Abstract
The aim of this study was to demonstrate the ultrasonographic features of prenatal torsion of the testis at presentation and during follow-up, with histological correlation post-orchidectomy. Between January 1985 and December 1999, 13 neonates with antenatal torsion of the testis were examined postnatally, at presentation and during follow-up, with high-resolution ultrasonography, including colour Doppler ultrasonography. Bilateral testis volume was evaluated [length×width×depth×(π/6)]. Ultrasonographic findings were correlated with histological findings (n=8) and findings at surgery. Moreover, in 1 patient the affected testis was postoperatively examined with ultrasonography in vitro. These findings were correlated with preoperative ultrasonography and corresponding histological slices. All patients (n=13) presented with a painless congenital scrotal mass. On the affected side no flow was found with colour Doppler ultrasonography. Testis volume on the affected and normal side showed mean values of 2.1 and 0.5 cc, respectively. On ultrasonography all patients showed scrotal swelling and a heterogeneous testis with hypoechoic central areas (necrosis). The tunica albuginea was thickened in all patients, with focal (n=2) or rim-like (n=11) hyperechoic reflections (calcifications) at the transitional zone between testis and tunica albuginea. In 9 patients follow-up ultrasonography showed progressive testis atrophy on the affected side. In 10 patients a contralateral hydrocele was found. Prenatal torsion shows a characteristic ultrasonographic pattern. In newborns with a scrotal mass, these ultrasonographic findings should suggest this diagnosis and delay in immediate surgery and/or oncological work-up may be appropriate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Differential diagnostic possibilities in a newborn with a painless congenital scrotal swelling and a palpable mass include testicular torsion, benign and malignant tumours of the testis and epididymis, inguinal hernia with or without incarceration, hydrocele, haematocele, torsion of the appendix of the testis or epididymis, epididymo-orchitis, idiopathic infarction of the testis, meconium peritonitis, ectopic splenic or adrenal rests [1, 2, 3, 4]. The principal argument to support early surgical intervention is that it enables one to confirm the diagnosis and differentiate a prenatal torsion from testicular tumour or incarcerated inguinal hernia [1, 5]. The major problem with this approach is that operative intervention and, in particular, risks from general anaesthesia, are significant in the newborn [5].
Ultrasonography with colour Doppler enhancement is proposed as imaging modality of choice in the assessment of a scrotal mass for identifying neonates with prenatal testis torsion and in excluding other scrotal pathological conditions [5, 6]; however, there are no reports on the ultrasonographic features of the testicle during follow-up after torsion. We present a series of 13 newborns who presented with a scrotal swelling and a palpable mass. The purpose of this study was twofold: firstly, to determine the ultrasonographic features of prenatal testicular torsion at presentation and during follow-up; and secondly, to correlate these ultrasonographic characteristics with histological findings.
Materials and methods
Between January 1985 and December 1999, 13 neonates with prenatal torsion of the testis were examined with ultrasonography. They were all full-time newborns with unilateral disease, except for one who had bilateral torsion. Ten patients presented in the first 3 days of life, and 3 patients presented at 7, 22 and 27 days of age, respectively. Patients older than 1 month were excluded from this study.
In this retrospective study for the ultrasonographic studies 7- to 10-MHz (Ultramark 9 HDI, Advanced Technology Laboratories, Bothell, Wash.) and 7-MHz (model 128 XP10; Acuson, Mountain View, Calif.) linear-array transducers were used. In the ultrasonographic study (a) colour Doppler ultrasonography was used for testicular flow determination, (b) testis volume was evaluated on both sides using the formula of an ellipsoid [length×width×depth×(π/6)], and (c) transverse and sagittal ultrasonographic images of both testicles were obtained for evaluation of testicular anatomy and texture.
The diagnosis was confirmed by surgery and subsequent histology (n=8), surgical exploration without orchidectomy (n=3), and clinical and ultrasonographic follow-up (n=2).
None of the patients underwent immediate surgery; therefore, it was possible to examine 10 affected testicles in 9 patients with ultrasonography during follow-up. During follow-up the testicular volume was measured and the changes of the parenchyma over time were recorded.
An in vitro study was performed using one testicle: the affected testicle was examined with ultrasonography at the first day of age, day 11, day 38 and at day 73 prior to surgery and immediately after surgery being submerged in a saline solution. The same technique and equipment as in the in vivo study was used. Subsequently, the testicle was fixed in formalin and embedded in paraffin for histological examination. The histological slices were compared with the corresponding ultrasonographic images.
Results
All patients with prenatal torsion of the testis presented with a painless congenital scrotal swelling and a palpable mass. The mass was left sided in 4 patients, right sided in 8 and bilateral in 1 patient. Colour Doppler ultrasonography demonstrated flow in the contralateral normal testicles in all infants with unilateral disease, whereas no testicular flow could be depicted on the affected side in all 13 patients.
The mean volume of the affected testis and contralateral normal testicle was 2.1 ml (range 0.7–4.6 ml) and 0.5 ml (range 0.2–0.7 ml), respectively. The difference was statistically significant (p=0.001, paired t test). At presentation in all 13 newborns, on ultrasonography the affected testicles showed a heterogeneous pattern with hypoechoic areas; however, immediately around the testis a thickened layer was seen, assumed to be a thickened tunica albuginea, which showed partially hypoechoic and partially hyperechoic, often even rim-like alterations. At the transitional zone between thickened tunica albuginea and affected testis parenchyma also sharply demarcated hyperechoic reflections were seen focally (n=2) and mostly even rim-like (n=11; Figs. 1, 2a). No calcifications or cysts were found in the testis parenchyma and the epididymis was not separately recognizable. In all patients with unilateral disease the contralateral hemiscrotum demonstrated a normal testis with homogeneous parenchyma and testicular flow, slight collateral swelling of the scrotal wall and a recognizable epididymis. In 10 patients a hydrocele was found on this side.
The first day after delivery, an ultrasonographic image of the left testicle shows a heterogeneous pattern consisting of a hyperechoic rim-like layer (long arrows) surrounding a centre of decreased inhomogeneous echogenicity assumed to be necrotic testicular tissue. Note the hyperechoic reflections (short arrows) at the border of the rim-like layer and the centre
Ultrasonographic images of the right testicle. All images are comparable with regard to magnification factor. a At birth, volume was 2.4 cc. Note heterogeneous pattern of testis parenchyma, although some rim-like structures can already be detected (arrows). b Ultrasonography after 26 days, volume 0.4 cc. Development of a hyperechoic rim at the transitional zone between tunica albuginea and affected testis (arrows). c Ultrasonography after 54 days, volume 0.1 cc. Progressive volume loss, and the hyperechoic rim persists
In 9 patients follow-up ultrasonography was done to evaluate testicular alterations in time. Mean number of studies was 3.7, with a mean follow-up of 75.2 days and time ranging between ultrasonographic controls of 3–85 days. All these patients showed progressive atrophy of the affected testis. Moreover, in time the testis became more hyperechoic and more homogeneous. We also noticed gradual progression of the hyperechoic reflections to a more rim-like configuration at the transitional zone between tunica albuginea and the affected testis (Fig. 2).
Testis wasting and volume half-time is shown in Fig. 3. Volume half-time ranged between 8 and 65 days and there was a mean volume half-time of 28.5 days for these 9 patients, including the one with bilateral torsion of the testis.
In 8 patients orchidectomy was performed between 3 weeks and 11 months (mean 4.4 months) after birth. In all these patients a preoperative ultrasonographic study was performed within 3 weeks of operation. In 1 patient with bilateral torsion of the testis, the left testis was left in situ, because some colour improvement after detorsion suggested a viable testis. Subsequent ultrasonography, however, showed progressive testis atrophy.
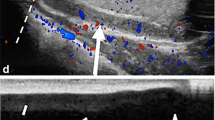
The in vitro ultrasonographic study of an affected testis shows heterogeneous testis parenchyma surrounded by a hyperechoic rim at the transitional zone between testis and the thickened overlying tunica albuginea (Fig. 4).
In vitro study of an atrophied testicle after prenatal torsion, at the age of 4 months. a, b Thickened tunica albuginea (small arrows) and hyperechoic rim, calcifications between tunica albuginea and necrotic testis (long arrow) are clearly visible. a Ultrasonographic image prior to orchidectomy (same as Fig. 2c, turned upside down for better comparison). b In vitro ultrasonographic image, the testicle submerged in a saline solution. c Low-power photomicrograph of the corresponding histological section (arrows). T atrophied testicular parenchyma
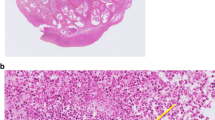
Histology shows that the atrophic testicle is composed of a necrotic centre surrounded by a thickened, fibrotic tunica albugninea. Punctate calcifications are found at the inner layers of the tunica albuginea and at the border between tunica and necrotic centre (Figs. 4c, 5). Hemosiderin deposits are also found. Correlation with ultrasonographic findings suggests that the calcifications cause the hyperechoic rim-like reflections (Fig. 4a, b).
High-power photomicrograph of the testis. a Normal testicle. Tunica albuginea (arrows) constitutes a thin layer surrounding the homogeneous testicular parenchyma. b Testicular atrophy after prenatal torsion. Tunica albuginea (arrows) is markedly thickened. Calcifications are seen at the inner border of the tunica (arrowheads) causing the hyperechoic rim
No in vitro study was done in the other 7 patients who underwent orchidectomy for torsion of the testis; however, ultrasonographic findings in these patients also were correlated with histologic findings. Two patients were surgically treated in an early stage (3 and 6 weeks), the others between 4 and 11 months of age. Histology showed typical punctate calcifications at the transitional zone between thickened tunica albuginea and affected testis in the patients who were surgically treated early, becoming more rim-like in time in the remaining patients. Also, the tunica albuginea itself became more fibrotic in time. These findings match the results of the in vitro study.
Discussion
Clinically, patients with prenatal testicular torsion present with a scrotal swelling and a palpable mass immediately after birth. The majority of torsions occur prenatally in utero and are manifest at birth [1, 7, 8, 9]. At this age torsion occurs at the level of the spermatic cord (extravaginal) as opposed to the usual intravaginal torsion occurring in adolescence [6, 7, 8, 9]. Extravaginal torsion of the spermatic cord involves both the testis and tunica vaginalis [6, 7] and results in haemorrhagic infarction of the testis. The cause of extravaginal torsion is unknown [8].
Traditionally, surgical exploration for suspected torsion of the testis has been the only definitive diagnostic modality, because reliance solely upon the physical findings increases the potential for error in diagnosis [5]. Because the potential for testicular salvage is remote, the principal reason for early surgical intervention is to confirm the diagnosis and differentiate a prenatal torsion of the testis from other intrascrotal pathological conditions [5]. The major problems in early operation are the potential risks inherent with surgery in newborns, and in particular, risks from general anaesthesia [5]. To avoid unnecessary surgery, ultrasonography (including colour Doppler) was proposed as the imaging modality of choice [5, 6].
Colour Doppler ultrasonography of the newborn testis may assist in the differential diagnosis of newborn scrotal masses [3, 4, 6, 8, 9, 10]. In our study colour Doppler ultrasonography revealed no testicular flow on the affected side in all 13 patients, which is a consistent finding in patients with torsion of the testis [2, 3, 5, 7, 9]. Zinn et al. stated that the absence of colour flow signal is diagnostic of acute testicular torsion [7]. We agree, however this seems only to be true when testicular flow is present on the contralateral normal side, which can be extremely difficult in neonates without state-of-the-art ultrasonographic equipment; thus, absence of testicular flow on both sides in the same study does not necessarily indicate bilateral torsion of the testis [6].
Moreover, although the sensitivity of absence of flow for the diagnosis of testicular torsion is high, the specificity is unknown for neonates.
On the other hand, colour Doppler ultrasonography can be very useful in differentiating torsion of the testis with absence of flow from haemangiomas and other solid tumours that most likely show flow on colour Doppler ultrasonography [4].
Subsequent grey-scale ultrasonography in our patient group showed scrotal swelling and the testis was more voluminous on the affected side, a finding also frequently seen by others [3, 6, 8].
In our study all patients showed heterogeneous testicular parenchyma with hypoechoic areas at presentation. In patients who were surgically treated in a relatively early stage (3 weeks) the ultrasonographic findings showed preoperatively an even more demarcated hypoechoic area in the affected testis, which proved to be infarction and necrosis of testicular parenchyma on histology. Torsion in neonates results in hemorrhagic infarction with necrosis resulting in a more heterogeneous parenchymal pattern than torsion in adolescents in whom the testis has a more homogeneous appearance [8].
On ultrasonography the thickened layer immediately around the testis parenchyma, partially hypoechoic and often more rim-like hyperechoic, proven to be the tunica albuginea on histological findings, also showed sharply demarcated hyperechoic reflections at the transitional zone between thickened tunica albuginea and affected testis parenchyma (Fig. 1). These hyperechoic reflections were also described by Cartwright et al. [3] and Brown et al. [6]. According to these authors the hyperechoic reflections were caused by calcifications in the tunica albuginea.
In the present study, histological examination showed these small calcifications mostly found at the transitional zone between tunica albuginea and residual atrophic testis parenchyma. When the testis was more atrophied at time of pathological investigation, also the rim-like calcifications were more pronounced. Our study was the first to perform an in vitro ultrasonographic study of a surgically removed testis after torsion, which confirmed that the rim-like reflections shown with ultrasonography corresponded with calcifications at the transitional zone between tunica albuginea and testicular parenchyma (Fig. 5). To our knowledge, no systematic ultrasonographic studies have been performed to investigate the testicular changes over time after prenatal torsion of the testicle. As shown in Fig. 3, 9 patients, the one with bilateral torsion of the testis included, had follow-up ultrasonographic studies. All 9 patients showed progressive testis atrophy on the affected side. The variation in testicular volume at presentation probably reflects the time interval since the initial event. Grey-scale ultrasonography showed the testis eventually to become more homogeneous and more hyperechoic with progression of the hyperechoic reflections, becoming continuous rim-like in time, due to progressive calcification.
Grey-scale ultrasonography of the normal hemiscrotum in patients with unilateral torsion revealed a normal testis with homogeneous parenchyma. The tunica albuginea itself cannot be visualized separately. In 10 patients a hydrocele was found in the normal hemiscrotum, a finding also described by others [6, 9, 10]. It is likely that these findings are secondary to inflammatory changes after contralateral torsion of the testis or represents a congenital abnormality, which can occur when there is an incomplete closure of the processus vaginalis, commonly reported in prenatal torsion [9].
The differential diagnosis of a scrotal swelling and a palpable mass in neonates includes hydrocele, haematocele, inguinal herniation, torsion of the appendix of the testis or epididymis, epididymo-orchitis, syphilitic orchitis, ectopic splenic or adrenal rests, meconium peritonitis, and benign and malignant tumours of the testes and epididymis [1, 2, 3, 4]. Ultrasonography can diagnose many of these entities: a primary differentiating factor that facilitates the diagnosis of a scrotal hernia in patients with a scrotal swelling is the observation of peristalsis within the scrotum at real-time sonography [4], hydroceles and hematoceles are manifested by a fluid-filled space within the scrotum next to the testes [4].
However, the most important diagnosis to exclude is a congenital testicular neoplasm. During the same period as the neonatal torsion study we reviewed all patients younger than 1 year of age with a testicular neoplasm who were referred to our hospital. Seven patients were identified, and all testicular neoplasms were confirmed with surgery and histology. At time of presentation they all were considerably older, the youngest 106 days of age and the oldest 319 days of age. Apparently, congenital testicular neoplasm is rare, or does not manifest during the neonatal period. In only three of these patients was a preoperative ultrasonographic study performed. Ultrasonography showed a cystic tumour in a swollen testis in 1 patient, a solid hypoechoic tumour in another patient and a partially solid and partially cystic tumour in the third patient.
Although the number of patients does not justify statistical analysis, it seems that young age (<1 month) and ultrasonographic appearance (heterogeneous parenchyma, thickened tunica albuginea and rim-like calcifications) strongly favours the diagnosis prenatal testicular torsion above testicular neoplasm.
Conclusion
Colour Doppler ultrasonography is the diagnostic modality of choice in a newborn with a painless congenital scrotal swelling and a palpable mass. Scrotal ultrasonography shows characteristic ultrasonographic features in diagnosing prenatal torsion of the testis: an enlarged testis; heterogeneous testis parenchyma; a thickened surrounding tunica albuginea; and diffuse or rim-like hyperechoic reflections (calcifications) at the transitional zone between testis and overlying tunica albuginea. These findings in combination with absence of testicular flow on the affected side are highly suggestive of prenatal torsion of the testis. Moreover, emergency surgical exploration can be postponed, because testicular salvage is not to be expected. In follow-up ultrasonographic studies progressive testis atrophy can be easily depicted and concomitant pathology can be studied.
However, asynchronous bilateral torsion is very rare, the contralateral testis can be evaluated as well in the follow-up ultrasonographic studies.
References
Das S, Singer A (1990) Controversies of perinatal torsion of the spermatic cord: a review, survey and recommendations. J Urol 143:231–233
Gross BR, Cohen HL, Schlessel JS (1993) Perinatal diagnosis of bilateral testicular torsion: beware of torsions simulating hydroceles. J Ultrasound Med 12:479–481
Cartwright PC, Snow BW, Reid BS, Schultz PK (1995) Color Doppler ultrasound in newborn testis torsion. Urology 45:667–670
Shipp TD, Benacerraf BR (1995) Scrotal inguinal hernia in a fetus: sonographic diagnosis. AJR 165:1494–1495
Stone KT, Kass EJ, Cacciarelli AA, Gibson DP (1995) Management of suspected antenatal torsion: What is the best strategy? J Urol 153:782–784
Brown SM, Casillas VJ, Montalvo BM, Albores-Saavedra J (1990) Intrauterine spermatic cord torsion in the newborn: sonographic and pathological correlation. Radiology 177:755–757
Zinn HL, Cohen HL, Horowitz M (1998) Testicular torsion in neonates: importance of power Doppler imaging. J Ultrasound Med 17:385–388
Zerin JM, DiPietro MA, Grignon A, Shea D (1990) Testicular infarction in the newborn: ultrasound findings. Pediatr Radiol 20:329–330
Ricci P, Cantisani V, Drudi FM, Carbone I, Coniglio M, Bosco S, Cozzi D (2001) Prenatal testicular torsion: sonographic appearance in the newborn infant. Eur Radiol 11:2589–2592
Hubbard AE, Ayers AB, MacDonald LM, James CE (1984) In-utero torsion of the testis: antenatal and postnatal ultrasonic appearances. Br J Radiol 57:644–646
Acknowledgements
The authors thank T. Rijsdijk and A. Zwamborn for preparing the figures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van der Sluijs, J.W., den Hollander, J.C., Lequin, M.H. et al. Prenatal testicular torsion: diagnosis and natural course. An ultrasonographic study. Eur Radiol 14, 250–255 (2004). https://doi.org/10.1007/s00330-003-2019-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-003-2019-0