Abstract
The purpose of this study was to evaluate whether a second cycle of contrast-enhanced voiding urosonography (VUS) with no added contrast medium (CM) can increase the detection rate of vesicoureteral reflux (VUR). One hundred twelve consecutive children with a mean age of 2.9 years with 224 kidney-ureter units (KUU) underwent two cycles of contrast-enhanced harmonic VUS. The first cycle of VUS was performed with 3.5–12.5 ml of suspension 300 mg/ml SH U 508 A and was followed immediately by a second cycle with only saline without adding CM. VUR was detected in 57 KUU from 44 children (39%) at the first cycle of VUS. Eight of the remaining 68 non-refluxing children (12%) demonstrated VUR at the second cycle (P=0.045). Most cases of missed reflux at the first cycle were grade II (75%). However, in two KUU from two children missed reflux was grade III. In one child reflux (grade II) was missed on the second cycle. Comparing the second cycle of VUS with the first cycle, concordant findings regarding the presence or absence as well as the grade of reflux were found in 94% of KUU. A second cycle of contrast-enhanced harmonic VUS with no added CM discloses significantly more cases of VUR at no additional cost for the examination.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vesicoureteral reflux (VUR) is one of the most common abnormalities of the urinary tract found in children with urinary tract infection (UTI), in siblings of children with VUR and in neonates with antenatally detected urinary tract dilatation [1–9]. The standard diagnostic method for evaluation of VUR is fluoroscopic voiding cystourethrography (VCUG), although the reliability of this technique has been questioned since VUR may be intermittent [10–12]. Therefore, cyclic VCUG has been used to demonstrate reflux in up to 20% of the cases with negative first cycle [10–12]. However, a second cycle increases the radiation dose, limiting its widespread application. Direct radionuclide cystography (DRNC) is a reliable alternative with a significantly smaller radiation dose; however, it is less available, and it has poor anatomical resolution [13, 14]. Contrast-enhanced voiding urosonography (VUS) with microbubbles containing contrast medium (CM) made of galactose-palmitic acid (SH U 508 A, Levovist; Schering, Berlin, Germany) has been used for the last 10 years and has been found to be equally sensitive compared to VCUG and DRNC [15–25]. Harmonic imaging has been shown to be significantly better at depicting microbubbles in the ureters and pelvicalyceal system [26–28]. Performing cyclic VUS further increases the sensitivity for detecting reflux, even without harmonic imaging [29, 30]. However, adding CM in the second cycle further increases the cost of the examination. The remaining small amount of CM after the first micturition is more conspicuous when scanned with harmonic imaging than with the fundamental mode. The purpose of our study is to enhance the ability of VUS to depict reflux by performing two cycles of contrast-enhanced VUS using harmonic imaging without increasing the cost of the examination.
Materials and methods
Between November 2003 and July 2004, 117 consecutive children referred for possible reflux were examined by contrast-enhanced VUS. The clinical indications for reflux examination were: UTI (n=75), follow-up of VUR after conservative (n=22) or surgical management (n=1), antenatal diagnosis of hydronephrosis (n=15), enuresis (n=2) and being a sibling of patients with VUR (n=2). This study was approved by the Ethics Committee of our hospital, and informed consent was obtained in all cases after the procedure was fully explained to the parents and older children.
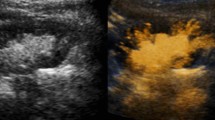
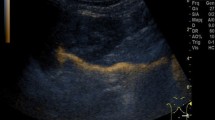
US examinations were performed with the contrast-harmonic mode of commercially available US apparatuses (Esaote-Technos, Esaote, S.p.A., Genoa, Italy, and General Electric, Logiq 9, GE Medical Systems, Waukesha, WI) using 3.5 and up to 10 MHz convex or linear transducers. The mechanical index (MI) was set at 0.3–0.8 for fundamental and 0.5–1.3 for harmonic imaging. The highest MI was used instantly during “flashing,” a technique purposely used to break refluxing microbubbles and make reflux more conspicuous. Standard US of the urinary tract was performed in all patients before the evaluation for reflux. Evaluation for reflux included a first cycle of contrast-enhanced VUS using a suspension of 99.9% galactose and 0.1% palmitic acid diluted in sterile water (Levovist, Schering) at a concentration of 300 mg/ml as a contrast medium (CM) in the supine or prone positions, followed immediately by a second cycle without additional CM.
After the baseline US examination of both kidneys, a transurethral catheterization of the bladder was performed with a 6- or 8-F infant feeding tube connected to a three-way stopcock connected also to a bottle of saline placed 80 cm above the patient’s bladder level. The volume of saline was more than twice the predicted bladder capacity that is sufficient for the two cycles of the examination, and it was estimated according to the formula: volume (in ml) = age (in years) +2×30 [31]. The bladder was emptied and subsequently half filled with saline by means of gravity. CM prepared according to directions written on the leaflet included in the drug was then instilled very slowly, and saline infusion was repeated until the bladder was full. The amount of Levovist suspension given was 3.5 ml in infants up to 1 year, 7.5 ml in children up to 4 years and 12.5 ml in older children, corresponding to approximately 5–7% of the final bladder volume. The level of saline was marked on the bottle at the point the child started voiding, and the infusion was stopped. US examination of the kidneys, bladder and retrovesical area was performed during bladder filling, voiding and immediately after voiding on both cycles. Emphasis was given to the kidneys rather than to the ureters unless the latter were dilated. That was decided because grade I reflux is not treated according to the clinical practice at our hospital, although it can potentially vary to a higher grade in an individual patient.
After the completion of voiding of the first cycle in older children or when the bladder was almost empty in the younger ones, a second cycle was performed with an infusion of saline only. The amount of saline infused for the second cycle was about the same as in the first cycle, and the entire procedure was repeated under the same conditions. No additional amount of Levovist was used for the second cycle, which was completed provided that the remaining number of CM microbubbles present in the bladder after complete voiding of first cycle was adequate to produce strong, evenly fine echoes. There were only five children in whom the amount of CM in the bladder during the second cycle was considered inadequate to produce diagnostic images. These children were excluded from the study. Finally, 112 patients with 224 kidney-ureter units (KUU) are included in this report (48 boys and 64 girls; mean age 2.9 years; SD 3.2 years; range 24 days to 14 years). The results were assessed in terms of patients and in terms of KUU. KUU is comprised of a renal pelvis with its own ureter inserting separately in the bladder. Repeat US examination of the kidneys during the second cycle bladder filling and voiding was done. After the end of the second cycle, US of the bladder was performed to assess for residual volume. The duration of each cycle of the examination as well as the volume of saline infused were recorded. The examinations were captured on hard copies using a laser camera (Agfa, Drystar 2000, Belgium), and images as well as video clips were recorded on compact disk in Dicom format. A commercially Dicom viewer software (efilm, efilm Medical Inc, Toronto, Canada) was used for offline evaluation of the examination in an ordinary personal computer. The vital signs were documented during the examination, and any sign of an adverse event during and 24 h after the examination was recorded.
All children were under prophylactic antibiotic therapy according to our pediatric clinic protocol, and no sedation was used in any case. Contrast-enhanced VUS was performed and interpreted in consensus by two experienced radiologists. The diagnosis of reflux on contrast-enhanced VUS was based on the appearance of microbubbles in a ureter or renal pelvis. Grading of VUR on VUS was similar to VCUG (five grades) [32]. Evaluation of grade I reflux in both cycles of VUS was not carried out consequently unless dilatation of the ureter was present.
For statistical analysis, the SPSS version 12 statistical program was used. The least significance difference test for post hoc comparisons, McNemar, t-Student’s and kappa coefficient-κ tests were applied where indicated. Tests were judged significant at P<0.05.
Results
Results in terms of patients are shown in Table 1. Forty-four children were found refluxing during the first cycle of contrast-enhanced harmonic VUS. Of the remaining 68 children with negative first cycle, 8 children (12%) showed reflux during the second cycle. Comparing the first cycle of contrast-enhanced harmonic VUS with the second cycle, concordant findings regarding the presence (43 patients) or absence (60 patients) of reflux were found in 103 (92%) patients (κ=0.84; 95% CI=0.73–0.94). In one patient reflux was disclosed only on the first cycle of VUS and in eight only on the second cycle (P=0.045).
In terms of KUU, reflux was present in 57 units during the first cycle, and of the remaining 167 non-refluxing KUU, 12 units showed reflux on the second cycle (P=0.005). Concordant findings regarding the presence or absence as well as the grade of reflux were found in 211 (94%) units: 55 units were found to be refluxing with both methods with the same degree and 155 units were found to be normal on both (Tables 2 and 3). In 1 unit, VUR was disclosed only on the first cycle (grade II) and in 12 units VUR was shown only on the second cycle of contrast-enhanced harmonic VUS (one grade I, nine grade II and two grade III). Moreover, in one case the second cycle upgraded VUR from grade II to III. There was strong agreement in the findings between the two cycles according to the kappa coefficient value (κ=0.86; 95% CI: 0.78–0.93).
No significant difference was found between children refluxing only on the second cycle and those who were not refluxing at all regarding mean age (30.3±34.2 versus 41.8±44.2 months; P=0.12), clinical indications, bladder capacity (125±79 versus 136±70 ml; P=0.89) and Levovist concentration (6% versus 5.5%; P=0.85). There was also no significant difference in the mean age, bladder capacity and Levovist concentration among children refluxing on the first and those with reflux only on the second cycle (39.5±32.3 versus 30.3±34.2 months; P=0.11; 128±83 versus 125±79 ml; P=0.97; 5.8 versus 6%; P=0.93). No significant differences were found in the mean values of liquid volume infused during the first and second cycle of VUS (130±93 and 135±69 ml, respectively; P=0.95). Residual urine volume after the second voiding was found in eight patients (7%). Considering all refluxing units as true positives, the sensitivity of the first and second cycles were 87 and 98%, and the negative predictive values 84 and 98%, respectively.
No adverse event related to the installation of Levovist was recorded immediately or 24 h after the examination, and the procedure was well tolerated by all children. The mean times of each step of the examination were as follows: baseline US, 8±3 min; bladder catheterization, 7±2 min; first cycle of contrast-enhanced VUS, 13±7 min; second cycle, 4±6 min. No significant difference in the mean duration of the examination was recorded between children refluxing and those who were not (15.2±6 versus 18.8±5 min, respectively). Microbubbles in the bladder that were visible for making a diagnosis were present up to 55 min after the preparation of the suspension.
Discussion
Primary VUR has been considered an abnormality of the maturation of the vesicoureteral junction [33]. It is a commonly found abnormality in children with UTI, siblings of children with reflux, infants with antenatally diagnosed hydronephrosis as well as children with other urinary tract abnormalities [1–9]. VCUG and DRNC are considered the standard methods to diagnose and follow-up VUR, each having its own specific indications. However, both methods involve ionizing radiation, although with DRNC it is much less than with VCUG [13, 14]. To overcome this problem, US methods have been developed for the evaluation of VUR utilizing air [34], air bubbles in shaken saline [35], sonicated albumin [36, 37] and, more recently, special US contrast media made from galactose suspension [15–32]. These are used to enhance the ability of US to detect VUR. In fact, recent reports indicate that contrast-enhanced VUS has equal or higher sensitivity to detect reflux compared with the standard methods [15, 16, 18, 19, 21]. Moreover, contrast-specific techniques using harmonic imaging have further improved this efficacy [26, 27]. We became attracted to this method because we have to confront more than 200 requests a year for the evaluation of reflux in our pediatric radiology department. We performed two cycles of contrast-enhanced VUS at the same session. The second cycle of contrast-enhanced VUS was chosen based on previous published data from VCUG indicating that VUR may be an intermittent phenomenon better evaluated when a second cycle is made available. Cyclic VCUG enhances the ability of the method to disclose reflux, as 12–20% of the negative examinations during the first cycle were found to have reflux during the second cycle [10–12]. For this reason, cyclic VCUG has been proposed as a standard procedure, at least in cases at high risk for reflux. However, although very useful in certain cases, cyclic VCUG gives more radiation to the gonads despite certain lower dose techniques (e.g., pulsed fluoroscopy). Contrast-enhanced VUS, which is free of ionizing radiation, could be performed in more than one cycle to increase the reflux detection rate. This, of course, will significantly increase the cost of the examination, considering that the price of this drug in our country is 113.06 and 75.48 Euros for the 4- and 2.5-g vial of Levovist, respectively. We performed the second cycle of contrast-enhanced harmonic VUS with no additional contrast medium, and we disclosed reflux in 12 KUU in 8 out of 68 (12%) children with a negative first cycle. This difference in reflux detection was significant (P=0.045). More importantly, these eight patients would not have been treated if a second cycle had not been performed. Missed reflux on the first cycle, disclosed only during the second cycle of VUS, was mostly of mild degree (grade I in one KUU and grade II in nine KUU). However, there were two KUU with VUR grade III shown only during the second cycle. We found only two reports in the literature on cyclic VUS for detecting VUR, both from Kenda et al. and without using harmonic imaging [29, 30]. The first includes renal transplant recipients of whom only eight were children. In this report, although the sensitivity in diagnosing VUR was not improved, the cyclic examination significantly upgraded the already diagnosed reflux. In the second study (49 children), the same authors found 25% more VUR than with the conventional one-cycle VUS (P=0.049). In both studies, however, the authors used 7–11 ml of Levovist suspension at 300 mg/ml per cycle, which is 14–22 ml in total. This is twice the amount of contrast we used for the two cycles of VUS.
A drawback of our study is that the amount of Levovist present during the second cycle, although adequate to produce diagnostic images, is not constant. Nevertheless, it is of interest that VUR was diagnosed in 12 KUU only during the second cycle of VUS. Moreover, the reported amounts and concentrations of Levovist used for contrast-enhanced VUS vary widely in the literature. The reported amount of CM ranged from 5 to 10% of the bladder capacity and the concentration of CM from 200 to 400 mg/ml [15–19]. The most commonly used dosage for the intravesical application of a 300 mg/ml dilution of Levovist is 10% of the bladder-filling volume [38]. Kenda et al. have used a lower dosage (5% of the bladder capacity) of 300 mg/ml Levovist, with comparable results and apparently at a lower cost [18]. We keep the cost of the examination to a minimum by using 3.5 ml of Levovist 300 mg/ml in infants up to 1 year of age, 7.5 ml in children up to 4 years and 12.5 ml in older children, corresponding to approximately 5–7% of the final bladder volume. This amount of CM is being used for both cycles because we performed the second cycle of contrast-enhanced VUS by introducing only saline in the bladder and by using the remaining microbubbles of CM that were trapped in the bladder from the first cycle, possibly between the mucosal folds. The number of microbubbles present on the second cycle was enough to produce diagnostic images in 96% of our patients. It should be mentioned, however, that the use of a contrast-specific harmonic mode is a prerequisite to increase the sensitivity of the method to disclose refluxing microbubbles significantly [26–28].
We now have started dividing the estimated amount of CM for VUS in two unequal doses: 2/3 for the first cycle and 1/3 for the second cycle, further reducing the cost of the examination. This practice is an ongoing project in our department. No significant difference regarding the mean age, clinical indications and bladder capacity was found between children refluxing only on the second cycle and those who did not, as well as between children refluxing on the first and those with reflux only on the second cycle (P>0.05). Nevertheless, our results are comparable to those reported on cyclic VCUG [10–12].
A reason for the higher sensitivity of cyclic VUS is probably the longer time of monitoring allowed, providing a better time window for detection of intermittent reflux. In our study, the mean monitoring times for possible reflux were 13±7 and 4±6 min for the first and second cycle of contrast-enhanced VUS, respectively (17±6 min total). Darge et al. reported a mean time of 14±7 min for contrast-enhanced VUS and 1.8±1.4 min for VCUG [16]. Respective times reported by Berrocal et al. were 15±6 and 1.8±1 min [19].
We did not make much effort to disclose reflux grade I by scanning the retrovesical space sonographically unless dilatation was present for two reasons: first, because it is hard to differentiate a few echogenic microbubbles in a non-dilated ureter surrounded by retrovesical echogenic tissues and second, because the clinical importance and treatment of VUR grade I are controversial. Moreover, no treatment is given in cases of grade I reflux at our institution.
The main disadvantage of contrast-enhanced VUS is the difficulty in disclosing anatomical or functional abnormalities of the bladder and urethra. Therefore, VCUG should remain the method of choice for the first evaluation of boys and children with the symptoms or history of an unstable bladder. In conclusion, the results of this study demonstrate that by performing a second cycle of contrast-enhanced voiding urosonography, more cases of intermittent reflux can be detected without increasing the amount of the echo-enhancing agent and the cost of the examination.
References
Smellie JM, Hodson CJ, Edwards D, Normand ICS (1964) Clinical and radiological features of urinary infection in childhood. Br Med J 2:1222–1226
Tanagho EA, Hutch JA, Meyers FH, Rambo ON Jr (1965) Primary vesicoureteral reflux: experimental studies of its etiology. Br J Urol 93:165–176
Lebowitz RL, Colodny AH (1973) Urinary tract infection in children. Crit Rev Clin Radiol Nucl Med 4:457–475
Noe NH, Wyatt RJ, Peeden JN, Rivas ML (1992) The transmission of vesicoureteral reflux from parent to child. J Urol 148:1869–1871
Noe NH (1992) The long term results of prospective sibling reflux screening. J Urol 148:1739–1742
Zerin JM, Ritchey ML, Chang ACH (1993) Incidental vesicoureteral reflux in neonates with antenatally detected hydronephrosis and other abnormalities. Radiology 187:157–160
Song JT, Ritchey ML, Zerin MJ, Bloom DA (1995) Incidence of vesicoureteral reflux in children with unilateral renal agenesis. J Urol 153:1249–1251
Lebowitz RL, Blickman JG (1983) The coexistence of obstruction and reflux. Am J Roentgenol 140:231–238
Scott JE, Swallow V, Coulthard MG, Lambert HJ, Lee RE (1997) Screening of newborn babies for familial ureteric reflux. Lancet 350:396–400
Paltiel HJ, Rupich RC, Kiruluta HG (1992) Enhanced detection of vesicoureteral reflux in infants and children with use of cyclic voiding cystourethrography. Radiology 184:753–755
Papadopoulou F, Efremidis S, Oiconomou A, Badouraki M, Panteleli M, Papachristou F, Soteriou I (2002) Cyclic voiding cystourethrography: is vesicoureteral reflux missed with standard voiding cystourethrography? Eur Radiol 12:666–670
Jequier S, Jequier J (1989) Reliability of voiding cystourethrography to detect reflux. Am J Roentgenol 153:807–810
Willi V, Treves S (1983) Radionuclide voiding cystography. Urol Radiol 5:161–173
Lebowitz RL (1992) The detection and characterization of vesicoureteral reflux in the child. J Urol 148:1640–1642
Bosio M (1998) Cystosonography with echocontrast: a new imaging modality to detect vesicoureteric reflux in children. Pediatr Radiol 28:250–255
Darge K, Troeger J, Duetting T, Zieger B, Rohrschneider W, Moehring K, Weber C, Toenshoff B (1999) Reflux in young patients: comparison of voiding US of the bladder and retrovesical space with echo enhancement versus voiding cystourethrography for diagnosis. Radiology 210:201–207
Farina R, Arena C, Pennisi F, Di Benedetto V, Politi G, Di Benedetto A (2000) Vesico-ureteral reflux: diagnosis and staging with voiding color doppler US. Preliminary experience. Eur J Radiol 35:49–53
Kenda R, Novljan G, Kenig A, Hojker S, Fettich J (2000) Echo-enhanced ultrasound voiding cystography in children: a new approach. Pediatr Nephrol 14:297–300
Berrocal T, Gaya F, Arjonilla A, Lonergan G (2001) Vesicoureteral reflux: diagnosis and grading with echo-enhanced cystography versus voiding cystourethrography. Radiology 221:359–365
Radmayr C, Klauser A, Pallwein L, Zumadden D, Bartsch G, Frauscher F (2002) Contrast-enhanced reflux sonography in children: a comparison to standard radiological imaging. J Urol 167:1428–1430
Kmetec A, Bren AF, Kandus A, Fettich J, Buturovic-Ponikvar J (2001) Contrast-enhanced ultrasound voiding cystography as a screening examination for vesicoureteral reflux in the follow-up of renal transplant recipients: a new approach. Nephrol Dial Transplant 16:120–123
Escape I, Martinex J, Bastart F, Soltuga C, Sala P (2001) Usefulness of echocystography in the study of vesicoureteral reflux. J Ultrasound Med 20:145–149
Ascenti G, Chimenz R, Zimbaro G, Mazzioti S, Scribano E, Fede C, Ricca M (2000) Potential role of colour-Doppler cystosonography with echocontrast in the screening and follow-up of vesicoureteral reflux. Acta Paediatr 89:1336–1339
Valentini AL, Salvaggio E, Manzoni C, Rendeli C, Destilo L, Summaria V, Campioni P, Marano P (2001) Contrast-enhanced gray-scale and color Doppler voiding urosonography versus voiding cystourethrography in the diagnosis and grading of vesicoureteral reflux. J Clin Ultrasound 29:65–71
Mentzel HJ, Vogt S, Patzer L, Schubert R, John U, Misselwitz J, Kaiser WA (1999) Contrast-enhanced sonography of vesicoureterorenal reflux in children:preliminary results. Am J Roentgenol 173:737–740
Darge K, Moeller RT, Trusen A, Butter F, Gordjani N, Riedmiller H (2005) Diagnosis of vesicoureteral reflux with low-dose contrast-enhanced harmonic ultrasound imaging. Pediatr Radiol 35:73–78
Darge K, Zieger B, Rohrscheider W,Ghods S, Wunsch R, Troeger J (2001) Contrast-enhanced harmonic imaging for the diagnosis of vesicoureteral reflux in pediatric patients. Am J Roentgenol 177:1411–1415
Kopitzko A, Cornely D, Reither K, Wolf K, Albrecht T (2004) Low contrast dose voiding urosonography in children with phase inversion imaging. Eur Radiol 14:2290–2296
Kenda RB, Kenig A, Novljan G, Ponikvar R, Ponikvar JB (2001) Cyclic voiding urosonography for detecting vesicoureteric reflux in renal transplant recipients. Nephrol Dial Transplant 16:2229–2231
Novljan G, Kenig A, Rus R, Kenda RB (2003) Cyclic voiding urosonography in detecting vesicoureteral reflux in children. Pediatr Nephrol 18:992–995
Berger RM, Maizels M, Moran GC, Conway JJ, Firlit CF (1983) Bladder capacity (ounces) equals age (years) plus 2 predicts normal bladder capacity and aids in diagnosis of abnormal voiding patterns. J Urol 129:347–352
Darge K, Troeger J (2002) Vesicoureteral reflux grading in contrast-enhanced voiding urosonography. Eur J Radiol 43:122–128
Hutch JA (1961) Theory of maturation of the intravesical ureter. J Urol 86:534–538
Siamplis D, Vasiou K, Giarmenitis S, Frimas K, Zavras G, Fezoulidis I (1996) Sonographic detection of vesicoureteral reflux with fluid and air cystography. Comparison with VCUG. Rofo Fortschr Geb Roentgenstr Neuen Bildgeb Verfahr 165:166–169
Hanbury DC, Coulden RA, Farman P, Sherwood J (1990) Ultrasound cystography in the diagnosis of vesicoureteral reflux. Br J Urol 65:250–253
Kaneko K, Kuwatsuru R, Fukuda Y, Yamataka A, Yabuta K, Katayama H, Miyano T (1994) Contrast sonography for detection of vesicoureteral reflux. Lancet 344:687
Atala A, Ellsworth P, Share J, Paltiel H, Walker RD, Retic AB (1998) Comparison of sonicated albumin enhanced sonography to fluoroscopic and radionuclide voiding cystography for detecting vesicoureteral reflux. J Urol 160:1820–1822
Darge K (2002) Diagnosis of vesicoureteral reflux with ultrasonography. Pediatr Nephrol 17:52–60
Acknowledgement
We thank Prof. K Darge of Wurzburg University Hospital, Germany, for his instructive advice in the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Papadopoulou, F., Tsampoulas, C., Siomou, E. et al. Cyclic contrast-enhanced harmonic voiding urosonography for the evaluation of reflux. Can we keep the cost of the examination low?. Eur Radiol 16, 2521–2526 (2006). https://doi.org/10.1007/s00330-006-0253-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0253-y