Abstract
The aim of the study is to investigate the levels of serum interleukin-35 (IL-35) before and after treatment and its relationship with clinical parameters as well as the frequency of different subsets of CD4+ T cells in patients with systemic sclerosis (SSc) to explore the role of IL-35 in the pathogenesis of SSc. The levels of serum IL-35, interferon-γ (IFN-γ), IL-4, IL-17A, and IL-10 in 49 patients with SSc and 50 age- and gender-matched healthy subjects were measured by enzyme-linked immunosorbent assay (ELISA). The percentages of peripheral blood Th1, Th2, Th17 cells and Tregs in 49 SSc patients and 20 healthy controls were characterized by flow cytometry. The relationship between the levels of serum IL-35 and the percentages of different subsets of CD4+ T cells, disease duration, the values of forced vital capacity (FVC), modified Rodnan skin scores (MRSS) or high-resolution computed tomography (HRCT) scores was analyzed in patients with SSc. The levels of serum IL-35 in SSc patients were significantly higher than that of healthy controls (P < 0.001), but significantly reduced after treatment for 3 months (P = 0.001). The levels of serum IL-35 were positively correlated with the HRCT scores in SSc patients (P = 0.014) and with disease duration in patients with diffuse cutaneous SSc (P = 0.03), but negatively correlated with the FVC values in SSc patients (P = 0.034). In comparison with that in the healthy controls, significantly decreased percentages of Th1, but increased Th2 and Th17 cells were detected in patients, leading to reduced ratios of Th1/Th2 and increased ratios of Th17/Tregs (P < 0.001). The levels of serum IL-35 were positively correlated with IL-4 (P = 0.036) and tended to be positively associated with the frequency of Tregs in SSc patients (P = 0.054). Higher levels of serum IL-35 may be associated with the development of SSc and severity of pulmonary fibrosis in SSc patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic sclerosis (SSc) is a chronic systemic autoimmune disease and is characterized by vasculopathy, inflammation, and fibrosis, particularly in the skin and lung [1]. SSc is categorized based on the extent of skin involvement into limited cutaneous SSc (lcSSc) and diffuse cutaneous SSc (dcSSc). The prevalence of SSc is 88–489/million people, and its incidence tends to be increasing in the world [2]. Currently, the pathogenic process of SSc is unclear.
Interleukin (IL)-35 is a heterodimeric and inhibitory cytokine, composed of IL-12 subunit alpha (P35) and Epstein–Barr virus-induced gene 3 (EBI3) [3]. A previous study has shown that IL-35 is predominantly secreted by regulatory T cells (Tregs) and CD8α+ dendritic cells, and IL-35 can inhibit the activation and functional differentiation of effector T cells, such as IL-17A+ Th17 cells and others, but promotes the expansion of Tregs [10]. IL-35 has been considered as a therapeutic reagent for autoimmune disease [4]. A previous study has shown that elevated levels of serum IL-35 in patients with SSc are associated with inflammation at early stages of disease process and skin dermal fibroblasts. Furthermore, transforming growth factor beta 1 (TGF-β1), a potent inducer of fibrosis, can induce IL-35 expression, which in turn activates resting fibroblasts and enhances the release of collagen in SSc [5]. However, it is unclear how the levels of serum IL-35 are associated with the severity of pulmonary fibrosis and disease duration in patients with SSc. There is no information on the dynamic changes in the levels of serum IL-35 in patients with SSc following standard therapies.
The balance between pro-inflammatory T cells and Tregs as well as their produced cytokines is crucial for the pathogenesis of SSc. Th1 cells and their secreted interferon gamma (INF-γ) are powerful anti-fibrosis factors [6]. Th17 cells can secrete IL-17A, IL-21 and IL-22, and promote inflammation, resulting in the development and progression of autoimmune diseases [8]. In contrast, Th2 cells and their produced IL-4 and IL-13 can promote collagen synthesis and fibrosis [7]. Tregs can produce IL-10 and TGF-β1, which are essential for maintaining self-tolerance and preventing autoimmunity [9]. However, the frequency of different subsets of CD4+ T cells and the relationship between the levels of serum IL-35 and IFN-γ, IL-4, IL-17A or IL-10 as well as the percentages of each subset of CD4+ T cells in patients with SSc have not been clarified.
This study was aimed at examining the levels of serum IL-35 in SSc patients before and after standard therapies as well as in age- and gender-matched healthy subjects and determining the frequency of different subsets of CD4+ T cells and their serum representative cytokine levels. Furthermore, we explored the relationship between the levels of serum IL-35 and disease severity, duration, the percentages of different subsets of CD4+ T cells and their serum cytokines in patients with SSc to explore the potential role of IL-35 in the development of SSc.
Materials and methods
Clinical data
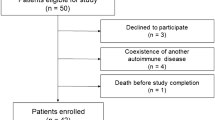
A total of 49 patients with SSc were recruited at the inpatient service of the Department of Rheumatology in the First Affiliated Hospital of Guangxi Medical University from June 2014 to June 2016. Individual patients with SSc were newly diagnosed by the criteria of American College of Rheumatology (ACR)/European league against rheumatism (EULAR) [11]. Patients were classified as lcSSc (n = 20) or dcSSc (n = 29), according to the 2013 classification criteria for SSc. The disease duration of patients was defined from the onset time of the first non-Raynaud event to enrollment time [12]. Those patients did not receive any treatment of corticosteroids and immunosuppressive drugs during baseline measurement. Individual patients were excluded if she/he had currently infectious disease or a seriously chronic disease in the respiratory, cardiovascular, nervous, endocrine, blood system, liver, kidney disease or malignant tumors. Fifty age- and gender-matched healthy individuals were recruited as the controls. Their demographic, clinical and laboratory characteristics are summarized in Table 1. The experimental protocol was approved by the Ethical Committee of the First Affiliated Hospital of Guangxi Medical University. Written informed consent was obtained from all subjects.
Treatment
All patients were treated with glucocorticoids and/or immunosuppressants for 3 months. A total of 34 patients were treated with both glucocorticoids (5–40 mg/day) and immunosuppressants, 12 with immunosuppressants alone, and 3 with glucocorticoids alone. Most patients received small and medium doses of prednisone, and the patients with severe interstitial lung disease were treated with 30–40 mg/day of prednisone. According to their disease condition, some patients were treated by a combination therapy with two immunosuppressants. There were 28 patients, who were treated with cyclophosphamide (1 g, every 4 weeks), 4 with azathioprine (100 mg/day), 3 with cyclosporine (50 mg, tid), 11 with methotrexate (10–15 mg, weekly), 3 with leflunomide (20 mg/day), 8 with thalidomide (50–75 mg/day), 4 with mycophenolate mofetil (75 mg, bid), and 3 with tripterygium glycosides (50 mg, tid). The specific drug delivery methods and dosage of the immunosuppressants in the whole process of disease treatment were individualized, according to the patients’ condition. There was no renal crisis in any patient during the observation period.
The pulmonary function test
All patients had undergone pulmonary function tests which were completed by specialists in the pulmonary function testing section of our hospital. The forced vital capacity (FVC) values were recorded at baseline and after therapy.
The modified Rodnan skin score (MRSS)
The skin thickness of individual patients was measured by the MRSS [13]. The skin thickness of 17 body sites was measured by palpation of two physicians in a blinded manner and rated on a scale of 0–3 as 0 (normal), 1 (mild), 2 (moderate) or 3 (severe skin thickening), leading to a total skin score of 0–51 [14].
Chest high-resolution CT (HRCT) score
The severity of pulmonary fibrosis in individual patients was tested by HRCT and scored as described previously [15]. Briefly, each lung was divided into three zones of the upper (lung apex to aortic arch), middle (aortic arch to inferior pulmonary veins), and lower (inferior pulmonary veins to lung bases). The extent of pulmonary abnormality in each of six zones in individual patients was scored using a scale from 0 to 4, as 0, absent; 1, 1–25%; 2, 26–50%; 3, 51–75%; and 4, 76–100%. The degrees of pulmonary fibrosis were defined as the pure ground-glass opacity (pGGO), pulmonary fibrosis (PF) or honeycomb cysts (HCs). The change in the extent of pulmonary abnormality in each of the six zones was scored by HRCT during the followed up period. The HRCT images were scored by two radiologists in a blinded manner.
Flow cytometry
Peripheral blood samples were collected from 49 SSc patients and 20 healthy controls and peripheral blood mononuclear cells (PBMCs) were isolated by density-gradient centrifugation using Ficoll-Hypaque (Pharmacia, Uppsala, Sweden). The PBMCs (106/tube) were stimulated with 25 ng/ml of phorbol-12-myristate-13-acetate (PMA, Sigma) and 1 µg/ml of ionomycin (Sigma) at 37 °C for 1 h and cultured in the presence of 10 µg/ml of brefeldin (BFA, Sigma) for another 4 h. The cells were stained with ALEXA 488-anti-CD4 (BD PharMingen), fixed, permeabilized and stained with PE-anti-IL-17A, APC-anti-INF-γ, PerCP-anti-IL-4 (BD PharMingen). The percentages of CD4+IL-17A+ Th17, CD4+INF-γ+ Th1 and CD4+IL-4+ Th2 cells were determined by flow cytometry on a BD FACSCalibur (Beckman Coulter; BD Biosciences). The data were analyzed using FCS ExpressV4 software (lenovo, Toronto, ON, Canada). In addition, CD4+ T cells were purified by negative selection and stained with ALEXA 488-anti-CD4, PE-CY7-anti-CD25 (BD PharMingen). The cells were fixed, permeabilized using the permeabilization kit (Caltag Laboratories) and stained with ALEXA647-anti-FoxP3 (eBioscience, USA). The percentages of CD4+ CD25+ Foxp3+ Tregs were determined by flow cytometry.
Enzyme-linked immunosorbent assay (ELISA)
Peripheral blood samples were collected from 49 individual patients before and after 3-month treatment and their serum samples were prepared. Similarly, serum samples were prepared from 50 individual healthy subjects. All serum samples were stored at − 80 °C. The concentrations of serum IL-35, IL-4, IL-17A, INF-γ and IL-10 in SSc patients and healthy controls were measured by ELISA using cytokine-specific kits (R&D Systems, Minneapolis, MN, USA), according to the manufacturer’s protocols. All samples were assayed in triplicates.
Statistical analysis
Data were analyzed with the SPSS statistical software version 22 (SPSS, Chicago, USA). Category data are summarized as counts and percentage. Quantitative data are expressed as the mean ± standard deviation or median and quartile range according to their distribution. The difference between groups was determined by Student’s t test or Mann–Whitney U test. The relationship between measures was analyzed by Pearson correlation or Spearman’s rank correlation. A two-tailed P value of < 0.05 was considered statistically significant.
Result
The levels of serum IL-35 in patients with SSc before and after treatment
To explore the potential role of IL-35 in the development of SSc, 49 patients with SSc and 50 age- and gender-matched healthy subjects were recruited. As expected, those patients had varying levels of skin thicknesses (100%), pulmonary abnormalities (93.88%), bone/joint involvements (12.24%), clinical gastrointestinal manifestations (57.14%), heart involvements (6.12%), kidney involvements (14.29%) and hypothyroidism (20.41%, Fig. 1c; Table 1). Moreover, most patients developed anti-ANA and anti-Scl-70 autoantibodies, particularly for those with diffuse cutaneous systemic sclerosis (dcSSc, Table 1). ELISA indicated the levels of serum IL-35 in patients with SSc were significantly higher than that of healthy controls (P < 0.001, Fig. 1a), but there was no significant difference in the levels of serum IL-35 between the patients with dcSSc and lcSSc (P = 0.462). Furthermore, the levels of serum IL-35 in patients with SSc were positively correlated with chest HRCT scores (rho = 0.350, P = 0.014), but not significantly with the values of MRSS (rho = − 0.124, P = 0.396, Fig. 2). And the levels of serum IL-35 in patients with SSc were negatively correlated with the FVC values (rho = − 0.303, P = 0.034, Fig. 2). In addition, the levels of serum IL-35 in patients with dcSSc were positively correlated with the disease duration in patients with dcSSc (rho = 0.3534, P = 0.030), but not in those with lcSSc (Fig. 1b). After standard treatment for 3 months, the levels of serum IL-35 in those patients were significantly reduced (P = 0.001) and were similar to that of the healthy controls (Fig. 1a). Hence, high levels of IL-35 were associated with the development and severity of SSc in human patients and significantly reduced after standard therapies.
The levels of serum IL-35 in individual patients and age- and gender-matched healthy subjects were determined by ELISA. Following treatment with standard therapies, the levels of serum IL-35 were tested. Data are expressed as the mean values of individual subjects (n = 49 for patients; n = 50 for healthy controls) from three separate experiments. The relationship between the levels of serum IL-35 and the disease duration in patients with SSc was analyzed by Spearman’s rank correlation. a The levels of serum IL-35. b The levels of serum IL-35 were positively correlation with the disease duration in dcSSc patients, but not in lcSSc patients. c The organ involvement in 49 SSc patients
The relationships between the levels of serum IL-35 and the values of HRCT, MRSS or FVC in patients with SSc were analyzed by Spearman’s rank correlation. The HRCT scores were used to evaluate the degrees of pulmonary fibrosis. The MRSS values were used to evaluate the degrees of skin sclerosis. The FVC values were used to evaluate the pulmonary function (n = 49 for patients)
The frequency of different subsets of CD4+ T cells in patients with SSc
Next, we characterized the frequency of different subsets of CD4+ T cells from 49 SSc patients and 20 healthy individuals by flow cytometry. As shown in Fig. 3, the percentages of CD4+ INF-γ+ Th1 cells in patients SSC were significantly lower than that of healthy control (7.16 ± 2.09 vs.12.23 ± 4.64, P < 0.001) while the percentages of CD4+ IL-4+ Th2 (5.38 ± 1.82 vs. 2.47 ± 0.89, P < 0.001) and CD4+ IL-17A+ Th17 (1.66 ± 0.80 vs. 0.93 ± 0.28, P < 0.001) in patients with SSC were significantly higher than that of healthy controls. However, there was similar percentages of CD4+ CD25+ Foxp3+ Tregs between the patients and healthy controls (3.90 ± 1.07 vs. 3.56 ± 0.97, P = 0.224). As a result, the ratios of Th1 to Th2 in patients with SSc were significantly lower than that of healthy controls while the ratios of Th17 to Tregs were significantly higher than that of healthy controls. Apparently, higher frequency of Th2 and Th17 cells were associated with the development of SSc in human patients.
The frequency of different subsets of CD4+ T cells in 49 SSc patients and 20 controls. The percentages of Th1, Th2, Th17 cells and Tregs in individual patients and healthy subjects were determined by flow cytometry. The ratios of Th1 to Th2 or Th17 to Tregs were calculated. Data are expressed as the mean ± SD of each group from several experiments. (n = 49 for patients; n = 20 for healthy controls)
The relationship between the levels of serum IL-35 and the percentages of different subsets of CD4+ T cells in SSc patients
To further clarify the role of IL-35 in SSc, we studied the relationship between the levels of serum IL-35 and the percentages of different subsets of CD4+ T cells in patients with SSc. There was a tendency that the levels of serum IL-35 were positively associated with the percentages of Treg cells (r = 0.277, P = 0.054), but negatively associated with the percentages of Th1 cells (r = − 0.255, P = 0.121, Fig. 4). These data support the notion that IL-35 is predominantly secreted by Tregs.
The relationship between the levels of serum IL-35 and the percentages of different subsets of CD4+ T cells in patients with SSc. The relationship between the levels of serum IL-35 and the percentages of Th1, Th2, Th17, Tregs, the ratios of Th1 to Th2 or Th17 to Tregs was analyzed by Pearson correlation. Data are individual values (n = 49)
The relationship between the levels of serum IL-35 and other cytokines tested in patients with SSc
To further shed light on the potential role of IL-35 in SSc, we studied the correlation between the levels of serum IL-35 and other cytokines tested in patients with SSc. We found that the levels of serum IL-35 were positively correlated with the levels of serum of IL-4 (r = 0.301, P = 0.036, Fig. 5), but not significantly with other cytokines tested in patients with SSc. These, together with higher frequency of Th2 cells, suggest that both IL-35 and Th2 responses may contribute to the development of SSc in human patients.
Discussion
In this study, we found significantly higher levels of serum IL-35, higher frequency of Th2 and Th17 cells, but decreased percentages of Th1 cells and the ratios of Th1 to Th2 cells in SSc patients, relative to that in the healthy controls. The increased levels of serum IL-35 in SSc patients were similar to a previous study [3]. The decreased ratios of Th1 and Th2 cells, together increased frequency of peripheral blood Th17 cells, were consistent with previous reports [18, 19]. These findings support the notion that dysregulated T cell responses and their produced cytokines are crucial for the pathogenesis of SSc [16]. However, our data were in disagreement with another report that higher levels of pro-inflammatory cytokine production in SSc patients [17]. The difference may stem from different populations of patients at varying stages of disease process. More importantly, the levels of serum IL-35 were positively correlated with chest HRCT scores in SSc patients and disease duration in dcSSc patients, but negatively correlated with FVC values in SSc patients. Hence, the levels of serum IL-35 may be valuable for evaluating the severity of pulmonary fibrosis in SSc patients.
IL-35 is an anti-inflammatory cytokine and is mainly produced by CD4+ CD25+ Foxp3+ Tregs [25]. IL-35 binds to its receptors to positive feedback promote its own expression. Functionally, IL-35 can inhibit immune responses, but promote the expansion of Tregs [26]. We detected higher levels of serum IL-35 in patients with SSc, but significantly reduced after 3-month therapies. Importantly, the levels of serum IL-35 were positively correlated with chest HRCT scores in SSc patients and disease duration in dcSSc patients. Given that IL-35 has been reported to regulate collagen expression [5], it is possible that IL-35 may participate in the pathogenesis of SSc. Alternatively, the higher levels of serum IL-35 may reflect compensatory anti-inflammatory responses to inhibit Th17, Th2 and Th1 responses during the development and progression of SSc.
In this study, we also found that the levels of serum IL-35 had a tendency to be positively correlated with the frequency of Treg cells in SSc patients, which supports the notion that IL-35 is mainly secreted by Tregs. In addition, a previous study has shown higher frequency of peripheral blood Tregs in patients with a high interstitial lung disease (ILD) score on computed tomography than those with normal ILD scores [1]. Our previous study has also found that the percentages of peripheral blood Tregs in patients with SSc are positively correlated with the chest HRCT scores. It is notable that Tregs can secrete TGF-β1, and Treg infiltrates in the skin can secrete Th2-like cytokines, such as IL-4 and IL-13 as well as some chemokines [28]. Actually, increased levels of IL-4 expression are detected in plasma and the skin of SSc patients [29,30,31]. We also found that higher levels of serum IL-35 were correlated positively with the levels of serum IL-4 in SSc patients. Therefore, IL-35, together other molecules from Tregs, may contribute to the process of fibrosis.
In conclusion, our data indicated significantly higher levels of serum IL-35, higher frequency of Th2 and Th17 cells, but decreased percentages of Th1 cells and the ratios of Th1 to Th2 cells in SSc patients. The levels of serum IL-35 were positively correlated with the chest HRCT scores in SSc patients and disease duration in dcSSc patients, but negatively correlated with the FVC values in SSc patients, and significantly reduced after 3-month therapies. Furthermore, the levels of serum IL-35 had a tendency to be associated with the percentages of peripheral blood of Tregs in SSc patients. Hence, IL-35, together with Th2 cytokines and other molecules secreted from Tregs, may contribute to the pathogenesis of fibrosis during the development of SSc and the levels of serum IL-35 may be valuable for evaluating the severity of pulmonary fibrosis in SSc patients. However, we recognized that our study did not include a disease control group of patients with idiopathic ILD. We are interested in further exploring this field in the future.
References
Jiang N, Li M, Zeng X (2014) Correlation of Th17 cells and CD4+ CD25+ regulatory T cells with clinical parameters in patients with systemic sclerosis. Chin Med J 127(20):3557–3561
Chifflot H, Fautrel B, Sordet C, Chatelus E, Sibilia J (2008) Incidence and prevalence of systemic sclerosis: a systematic literature review. Semin Arthritis Rheum 37(4):223–235
Dantas AT, Goncalves SM, Pereira MC, Goncalves RS, Marques CD, Rego MJ, Pitta IR, Duarte AL, Pitta MG (2015) Increased IL-35 serum levels in systemic sclerosis and association with pulmonary interstitial involvement. Clin Rheumatol 34(9):1621–1625
Guan SY, Leng RX, Khan MI, Qureshi H, Li XP, Ye DQ, Pan HF (2017) Interleukin-35: a potential therapeutic agent for autoimmune diseases. Inflammation 40(1):303–310
Tomcik M, Zerr P, Palumbo-Zerr K, Storkanova H, Hulejova H, Spiritovic M, Kodet O et al (2015) Interleukin-35 is upregulated in systemic sclerosis and its serum levels are associated with early disease. Rheumatology 54(12):2273–2282
Fletcher JM, Lalor SJ, Sweeney CM, Tubridy N, Mills KH (2010) T cells in multiple sclerosis and experimental autoimmune encephalomyelitis. Clin Exp Immunol 162(1):1–11
Chizzolini C, Parel Y, De Luca C, Tyndall A, Akesson A, Scheja A, Dayer JM (2003) Systemic sclerosis Th2 cells inhibit collagen production by dermal fibroblasts via membrane-associated tumor necrosis factor alpha. Arthritis Rheum 48(9):2593–2604
Hu D, Notarbartolo S, Croonenborghs T, Patel B, Cialic R et al (2017) Transcriptional signature of human pro-inflammatory TH17 cells identifies reduced IL10 gene expression in multiple sclerosis. Nat Commun 8(1):1600
Fenoglio D, Battaglia F, Parodi A, Stringara S, Negrini S, Panico N, Rizzi M, Kalli F, Conteduca G et al (2011) Alteration of Th17 and Treg cell subpopulations co-exist in patients affected with systemic sclerosis. Clin Immunol 139(3):249–257
Collison LW, Chaturvedi V, Henderson AL, Giacomin PR, Guy C, Bankoti J, Finkelstein D, Forbes K, Workman CJ et al (2010) IL-35-mediated induction of a potent regulatory T cell population. Nat Immunol 11(12):1093–1101
van den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, Tyndall A, Matucci-Cerinic M et al (2013) 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League against rheumatism collaborative initiative. Arthritis Rheum 65(11):2737–2747
Cutolo M, Smith V, Furst DE, Khanna D, Herrick AL (2017) Points to consider-Raynaud’s phenomenon in systemic sclerosis. Rheumatology 56(Suppl 5):v45–v48
Khanna D, Furst DE, Clements PJ, Allanore Y, Baron M, Czirjak L, Distler O et al (2017) Standardization of the modified Rodnan skin score for use in clinical trials of systemic sclerosis. J Scleroderma Relat Disord 2(1):11–18
Kumánovics G, Péntek M, Bae S, Opris D, Khanna D, Furst DE, Czirják L (2017) Assessment of skin involvement in systemic sclerosis. Rheumatology 56(Suppl 5):v53–v66
Goldin JG, Lynch DA, Strollo DC, Suh RD, Schraufnagel DE, Clements PJ, Elashoff RM, Furst DE et al (2008) High-resolution CT scan findings in patients with symptomatic scleroderma-related interstitial lung disease. Chest 134(2):358–367
Denton CP, Khanna D (2017) Systemic sclerosis. Lancet 390(10103):1685–1699
Antonelli A, Ferri C, Fallahi P, Colaci M, Giuggioli D, Ferrari SM, Frascerra S, Franzoni F, Galetta F, Ferrannini E (2008) Th1 and Th2 chemokine serum levels in systemic sclerosis in the presence or absence of autoimmune thyroiditis. J Rheumatol 35(9):1809–1811
Fujii H, Hasegawa M, Takehara K, Mukaida N, Sato S (2002) Abnormal expression of intracellular cytokines and chemokine receptors in peripheral blood T lymphocytes from patients with systemic sclerosis. Clin Exp Immunol 130(3):548–556
Baraut J, Farge D, Jean-Louis F, Kesmandt H, Durant C, Verrecchia F, Michel L (2012) Cytokines in systemic sclerosis. Pathol Biol (Paris) 60(2):127–139
Cordiali-Fei P, Mussi A, D'Agosto G, Trento E, Bordignon V, Trincone S, Vento A, Sperduti I, Cristaudo A, Ensoli F (2013) Assessment of T regulatory cells and expanded profiling of autoantibodies may offer novel biomarkers for the clinical management of systemic sclerosis and undifferentiated connective tissue disease. Clin Dev Immunol 2013:390563
Lei L, Zhao C, Qin F, He ZY, Wang X, Zhong XN (2016) Th17 cells and IL-17 promote the skin and lung inflammation and fibrosis process in a bleomycin-induced murine model of systemic sclerosis. Clin Exp Rheumatol 100(5):14–22
Rodriguez-Reyna TS, Furuzawa-Carballeda J, Cabiedes J, Fajardo-Hermosillo LD, Martinez-Reyes C, Díaz-Zamudio M, Llorente L (2012) Th17 peripheral cells are increased in diffuse cutaneous systemic sclerosis compared with limited illness: a cross-sectional study. Rheumatol Int 32(9):2653–2660
Kurasawa K, Hirose K, Sano H, Endo H, Shinkai H, Nawata Y, Takabayashi K, Iwamoto I (2000) Increased interleukin-17 production in patients with systemic sclerosis. Arthritis Rheum 43(11):2455–2463
Andersen GN, Nilsson K, Nagaeva O, Rantapää-Dahlqvist S, Sandström T, Mincheva-Nilsson L (2011) Cytokine mRNA profile of alveolar T lymphocytes and macrophages in patients with systemic sclerosis suggests a local Tr1 response. Scand J Immunol 74(3):272–281
Collison LW, Workman CJ, Kuo TT, Boyd K, Wang Y, Vignali KM, Cross R, Sehy D, Blumberg RS, Vignali DA (2007) The inhibitory cytokine IL-35 contributes to regulatory T-cell function. Nature 450(7169):566–569
Niedbala W, Wei XQ, Cai B, Hueber AJ, Leung BP, McInnes IB, Liew FY (2007) IL-35 is a novel cytokine with therapeutic effects against collagen-induced arthritis through the expansion of regulatory T cells and suppression of Th17 cells. Eur J Immunol 37(11):3021–3029
Kudo H, Wang Z, Jinnin M, Nakayama W, Inoue K, Honda N, Nakashima T et al (2015) EBI3 downregulation contributes to type I collagen overexpression in scleroderma skin. J Immunol 195(8):3565–3573
MacDonald KG, Dawson NA, Huang Q, Dunne JV, Levings MK, Broady R (2015) Regulatory T cells produce profibrotic cytokines in the skin of patients with systemic sclerosis. J Allergy Clin Immunol 135(4):946–949
Kanellakis P, Ditiatkovski M, Kostolias G, Bobik A (2012) A pro-fibrotic role for interleukin-4 in cardiac pressure overload. Cardiovasc Res 95(1):77–85
Parel Y, Aurrand-Lions M, Scheja A, Dayer JM, Roosnek E, Chizzolini C (2007) Presence of CD4+ CD8+ double-positive T cells with very high interleukin-4 production potential in lesional skin of patients with systemic sclerosis. Arthritis Rheum 56(10):3459–3467
Furue M, Mitoma C, Mitoma H, Tsuji G, Chiba T, Nakahara T, Uchi H, Kadono T (2017) Pathogenesis of systemic sclerosis—current concept and emerging treatments. Immunol Res 65(4):790–797
Acknowledgements
The authors would like to express their appreciation to Professor Jia-Quan Li, Guangxi Medical University, for his assistance and advice in performing experiments. This manuscript has been edited and proofread by Medjaden Bioscience Limited.
Funding
This study was supported by grants from the Guangxi Natural Science Foundation (Grant No. 2016GXNSFAA380175).
Author information
Authors and Affiliations
Contributions
Jie Tang carried out the experiments, data collection and interpretation and writing the manuscript. Ling Lei designed the study, analyzed and interpreted the data, reviewed the manuscript, and supervised the entire study. Jie Pan helped to perform experiments and data acquisition. Cheng Zhao and Jing Wen participated in data collection and analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethical Committee of the First Affiliated Hospital of GuangXi Medical University. Written informed consent was obtained from all patients and healthy controls.
Conflict of interest
All authors have no conflict of interest to declare. There is no any interest or relationship with pharmaceutical agencies within the past 36 months.
Rights and permissions
About this article
Cite this article
Tang, J., Lei, L., Pan, J. et al. Higher levels of serum interleukin-35 are associated with the severity of pulmonary fibrosis and Th2 responses in patients with systemic sclerosis. Rheumatol Int 38, 1511–1519 (2018). https://doi.org/10.1007/s00296-018-4071-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-018-4071-8