Abstract
Percutaneous vertebroplasty has become an efficient technique for the treatment of painful vertebral fractures. Osteoporotic vertebral compression fractures are characterized by severe back pain and immobilization causing other complications like thrombosis or pneumonia. Vertebral cement augmentation provides increased strength of the vertebral body and an obvious pain relief. Between 1989 and 2004, 30 studies and a total of 2,086 treated patients have been published in literature. A review of these studies has been performed. The number and age of the patients, number of treated vertebrae, pre- and postoperative outcome of pain and complications of the different studies were assessed and analyzed. Percutaneous vertebroplasty is an efficient technique with low complication rates and a significant reduction in pain. It rapidly improves the mobility and quality of life of patients with vertebral compression fractures. With an increasing number of treated patients, experience with this interventional technique has become excellent. But still there are no randomized controlled trials available, showing that percutaneous vertebroplasty has a significantly better outcome than other treatment options, especially after a long-term follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a disease characterized by low bone mass and the structural deterioration of bone tissue, leading to bone fragility and an increased susceptibility to fractures. The consequences of this chronic disease and public health threat will increase rapidly in the next decades and will be caused by the increasing number of elderly people [1]. The spine is the most frequently affected localization for osteoporosis-induced fractures [2, 3]. In the U.S., osteoporosis is responsible for more than 1.5 million fractures annually, including approximately 700,000 vertebral fractures [4–6]. Consequences of these fractures are pain, collapse of the vertebral body and loss of the physiological posture. Concomitant complications are various and comprise orthopedic, pulmonary, cardiovascular and neurological diseases. In the U.S., the socio-economic consequences are the estimated national direct expenditures (hospitals and nursing homes) for osteoporosis and related fractures of more than $14 billion each year [4]. Percutaneous vertebroplasty is a minimally invasive technique in the therapy of vertebral compression fractures and was described first by Galibert and Deramond in 1987 [7]. It is used to augment and immobilize the vertebral body and therefore to relieve pain and restore the mobility and quality of life of the patients.
Patients and methods
Vertebroplasty technique
The standard technique for percutaneous vertebroplasty has been described explicitly before [5, 8, 9]. High-quality fluoroscopy equipment is essential. A combination of fluoroscopy and computed tomography is possible and has been described by some authors before [10–13]. In most of the studies, percutaneous vertebroplasty was carried out under local anesthesia. To provide conscious sedation, different medications are used. In our center, we prefer to use fentanyl (Sublimaze; Labors Abbott, Nordchicago, IL) and midazolam (Versed; Roche Pharma, Manati, Puerto Rico).
Under fluoroscopic control, the pedicle must be adjusted carefully so that it projects over the targeted vertebral body. The transpedicular approach is used most often in the lumbar spine, while the extrapedicular approach in the thoracic spine. After positioning of the patient and preparation in a strictly sterile manner, the cannula is placed through a small skin incision into the bone. The exact positioning of the vertebroplasty cannula is important to assure satisfying bone cement filling of the vertebral body. Under continued anteroposterior and lateral fluoroscopic control, the cannula is advanced into the vertebral body. After correct positioning of the cannula, either uni- or bipedicular, the bone cement is prepared. Different systems are used for application of the bone cement. Most often, the use of Luer-lok syringes is reported. During injection of the cement, continuous observation is necessary to prevent excessive bone cement leakage. Although bone cement achieves approximately 90% of its ultimate strength within 1 h of injection [14], the patients should be hospitalized at least for the day of the intervention. Figs. 1 and 2 show examples of uni- and bipedicular percutaneous vertebroplasty.
a A 69–year–old female patient. Unipedicular percutaneous vertebroplasty of the first sacral vertebral body (S1). Axial CT scan shows entering of the vertebroplasty cannula. b A 69–year–old female patient. Unipedicular percutaneous vertebroplasty of the first sacral vertebral body (S1). Axial CT scan shows application of bone cement
a A 74–year–old female patient. Bipedicular percutaneous vertebroplasty of thoracic vertebra 12. Axial CT scan shows entering of the vertebroplasty cannula. b A 74–year–old female patient. Bipedicular percutaneous vertebroplasty of thoracic vertebra 12. Axial CT scan shows the vertebral body after satisfactory application of bone cement
Data analysis
The study design is retrospective with retrospective data evaluation of studies found in the literature. Mean values were calculated, and for analysis, paired comparison procedures were used (paired t-test). P≤0.05 was considered to be statistically significant.
Patient selection for vertebroplasty
The results of percutaneous vertebroplasty are very promising. As can be seen in Figs. 3 and 4, vertebroplasty is gaining acceptance. The number of publications and the number of treated patients have obviously been increasing, especially in the period from 1999 to 2004. Due to the ongoing increasing number of treated patients, quality improvement guidelines have been set up to secure high standards. Tables 1, 2 and 3 show the indications and contraindications for vertebroplasty established by the American Society of Interventional Radiology and by the German Society of Radiology [5, 8].
Results of Percutaneous Vertebroplasty between 1989 and 2004
1. Patient data
Thirty studies were found in the literature from 1989 to 2004. Two thousand eighty–six patients (5,849 vertebral bodies) were treated (Table 4 and Fig. 4). The minimum number of treated vertebrae per study was 14; the maximum number was 1,398. The mean number of treated vertebrae per patient was 1.9 (range: 1.2–4.4; Table 4). The median age of the treated patients between 1989 and 2004 was 68.9 years (median range: 57.5–79; Table 4). The youngest treated patient was 20 years old [9, 15], and the oldest treated patient was 98 years old [16]. The female ratio was 67.4%, and the mean follow-up was 12.5 months (range: 28 days–5 years; Table 4).
2. Pain documentation
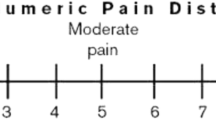
Pain is the main indication for treatment by percutaneous vertebroplasty. There are different scales for the measurement of pain. Most authors use the visual analogue scale (VAS), which is divided into 10 grades: 0 for no pain and 10 for a maximum of pain [17]. VAS has been documented in 19 of the 30 studies. Before treatment, the mean VAS was 8.1 (mean range: 6.4–9.7; see Table 5). After percutaneous vertebroplasty, pain was reduced significantly down to VAS 2.6 (mean range: 1.7–3.9; P<0.001; see Table 5). Fig. 5 shows a graphical summary of the VAS documentation of the different studies. In those studies, pain was reduced significantly by 5.5 points or 67.9% (P<0.001). Most of the missing data studies (11/30) reported the pain improvement in percentages. The exact definitions of pain improvement were often not documented and are therefore not comparable.
3. Vertebroplasty technique
In the first years of percutaneous vertebroplasty, many patients were treated using general anesthesia. However, more patients have been treated using local anesthesia in the last years. Many authors describe the advantage of local anesthesia as being that communication with the patient, especially concerning neurological symptoms, is possible. Neural affections can therefore be detected earlier. General anesthesia was carried out in 15% of the patients, strictly local anesthesia in 30% and a combination of local and neuroleptanalgesia in 55% of the patients (see Table 6) [9, 11, 15, 16, 18–32].
Most of the authors use fluoroscopy for percutaneous vertebroplasty (75%; see Table 6). Some authors describe a combination of fluoroscopy and CT as a useful upgrade for exact positioning of the vertebroplasty cannula and for an earlier detection of bone cement leakages (25%; see Table 6) [10, 11, 13, 14]. The mean size of the cannula used was 11.1 G (range: 7–14; see Table 6). In the thoracic and lumbar spine, different approaches to the vertebral body are described. A transpedicular or extrapedicular/posterolateral entrance into the vertebral body is used. In this review, most authors used a transpedicular approach (61%, see Table 6). Of the authors, 5.5% described the extrapedicular approach, and 33.5% used both extrapedicular and transpedicular approaches to the vertebral body (see Table 6).
4. Complications
In most of the studies, complications were divided into serious and non-serious complications. Serious and symptomatic complications are rare and were only documented in 0.9% of all treated patients in this review (see Table 7). Especially severe bone cement leakage and neurological compression making surgical therapy necessary have been described. Transient symptomatic complications like a radiculopathy or neuritis have been described more often. None of the patients died as a result of percutaneous vertebroplasty. Cement embolism was documented in less than 0.1% and was asymptomatic in all cases. Severe embolism, especially symptomatic lung embolism, was not described, but can be found in several case reports [33, 34]. The rates of bone-cement-induced complications are higher. Bone cement leakage was described in 41.2% (range: 7–81; see Table 7) [9, 11, 15, 16, 18–32]. However, more than 98% of the leakages were minor and asymptomatic. Only solitary cases made surgical therapy necessary [15, 33–35].
Discussion
Osteoporosis is responsible for more than 1.5 million fractures annually, including approximately 700,000 vertebral fractures in the U.S. [4]. The associated morbidity and mortality will have a high socio-economic impact. Percutaneous vertebroplasty is a cost-effective interventional procedure and can be performed under local anesthesia and conscious sedation as an outpatient procedure. With the rising number of patients and experience, the results after 17 years of percutaneous vertebroplasty are promising. Thirty studies with a total of 2,086 of treated patients and 5,849 treated vertebrae have been found in the literature between 1989 and 2004. Especially in the last 4 years, the number of studies and patients has been rising rapidly (Figs. 3 and 4). Most of the patients have been treated by radiologists: 66.7%. In the first decade of vertebroplasty, most authors preferred a longer hospitalization or general anesthesia [9, 18, 29, 32]. However, in the last years, treatment strategies have changed, and many patients have been treated on an outpatient basis under local anesthesia. Most of the studies presented two primary endpoints: a reduction of pain and the type and number of complications.
1. Evaluation of pain
Pain and reduced mobility are the most harassing consequences of vertebral body fractures. The majority of the studies reported a significant reduction of pain with an average VAS score of 8.1 before and 2.6 after treatments (see Table 5). The effects of percutaneous vertebroplasty on the reduction of pain are still not clearly understood. The analgesic effect can be explained by the immobilization of the vertebral body fracture and the heat effects on nerve endings [10, 22, 31, 36]. Vertebral compression fractures are caused by bone turnover, micro-damage and consecutively macro-damage. Changes in bone matrix structural factors, such as collagen, glycans and minerals, lead to micro-damage of the bone and therefore especially of the fractured trabeculae [36, 37]. Considering that bone also stores energy generated from the stresses of movement, it might be that already micro-fractures generate pain. The analgesic effect could therefore be explained by the stabilization and immobilization of the macro- and micro-fractures. Polymerization heat is another important factor in the reduction of pain. Pain-sensitive nerve endings seem to be damaged by the extensive impact of heat, and therefore local pain seems to be reduced additionally [36]. Polymerization of bone cement results in a partly severe cytotoxicity [38–40]. However, toxic effects due to PMMA in bone are not clearly understood yet. Actually, only a few in-vivo examinations can be found in the literature [38]. Larger series need to show more details to understand the long-time effects of bone cements.
2. Evaluation of complications
Serious and symptomatic complications in percutaneous vertebroplasty are rare and have only been reported in less than 1% (Table 7) [9, 11, 15, 16, 18–32]. Adjusting the pedicles under fluoroscopy before injecting the vertebroplasty cannula and the careful application of the bone cement under constant radiological control seem to be the most important factors to prevent complications.
Adjacent vertebral body fractures after percutaneous vertebroplasty have been described in several articles [9, 29, 41]. At this time, no evidence-based data are available showing that there is a significantly increased risk of subsequent fractures due to the vertebroplasty and not due to the natural history of the osteoporosis. Still, there are many patients treated by percutaneous vertebroplasty without a detailed examination for osteoporosis and especially without adequate medication.
The rate of bone-cement-induced complications is higher, especially regarding bone cement leakages. Reviewing the literature, the mean leakage rate is 41% [9, 11, 15, 16, 18–32] (Table 7). However, more than 98% of the leakages are asymptomatic. Only solitary cases of serious complications have been reported in the literature [15, 33–35]. Hodler et al. divided bone cement leakage into two grades [15]: grade 1 (minor) leakage: the longest diameter of the extravertebral bone-cement collection is less than the longest diameter of the closest pedicle; grade 2 (moderate) leakage: the longest diameter of the extravertebral bone-cement collection is greater than the longest diameter of the closest pedicle, but less than the nearest normal vertebral body. Many authors describe a minor leakage (grade 1) when the maximum amount of injectable bone cement is reached [9, 11, 15, 16, 18–32, 42]. The question is whether it is necessary to document minor leakage as a complication or to use it as a possibility for optimal filling of the vertebral body.
Evidence-based evaluation of percutaneous vertebroplasty
Most of studies found in the literature presented retrospective findings. Only seven studies (23.3%) were prospective trials. Still, there is no prospective randomized controlled trial (RCT) existent. Difficulties in comparing the different studies and evaluating primary and secondary endpoints arise from the following findings:
-
1.
No RCT exists, and no comparison of a vertebroplasty and a control group has been initiated yet.
-
2.
The setup and documentation of the studies differ from each other.
-
3.
Data collections are often subjective.
-
4.
A direct comparison of the presented studies is only possible regarding the evaluation of pain and complications.
-
5.
Follow-up is often too short; only a few studies examine the long-term results in prospective trials.
-
6.
No standardized study concept exists.
Prospective randomized trials are necessary to control, compare and statistically evaluate the above-mentioned findings. One question still remains: Is there a significant benefit for the patients treated with percutaneous vertebroplasty after a long period of time? Actual results show that it seems to be so. But definite proof will only be given by a randomized controlled trial.
Conclusion
The results of all the evaluated studies show a significant reduction of pain, a minor complication rate and a fast, easy to learn and favorable technique. But considering the above-mentioned arguments, there is no explicit proof in terms of evidence-based medicine that percutaneous vertebroplasty is really better than conservative treatment or other techniques. Especially long-term results regarding the stability of the bone cement and the adjacent vertebrae are still missing.
References
European Prospective Osteoporosis Study (EPOS) (2002) J Bone Miner Res, 17:716–724
Melton LJ, Frye MA, Wahner HW, Riggs BL (1989) Epidemiology of vertebral fractures in women. Am J Epidemiol, 129:1000–1011
Kanis JA. Epidemiology of osteoporosis. Bone 1992; 13 (Suppl. 1):7–15
Ettinger MP. Aging bone and osteoporosis: strategies for preventing fractures in the elderly; Arch Intern Med. 2003 Oct 13; 163(18)2237–2246
McGraw JK, Barr JD, Mathis JM, Sacks D. Society of Interventional Radiology Quality Improvement Guidelines for Percutaneous Vertebroplasty. J Vasc Interv Radiol 2003; 14:827–831
Zoarski GH, Olan WJ, Stallmeyer MJ, Dick BW, Deyne M. Percutaneous vertebroplasty for osteoporotic compression fractures: quantitative prospective evaluation of long-term outcomes. J Vasc Interv Radiol 2002; 13:139–148
Galibert P, Rosat P, Le Gars D. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 1987; 33:166–168
Helmberger T, Hierholzer J, Vorwerk D. Leitlinien der Deutschen Röntgengesellschaft zur Vertebroplastie. Radiologe 2003; 43:703–708
Heini PF. Vertebroplastik bei hochgradiger Osteoporose. Orthopäde 2004; 33:22–29
Gangi A, Dietemann JL. Percutaneous vertebroplasty guided by a combination of CT and fluoroscopy. AJNR 1994; 15:83–86
Alvarez L, Quinones D, Calvo E, Rossi RE. Vertebroplasty in the treatment of vertebral tumors: postprocedural outcome and quality of life. Eur Spine J 2003; 12:356–360
Gangi A, Imbert JP, Marin H, Dietemann JL. Percutaneous vertebroplasty: indications, technique and results. Radiographics 2003; 23:15–15
Pitton MB, Brecher B, Herber S, Mohr W, Thelen M. Evaluation of percutaneous vertebroplasty in osteoporotic vertebral fractures using a combination of CT fluoroscopy and conventional lateral fluoroscopy. RoFo 2004; 176:1005–1012
Gangi A, Dietemann JL. Percutaneous vertebroplasty: a developing standard of care for vertebral compression fractures. AJNR 2001; 22:373–381
Hodler J, Gilula LA. Midterm outcome after vertebroplasty: predicitve value of technical and patient-related factors. Radiology 2003; 227:662–668
Evans AJ, Kip KE, Dunnagan SA. Vertebral compression fractures: pain reduction and improvement in functional mobility after percutaneous vertebroplasty. Radiology 2003; 226:366–372
Deschamps M, Coldman AJ. Assessment of adult cancer pain: shortcomings of current methods. Pain 1988; 32:133–139
Legroux-Gerot I, Boutry N, Cortet B. Long-term follow-up of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Clin Rheumatol 2004; 23:310–317
Winking M, Ortel M, Schnettler R, Böker DK. Treatment of pain from osteoporotic vertebral collapse by percutaneous PMMA vertebroplasty. Acta Neurochir 2004; 146:469–476
Martin JP, Seium Y, Dietrich PY, Ruefenacht DA. Percutaneous vertebroplasty in metastatic disease: transpedicular access and treatment of lysed pedicles-initial experience. Radiology 2003; 229
Martin JB, Sugiu D, Piotin K, Murphy B, Rüfenacht DA. Vertebroplasty: clinical experience and follow-up results. Bone 1999; 25:11S–15S
Winking M, Ortel M, Schnettler R, Böker DK. Polymethylmethacrylat-Vertebroplastie. Dtsch Med Wochenschr 2003; 128:2525–2530
Perez-Higueras A, Rossi RE, Quinones D, Al-Assir I. Percutaneous vertebroplasty: long-term clinical and. Neurorad 2002; 44:950–954
McGraw JK, Minkus KD, Rami PM, Davis TM. Prospective evaluation of pain relief in 100 patients undergoing percutaneous vertebroplasty: results and follow-up. J Vasc Interv Radiol 2002; 13:883–886
Gaughen JR, Schweickert PA, Kaufmann TJ, Kallmes DF. Relevance of antecedent venography in percutaneous vertebroplasty for the treatment of osteoporotic compression fractures. AJNR 2001; 23:594–600
Kallmes DF, Marx WF, Jensen ME. Vertebroplasty in the mid- and upper thoracic spine. AJNR 2002; 23:1117–1120
Peh WCG, Peck DD. Percutaneous vertebroplasty for severe osteoporotic vertebral compression fractures. Radiology 2002; 223:121–126
Kaufmann TJ, Schweickert PA, Marx FW, Kallmes DF. Age of fracture and clinical outcome of percutaneous vertebroplasty. AJNR 2001; 22:1860–1863
Heini PF, Berlemann U. Percutaneous transpedicular vertebroplasty with PMMA. Eur Spine J 2000; 9:445–450
Grados F, Cayrolle G, Hardy N, Deramond H. Long-term observation of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatol 2000; 39:1410–1414
Cyteval C, Roux JO, Thomas E, Taourel P. Acute osteoporotic vertebral collapse. AJR 1999; 173:1685–1690
Cortet B, Voutry N, Flipo RM, Delcambre B. Percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fractures. J Rheumatol 1999; 26:2222
KY Yoo. Acute respiratory distress syndrome associated with pulmonary cement embolism following percutaneous vertebroplasty with polymethylmethacrylate. Spine 2004; 29:294–297
Pleser M, O Worsdorfer, C Manke. [Pulmonary embolism caused by PMMA in percutaneous vertebroplasty Case report and review of the literature.]. Unfallchirurg 2004; 107:807–811
Laredo JD, Hamze B. Complications of percutaneous vertebroplasty and their prevention. Skelet Radiol; 33:493–505
Aaron J. Bone turnover and microdamage. Adv Osteopor Fract Manag 2:102–110
Jensen ME, Mathis JM, Kallmes DF, Cloft HJ, Dion JE. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: technical aspects. AJNR, 18:1897–1904
Kalteis T, Gugler G, Zysk S, Grifka J (2004) Acute tissue toxicity of PMMA bone cements. Z Orthop ;142:666–672
Ciapetti G, Cenni E, Savarino L, Cavedagna D, Pizzoferrato A (2000) Cytotoxic effect of bone cements in HL–60 cells: distinction between apoptosis and necrosis. Biomed Mater Res, 52:338–345
Goodman SB, Song Y, Lee K, Doshi A, Rushdieh B, Woolson S, Maloney W, Schurman D, Sibley R (1997) Loosening and osteolysis of cemented joint arthroplasties. A biologic spectrum. Clin Orthop Relat Res, ; Apr.:149–163
Kallmes DF (2003) Percutaneous vertebroplasty. Radiology, 229:27–36
Kobayashi K, Nakamura K, Murata K (2005) Percutaneous vertebroplasty immediately relieves pain of osteoporotic vertebral compression fractures. Eur Radiol, 15:360–367
Amar AP, Esnaashari N, Lavine SD, Teitelbaum GP (2001) Percutaneous transpedicular PMMA vertebroplasty for the treatment of spinal compression fractures. Neurosurgery, 49:1105–1114
Author information
Authors and Affiliations
Corresponding author
Additional information
K. Hochmuth and D. Proschek contributed equally to this work.
Rights and permissions
About this article
Cite this article
Hochmuth, K., Proschek, D., Schwarz, W. et al. Percutaneous vertebroplasty in the therapy of osteoporotic vertebral compression fractures: a critical review. Eur Radiol 16, 998–1004 (2006). https://doi.org/10.1007/s00330-005-0067-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-005-0067-3