpm) was comparable to results obtained using standard halfscan reconstruction at low heart rates (below 65 bpm, Fig. 6). Per-vessel nondiagnostic rates with multisegment and halfscan reconstruction for the three heart rate groups are shown in Table 2.
Comparison of per-patient diagnostic accuracy (a) and per-patient nondiagnostic rate (b) of MSCT coronary angiography obtained using multisegment and halfscan reconstruction in the three heart rate groups. There was a trend towards reduced accuracies and elevated nondiagnostic rates at higher heart rates with significance only for halfscan reconstruction in the comparison of accuracy between the 65–74 and above 74 bpm groups (†). For all heart rate ranges, accuracies and nondiagnostic rates were significantly superior for multisegment reconstruction compared with standard halfscan reconstruction (*). Note that the difference in accuracy and nondiagnostic rate between both reconstruction approaches increased with the heart rate
Discussion
Insufficient temporal resolution of MSCT at high heart rates is still one of the major challenges for this emerging noninvasive coronary imaging modality [7–9, 24]. We found a dependency of per-patient accuracy and image quality of 16-slice CT coronary angiography on heart rate, which is in agreement with the observations of previous studies analyzing the per-segment and per-vessel diagnostic accuracies of MSCT using 4 [7, 8] and 16 [9] detector rows. Unlike these studies, we additionally analyzed the heart rate dependency of diagnostic accuracy for the clinically most important and unclustered level of analysis-the patient.
In contrast to the conclusions of our small retrospective study [13], this large prospective intention-to-diagnose analysis shows that the diagnostic performance of CT coronary angiography using multisegment reconstruction is too poor for routine clinical application in patients with high heart rates (>75 bpm). This observation is also in agreement with a recent experimental study demonstrating the negative correlation of image quality and heart rate in a moving heart phantom [25]. In addition to this study, we found both a superior diagnostic accuracy and image quality of multisegment reconstruction over halfscan reconstruction already at low heart rates. This might be due to the superior temporal resolution of multisegment reconstruction also at low heart rates (Fig. 1) and the advantages of the adaptive multisegment reconstruction approach in patients with heart rate variability (which cannot be simulated in phantoms). However, the direct effects of heart rate variability have not been analyzed in this study, but in no case did the adaptive multisegment reconstructions have poorer image quality than the standard halfscan reconstructions. Also Hoffmann et al. have recently found that arrhythmia does not impede diagnostic assessment if adaptive multisegment reconstruction is used [24]. Our study is also in agreement with that of Hamoir et al. in 100 patients who showed a higher number of nonassessable segments (based on image quality) in patients with high heart rates (above 70) using halfscan and nonadaptive bisegmental reconstruction [26]. Grosse et al. [27] recently analyzed image quality in 40 patients undergoing 40-slice CT and have found that all of the 8 patients (20%) with nondiagnostic image quality had heart rates above 70 bpm.
Based on image quality determined in 50 patients, Hoffmann et al. recently suggested that adequate MSCT coronary angiographies can be obtained with adaptive multisegment reconstruction for heart rates of up to 75 bpm [24]. In addition to this study, we also analyzed per-patient diagnostic accuracy. Most importantly, in the present study the segmented approach yielded an accuracy and quality at high heart rates (>75 bpm) that were comparable to the results achieved with the standard approach at low heart rates (<65 bpm). Very recently dual-source CT coronary angiography has been suggested as another option to improve temporal resolution by simultaneously acquiring datasets from two independent gantries [28–31].
The present analysis in a large patient population shows that higher heart rates still reduce the overall image quality of coronary angiography as suggested by the reduction of vessel lengths free of motion artifacts (Table 1) and the relevant per-vessel nondiagnostic rates (Table 2). These data confirm that MSCT results vary with the patient’s heart rate and that it is not possible to dispense with beta blocker administration altogether. However, depending on the clinical question to be answered by MSCT coronary angiography (e.g., simply ruling out stenoses), higher heart rates might be acceptable if segmented reconstruction is used, which yields similar results at higher heart rates as standard halfscan reconstruction in patients with low heart rates. Moreover, multisegment reconstruction may enable successful MSCT coronary imaging also in patients with contraindications to beta blocker administration (e.g., asthmatic patients, intolerance to beta blockers). In the present study 15 of the 88 patients with a heart rate above 65 bpm had moderate to severe asthma that might have been considered a contraindication to beta blocker administration.
Limitations
MSCT with 64 detector rows [5, 6, 15, 32–34] reduces imaging time and therefore also the breathhold time. This has the potential to further improve the diagnostic accuracy of MSCT. Future studies should determine whether the present heart rate dependency of accuracy and quality of current MSCT technology also limits 64-slice scanners, especially those capable of dual-source acquisitions [28–30] since such information is still lacking for this interesting new type of scanner [31]. Heart rate variability during helical acquisition [35] and its effects on different image reconstruction windows [36] was recently analyzed by Leschka et al., but not in our study. Nor did we study cardio-thoracic imaging, which is an interesting combined approach very recently suggested by Salem et al. [37]. The gantry rotation time was not varied in the present study [38] because this feature was unavailable when the study was conducted. No interobserver analysis was performed. The strengths of the present study are the consecutive inclusion of a large number of patients with suspected coronary artery disease all undergoing conventional coronary angiography, the intention-to-diagnose design (inclusion of nondiagnostic segments), and the independent blinded comparison of the CT reconstruction techniques.
In conclusion, our study of the influence of heart rate on 16-slice CT shows that diagnostic accuracy and image quality decrease at increasing heart rate when standard halfscan reconstruction is used, while there is significant improvement with an adaptive segmented reconstruction approach. This multisegment reconstruction technique yields diagnostic and qualitative results at high heart rates (>75 bpm) that are comparable to results obtained using standard halfscan reconstruction at low heart rates (<65 bpm). MSCT coronary angiography may thus be successfully employed to answer certain diagnostic queries in patients with heart rates above 65 bpm and contraindications to beta blockers.
References
Garcia MJ, Lessick J, Hoffmann MH (2006) Accuracy of 16-row multidetector computed tomography for the assessment of coronary artery stenosis. JAMA 296:403–411
Dewey M, Teige F, Schnapauff D, et al (2006) Noninvasive detection of coronary artery stenoses with multislice computed tomography or magnetic resonance imaging. Ann Intern Med 145:407–415
Hoffmann MH, Shi H, Schmitz BL, et al (2005) Noninvasive coronary angiography with multislice computed tomography. JAMA 293:2471–2478
Mollet NR, Cademartiri F, Nieman K, et al (2004) Multislice spiral computed tomography coronary angiography in patients with stable angina pectoris. J Am Coll Cardiol 43:2265–2270
Pugliese F, Mollet NR, Runza G, et al (2006) Diagnostic accuracy of non-invasive 64-slice CT coronary angiography in patients with stable angina pectoris. Eur Radiol 16:575–582
Leschka S, Alkadhi H, Plass A, et al (2005) Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J 26:1482–1487
Nieman K, Rensing BJ, van Geuns RJ, et al (2002) Non-invasive coronary angiography with multislice spiral computed tomography: impact of heart rate. Heart 88:470–474
Giesler T, Baum U, Ropers D, et al (2002) Noninvasive visualization of coronary arteries using contrast-enhanced multidetector CT: influence of heart rate on image quality and stenosis detection. AJR Am J Roentgenol 179:911–916
Cademartiri F, Mollet NR, Runza G, et al (2005) Diagnostic accuracy of multislice computed tomography coronary angiography is improved at low heart rates. Int J Cardiovasc Imaging:1–5
Martuscelli E, Romagnoli A, D’Eliseo A, et al (2004) Accuracy of thin-slice computed tomography in the detection of coronary stenoses. Eur Heart J 25:1043–1048
Ropers D, Baum U, Pohle K, et al (2003) Detection of coronary artery stenoses with thin-slice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation 107:664–666
Nieman K, Cademartiri F, Lemos PA, Raaijmakers R, Pattynama PM, de Feyter PJ (2002) Reliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation 106:2051–2054
Dewey M, Laule M, Krug L, et al (2004) Multisegment and halfscan reconstruction of 16-slice computed tomography for detection of coronary artery stenoses. Invest Radiol 39:223–229
Hoffmann U, Moselewski F, Cury RC, et al (2004) Predictive value of 16-slice multidetector spiral computed tomography to detect significant obstructive coronary artery disease in patients at high risk for coronary artery disease: patient-versus segment-based analysis. Circulation 110:2638–2643
Raff GL, Gallagher MJ, O’Neill WW, Goldstein JA (2005) Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol 46:552–557
Dewey M, Hoffmann H, Hamm B (2006) Multislice CT coronary angiography: effect of sublingual nitroglycerine on the diameter of coronary arteries. Fortschr Röntgenstr 178:600–604
Dewey M, Müller M, Teige F, et al (2006) Multisegment and halfscan reconstruction of 16-slice computed tomography for assessment of regional and global left ventricular myocardial function. Invest Radiol 41:400–409
Austen WG, Edwards JE, Frye RL, et al (1975) A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 51:5–40
Dewey M, Rutsch W, Schnapauff D, Teige F, Hamm B (2007) Coronary artery stenosis quantification with multislice computed tomography. Invest Radiol 42:78–84
Achenbach S, Giesler T, Ropers D, et al (2003) Comparison of image quality in contrast-enhanced coronary-artery visualization by electron beam tomography and retrospectively electrocardiogram-gated multislice spiral computed tomography. Invest Radiol 38:119–128
Simel DL, Feussner JR, DeLong ER, Matchar DB (1987) Intermediate, indeterminate, and uninterpretable diagnostic test results. Med Decis Mak 7:107–114
Begg CB, Greenes RA, Iglewicz B (1986) The influence of uninterpretability on the assessment of diagnostic tests. J Chronic Dis 39:575–584
Knottnerus JA, Muris JW (2003) Assessment of the accuracy of diagnostic tests: the cross-sectional study. J Clin Epidemiol 56:1118–1128
Hoffmann MH, Shi H, Manzke R, et al (2005) Noninvasive coronary angiography with 16-detector row CT: effect of heart rate. Radiology 234:86–97
Greuter MJ, Dorgelo J, Tukker WG, Oudkerk M (2005) Study on motion artifacts in coronary arteries with an anthropomorphic moving heart phantom on an ECG-gated multidetector computed tomography unit. Eur Radiol 15:995–1007
Hamoir XL, Flohr T, Hamoir V, et al (2005) Coronary arteries: assessment of image quality and optimal reconstruction window in retrospective ECG-gated multislice CT at 375-ms gantry rotation time. Eur Radiol 15:296–304
Grosse C, Globits S, Hergan K (2007) Forty-slice spiral computed tomography of the coronary arteries: assessment of image quality and diagnostic accuracy in a non-selected patient population. Acta Radiol 48:36–44
Johnson TR, Nikolaou K, Wintersperger BJ, et al (2006) Dual-source CT cardiac imaging: initial experience. Eur Radiol 16:1409–1415
Flohr TG, McCollough CH, Bruder H, et al (2006) First performance evaluation of a dual-source CT (DSCT) system. Eur Radiol 16:256–268
Achenbach S, Ropers D, Kuettner A, et al (2006) Contrast-enhanced coronary artery visualization by dual-source computed tomography-initial experience. Eur J Radiol 57:331–335
Scheffel H, Alkadhi H, Plass A, et al (2006) Accuracy of dual-source CT coronary angiography: first experience in a high pre-test probability population without heart rate control. Eur Radiol 16(12):2739–2747
Leber AW, Knez A, von Ziegler F, et al (2005) Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol 46:147–154
Mollet NR, Cademartiri F, van Mieghem CA, et al (2005) High-resolution spiral computed tomography coronary angiography in patients referred for diagnostic conventional coronary angiography. Circulation 112:2318–2323
Ropers D, Rixe J, Anders K, et al (2006) Usefulness of multidetector row spiral computed tomography with 64- × 0.6-mm collimation and 330-ms rotation for the noninvasive detection of significant coronary artery stenoses. Am J Cardiol 97:343–348
Leschka S, Wildermuth S, Boehm T, et al (2006) Noninvasive coronary angiography with 64-section CT: Effect of average heart rate and heart rate variability on image quality. Radiology 241:378–385
Leschka S, Husmann L, Desbiolles LM, et al (2006) Optimal image reconstruction intervals for non-invasive coronary angiography with 64-slice CT. Eur Radiol 16(9):1964–1972
Salem R, Remy-Jardin M, Delhaye D, et al. (2006) Integrated cardio-thoracic imaging with ECG-Gated 64-slice multidetector-row CT: initial findings in 133 patients. Eur Radiol 16:1973–1981
Greuter MJ, Flohr T, van Ooijen PM, Oudkerk M (2007) A model for temporal resolution of multidetector computed tomography of coronary arteries in relation to rotation time, heart rate and reconstruction algorithm. Eur Radiol 17(3):784–812
Achenbach S, Ropers D, Holle J, Muschiol G, Daniel WG, Moshage W (2000) In-plane coronary arterial motion velocity: measurement with electron-beam CT. Radiology 216:457–463
He S, Dai R, Chen Y, Bai H (2001) Optimal electrocardiographically triggered phase for reducing motion artifact at electron-beam CT in the coronary artery. Acad Radiol 8:48–56
Mao S, Lu B, Oudiz RJ, Bakhsheshi H, Liu SC, Budoff MJ (2000) Coronary artery motion in electron beam tomography. J Comput Assist Tomogr 24:253–258
Wang Y, Vidan E, Bergman GW (1999) Cardiac motion of coronary arteries: variability in the rest period and implications for coronary MR angiography. Radiology 213:751–758
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dewey, M., Teige, F., Laule, M. et al. Influence of heart rate on diagnostic accuracy and image quality of 16-slice CT coronary angiography: comparison of multisegment and halfscan reconstruction approaches. Eur Radiol 17, 2829–2837 (2007). https://doi.org/10.1007/s00330-007-0685-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-007-0685-z