Abstract
Acute testicular torsion in children is an emergency and has to be diagnosed urgently. D oppler sonography is increasingly used in imaging the acute scrotum. Nevertheless, in uncertain cases, surgical exploration is required. In this study, we attempted to define the role of Doppler sonography in the diagnostic workup of the acutely painful scrotum. All patients admitted between 1999 and 2005 with acute scrotal pain were included. After clinical assessment, patients were imaged by Doppler sonography with a ‘‘high-end’’ instrument. In cases of absent arterial perfusion of the testis in Doppler sonography, surgical exploration was carried out. Patients with unaffected perfusion were followed clinically by ultrasound for up to 2 years. Sixty-one infants and children aged 1 day to 17 years (median: 7.9 years) were included. In 14 cases, sonography demonstrated absent central perfusion, with abnormal parenchymal echogenicity in six. Absence of venous blood flow together with reduction of central arterial perfusion was found in one infant. In these 15 patients, surgical exploration confirmed testicular torsion. Among the other 46 patients, we found four cases with increased testicular perfusion and 27 with increased perfusion of the epididymis. In one infant, a testicular tumour was found sonographically, and orchiectomy confirmed diagnosis of a teratoma. Follow-up examinations of the conservatively treated patients showed good clinical outcome with physiologic central perfusion as well as normal echogenic pattern of both testes. No case of testicular torsion was missed. By means of Doppler sonography, an unequivocal statement regarding testicular perfusion was possible in all cases. The initial Doppler diagnosis was confirmed by operative evaluation and follow-up ultrasound. Testicular torsion can therefore be excluded by correctly performed ultrasound with modern equipment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute testicular torsion in children is an emergency [1]. At first glance, the triggering reason for scrotal swelling, reddening and pain is not obvious. Besides testicular torsion, torsion of the appendages of the testis, inflammatory diseases or further underlying causes such as Schoenlein-Henoch purpura can be responsible for acute scrotal pain [2–4]. About 1:4,000 boys is affected, and two age groups (infants and juveniles) are most likely to be affected [5]. Testicular torsion is defined as a rotation of the longitudinal axis of the spermatic cord, resulting in strangulation of testicular blood flow. Because of the occurrence of irreversible parenchymal damage after 6 h of ischaemia [1, 6], testicular torsion should be differentiated from other acute scrotal diseases.
In addition to careful clinical evaluation, Doppler sonography is increasingly used in the management of patients with suspicion for testicular torsion [4, 7–14]. This can mainly be attributed to the quick technical progress with excellent anatomical imaging and simultaneous portrayal of blood flow [8, 10]. High-frequency transducers, power Doppler and tissue-harmonic functions are increasingly used in daily routine care. However, to prove testicular torsion, surgical exploration of the scrotum is still fairly often performed. Taken into consideration that less than 30% of infants with an acute scrotum suffer from testicular torsion [11], it is obvious that most infants may be managed conservatively. Therefore, accurate indication for surgery aims to avoid unnecessary exploration without missing torsion that may potentially lead to dangerous consequences. This prompted us to determine the reliability of Doppler sonography in the diagnostic workup of the acutely painful scrotum.
Materials and methods
All patients admitted between 1999 and 2005 with acute scrotal pain were included. After clinical assessment, a Doppler sonographic examination with a ‘‘high-end’’ instrument (Sonoline Elegra/Siemens) was performed. Sonography was done by a highly experienced paediatric radiologist in urosonography according to the following examining pattern whereby a side comparison was undertaken.
-
1.
Determination of sonomorphology of the scrotum and epididymis, including echogenicity and echotexture
-
2.
Testicle volume
-
3.
Central and peripheral perfusion of the testicle via power and colour Doppler sonography
-
4.
Central arterial and venous flow curve in the testicle using the triplex mode
A 7.5 MHz linear array transducer (7.5 l40/Siemens) with a frequency of 7.5–9 MHz was used for examination. Speed scale of the colour Doppler setting was put at the lowest detectable flow speed (low flow, low PRF). Therefore, a low filter setting was important. This allowed detection of flow speeds below 3 cm/s. Measurement of serum electrolytes and C-reactive protein and a full blood count completed the assessments. If Doppler investigation documented a lack or reduction of central arterial perfusion without an identification of a diastolic flow, the organ was explored surgically (Fig. 1). Patients with intact central perfusion (Fig. 2) had clinical and ultrasound follow-up up to 2 years after initial presentation. Conservative treatment included local antiphlogistic measures. In cases of increased perfusion of testicular parenchyma or epididymis, antibiotic therapy was performed.
Additionally, all cases of acute scrotum were evaluated retrospectively (1985–1994) for determination of the frequency of testicular torsion. Within this period, surgical exploration in suspicion for testicular torsion was routinely performed.
Results
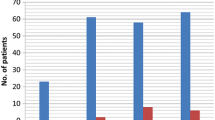
Sixty-one infants and children aged 1 day to 17 years (median: 7.9 years) were included (Fig. 3). Four patients were neonates. All infants presented with acute scrotal swelling, reddening and pain. In all cases, clinical evaluation led to suspicion on testicular torsion.
Surgical exploration
Fifteen infants were operated due to suspicion for testicular torsion and 13 for other reasons. In 14 cases, sonography demonstrated absent central venous and arterial perfusion. In one patient, venous blood flow was absent and central arterial perfusion of the testis was reduced (no diastolic flow and hypoperfusion at power Doppler sonography). Six of these testes presented inhomogeneous echogenic parenchyma. Surgical exploration confirmed testicular torsion in all 15 patients. Surgery was performed at an average of about 6 h after the onset of symptomatic pain. Neonates are not included in this estimate. Intravaginal torsion was found in eight (one neonate) 2–14 years (mean age: 6.8 years) and supravaginal torsion in seven (3 neonates) 1–17 years (mean age: 7.1 years). In four cases, testes had to be removed because of necrosis. In 11 cases, we performed detorsion and a two-point fixation by suture. Contralateral orchidopexy was performed 4–6 weeks after the first operation. In one infant (7 months), a testicular tumour was found sonographically, and histologic analysis following orchiectomy confirmed diagnosis of a teratoma. Twelve boys with integral central testicular perfusion in the initial workup had persistent intense pain for up to 2 days. Torsion of the hydatid was suggested in preoperative ultrasound in eight of these infants. Testicular torsion was not found in any of them. In 11 cases, a torsion of the hydatid was removed, and in one case only, hyperaemia and swelling of the testis and epididymis was noted, as shown by preoperative sonography.
Conservative therapy
Among the 33 nonoperated patients, one case with increased testicular perfusion and 19 with increased perfusion of the epididymis were detected (Fig. 4). Laboratory assessments showed an increase in leukocyte count in nine cases and an increase in C-reactive protein in four, without correlation to testicular perfusion. One of these patients showed obvious signs of a Schoenlein-Henoch purpura. During the period, only one patient had to be excluded because of restlessness while examination. In four patients with initial uncomplicated hospital stay and clinical course, follow-up examination was not possible. In all other cases, normal central perfusion as well as normal echogenic pattern and size of both testes were documented during follow-up examinations. In sonography after surgical detorsion, we found adequate reperfusion in ten cases in the initial stage. Three testes showed signs of atrophy, with scars of testicular parenchyma over time. History of these patients showed an onset of pain 4, 7 and 24 h before reduction. Another patient (3 weeks old) with a reduction at approximately 10 h after the onset of symptoms showed normal morphology and testicular perfusion at 6 months of age. When compared with the unaffected side, the difference in testicular volume was +110% (mean: + 126% SD) in cases with surgically reduced torsion and + 15% (mean: +30% SD) in the group without torsion.
Altogether sonographic examination resulted in a decisive statement about testicular perfusion in all cases, and was, as a consequence followed by adequate treatment. The use of Doppler sonography for detecting testicular torsion resulted in the correct diagnosis in all patients, with a sensitivity, specificity and positive as well as negative predictive value of 100% (15/15, 46/46, 15/15, 46/46, respectively). By retrospective evaluation from 1985 to 1994, 75 cases of acute scrotum with an average of 6.3 years of age were identified. In all patients, testes were explored surgically without preoperative sonographic evaluation (Table 1). Testicular torsion was found in 25 cases only (33 %).
Discussion
In the last few years, ultrasound has become the most important examination device in all types of paediatric scrotal pathology [9–18]. This is mainly due to the excellent imaging of anatomic details and perfusion as well as the advantage of real-time examination. Because of the prompt availability, low costs, short duration (<30 min) and convenience of this examining method when compared with alternative diagnostic tools such as magnetic resonance imaging (MRI) or scintigraphy, sonography has become the standard examination device in the acute scrotum [19, 20]. Despite reports on strongly varying results concerning the reliability for detecting testicular torsion by Doppler sonography [1, 17, 21], recent studies show an increasing sensitivity of this method [11, 12, 14, 22]. Nevertheless, surgical exploration is still mandatory in uncertain cases. The aim of our study was to determine the accuracy of ultrasonographic assessment of the acute scrotum in infants in a recent time span (1999–2005).
In 61 cases, Doppler sonography resulted in an unequivocal statement regarding testicular perfusion. Therapy was performed on the basis of sonographic findings. Suspicion on testicular torsion via impaired blood flow was revealed preoperatively in all 15 cases of surgically confirmed testicular torsion. In the remaining cases with positive perfusion of the testicle, adequate therapy could be achieved by supportive therapy or surgery if indicated as for removal of a tumour or a painful torched appendix testis. The present study thus confirms the reliability and underlies the importance of sonography in the diagnostic workup of the acute scrotum in infancy.
Due to age-related incidence and diagnostic difficulties, a separating patients into neonates and others was proposed [23]. Our results, however, indicate that an evaluation of testicular perfusion can be achieved with a sensitivity and specificity of 100% independent of the infant’s age. According to van der Sluijs, sonography may even serve to identify prenatal torsion [24]. Especially important, therefore, is differentiation to the neonatal neoplasia [25]. Due to difficulties in clinical assessment and differentiation between neoplasm and torsion of the testicle, we recommend urgent surgical exploration in the absence of central testicular perfusion in neonates.
Volumetry was not helpful in differential diagnosis of the acute scrotum. Considering the large variability of testicular size, volumes ranged from normal until elevated in either underlying pathology. Laboratory parameters did not correlate to any cause of the disease.
As well as excluding the absence of perfusion, sonography was useful in further aetiological differentiation of diseases. Differentiation between epididymitis and torsion of the testis appendix via sonography can be inconclusive since an existing hydatid cannot always be seen (Fig. 5). In nine of 11 infants with excision of the hydatid, only hyperperfusion was found in sonography. However, if hyperperfusion of the epididymis is found, sonographic examination of the entire urinary tract to exclude structural anomalies is recommended. Surgical exploration of the testis in persistent pain with intact perfusion is controversial. We believe that for suspicion of hydatid torsion, surgical exploration can be justified since hydatid excision may potentially reduce ongoing inflammation and pain.
Moreover ultrasonography was helpful in evaluating he recovery of the testis after reduction. In one remarkable case, reperfusion was documented following a duration of about 10 h, clearly longer than the 6 h after which ischaemic damage is believed to be irreversible. As intraoperatively the degree of irreversibility of tissue damage cannot be judged conclusively, we recommend extraction of the testis only in strongly evident destruction, but otherwise we recommend detorsion and sonographic follow-up evaluation.
The present data suggest that obligatory emergency scrotal exploration was not necessary in more than 75% of cases presenting for acute scrotum. This was also confirmed by retrospective evaluation. The diagnostic benefit of routine surgical evaluation is small in relation to the risk-taking of aspiration and wound infection. Nonetheless, acute testicular torsion is an emergency requiring immediate diagnostic intervention when suspected. In all cases, torsion was revealed sonographically. We believe that diagnostic ultrasound, if performed correctly (central arterial and, if possible, venous perfusion signal during tranquil examining conditions) and with modern equipment, may reliably be used to exclude testicular torsion in infants and children. Last but not least, total costs may be reduced by replacing scrotal exploration with a less extensive evaluation method (2,300 euro vs 1,300 euro, respectively, according to the German diagnosis-related group’s catalogue).
For consistent and comparable results, documentation should always include description of echogenicity and tissue structure of testis and epididymis of both sides, scrotum volumetry in side comparison and assessment of central and peripheral blood flow of the testicles at power and colour Doppler sonography, including documentation of the central arterial and venous flow curve at the triplex mode. In case of given perfusion, the resistance index (RI) should be included to recognise possible partial torsion (180°) [25]. At 0.6–0.7, the RI in the infantile testicle is usually rather low [11, 25]. In an inflammatory process, RI even declines, and at a partial torsion, higher counts are to be expected [11, 25]. Special attention has to be paid to the fact that spontaneous reduction in intermittent torsion can appear as reactive hyperfusion of the testicular parenchyma. Additionally, one should take into consideration that, in case of testicular torsion with absent central blood flow, peripheral perfusion can be maintained via collateral arterial supply. Preoperative sonographically controlled reduction might be beneficial until emergency surgery [26] but there is little experience with this proceeding so far.
In our study, central arterial perfusion was a reliable diagnostic parameter to exclude testicular torsion. To be sure not to fail to notice a partial torsion, sonographic identification of central venous perfusion should be reached. We conclude that Doppler sonography, if performed correctly with modern equipment as a standard procedure, may replace surgical exploration in case of suspected testicular torsion. In case of doubt, surgical exploration is still indicated.
References
Dunne PJ, O’Loughlin BS (2000) Testicular torsion: time is the enemy. ANZ J Surg 70:441–442
Somekh E, Gorenstein A, Serour F (2004) Acute epididymitis in boys: evidence of post-infectious etiology. J Urol 171:391–394
Ben-Sira L, Laor T (2000) Severe scrotal pain in boys with Henoch-Schonlein purpura: incidence and sonography. Pediatr Radiol 30:125–128
Ciftci AO, Senocak ME, Cahit Tanyel F, Buyukpamukcu N (2004) Clinical Predictors for Differential Diagnosis of Acute Scrotum. Eur J Pediatr Surg 14:333–338
McAndrew HF, Pemberton R, Kikiros CS, Gollow I (2002) The incidence and investigation of acute scrotal problems in children. Pediatr Surg Int 18:435–437
Frush DP, Babcock DS, Lewis AG, Paltiel HJ, Rupich R, Bove KE, Sheldon CA (1995) Comparison of color Doppler sonography and radionuclide imaging in different degrees of torsion in rabbit testes. Acad Radiol 2:945–951
Corbett HJ, Simpson ET (2002) Management of the acute scrotum in children. ANZ J Surg 72:226–228
Hormann M, Balassy C, Philipp MO, Pumberger W (2004) Imaging of the acute scrotum in children. Eur Radiol 14:974–983
Kadish HA, Bolte RG (1998) A retrospective review of pediatric patients with epididymitis, testicular torsion and torsion of testicular appendages. Pediatrics 102:73–76
Pavlica P, Barozzi L (2001) Imaging of the acute scrotum. Eur Radiol 11:220–228
Stehr M, Boehm R (2003) Critical Validation of Colour Doppler Ultrasound in Diagnostics of Acute Scrotum in Children. Eur J Pediatr Surg 13:386–392
Weber DM, Rosslein R, Fliegel C (2000) Color Doppler sonography in the diagnosis of acute scrotum in boys. Eur J Pediatr Surg 10:235–241
Aso C, Enriquez G, Fite M, Toran N, Piro C, Piqueras J, Lucaya J (2005) Gray-scale and color Doppler sonography of scrotal disorders in children : an update. Radiographics 25:1197–1214
Baker LA, Sigman D, Mathews RI, Benson J, Docimo SG (2000) An analysis of clinical outcomes using color Doppler testicular ultrasound for testicular torsion. Pediatrics 105:604–607
Dubinsky TJ, Chen P, Maklad N (1998) Color-flow and power Doppler imaging of the testes. World J Ur 16:35–40
Farriol VG, Comella XP, Agromayor EG, Creixams XS, Martinez De La Torre IB (2000) Gray-scale and power Doppler sonographic appearances of acute inflammatory diseases of the scrotum. J Clin Ultrasound 28:67–72
Yazbeck S, Patriquin HB (1994) Accurancy of Doppler sonography in the evaluation of acute conditions of the scrotum in children. J Pediatr Surg 29:1270–1272
Frush DP, Sheldon CA (1998) Diagnostic imaging for pediatric scrotal disorders. Radiographics 18:969–985
Nussbaum Blask AR, Bulas D, Shalaby-Rana E, Rushton G, Shao C, Majd M (2002) Color Doppler sonography and scintigraphy of the testis: a prospective, comparative analysis in children with acute scrotal pain. Pediatr Emerg Care 18:67–71
Trambert MA, Mattrey RF, Levine D, Bethoty DP (1990) subacute scrotal pain: evaluation of torsion versus epididymitis with MR imaging. Radiology 175:53–56
Zoller G, Kugler A, Ringert RH (2000) ‘‘False positive’’ testicular perfusion in testicular torsion in power Doppler ultrasound. Urologe A 39:251–253
Kravchick S, Cytron S, Leibovici O, Linov L, London D, Altshuler A, Yulish E (2001) Color Doppler sonography: its real role in the evaluation of children with highly suspected testicular torsion. Eur Radiol 11:1000–1005
Pinto KJ, Noe HN, Jerkins GR (1997) Management of neonatal testicular torsion. J Urol 158:1196–1197
van der Sluijs JW, den Hollander JC, Lequin MH, Nijman RM, Robben SG (2004) Prenatal testicular torsion: diagnosis and natural course. An ultrasonographic study. Eur Radiol 14:250–255
Jee WH, Choe BY, Byun JY, Shinn KS, Hwang TK (1997) Resistive index of the intrascrotal atery in scrotal inflammatory disease. Acta Radiol 38:1026–1030
Garel, L, Dubois J, Azzie G, Filiatrault D, Grignon A, Yazebeck S (2000) Preoperative manual detorsion of the spermatic cord with Doppler ultrasound monitoring in patients with intravaginal acute testicular torsion. Pediatr Radiol 30:41–44
Author information
Authors and Affiliations
Corresponding author
Additional information
Patrick Gunther and Jens-Peter Schenk contributed equally to this work
Rights and permissions
About this article
Cite this article
Gunther, P., Schenk, J., Wunsch, R. et al. Acute testicular torsion in children: the role of sonography in the diagnostic workup. Eur Radiol 16, 2527–2532 (2006). https://doi.org/10.1007/s00330-006-0287-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0287-1