Abstract
Predictive factors of response to hypomethylating agents (HMA) in elderly acute myeloid leukemia (AML) patients remain unclear in the real-life setting and no direct comparison between azacitidine (AZA) and decitabine (DEC) has been carried out. We retrospectively evaluated 110 AML patients treated with HMA (78 AZA, 32 DEC) as first-line therapy outside of clinical trials. Median age was 75 years (range 58–87). The median overall survival (OS) of the entire cohort was 8.0 months (95% CI 6.1–10), without significant differences among the subgroups: AZA 8.8 months vs DEC 6.3 months (p = 0.291). HMA treatment yielded an overall response rate (ORR) of 40% (AZA 37% vs DEC 47%, p = 0.237). A stable disease (SD) after 4 HMA cycles was not associated with a worse survival outcome compared with an early optimal response. Factors independently associated with a better OS were transfusion independence during treatment (p = 0.049), achievement of an optimal response to treatment (p < 0.001), and a baseline hemoglobin level ≥ 9.25 (p = 0.018). A bone marrow (BM) blast count ≥ 30% (p < 0.001) and a therapy-related AML (p = 0.008) remain poor survival predictors. Of the available biologic features, an adverse risk category according to the ELN classification was significantly associated with a shorter survival over the intermediate risk category (p = 0.034). Disease progression remains the primary cause of death. Infectious complications were more severe (p = 0.036) and occurred earlier (p = 0.006) in the DEC group compared with that of the AZA group. In conclusion, clinical prognostic factors associated to response and survival have been identified without significant associations concerning overall outcomes between the two HMAs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myeloid leukemia (AML) is the most common form of acute leukemia in adults and is characterized by a clinically and biologically heterogeneous disease [1]. According to the most recent data from the NCI’s Surveillance, Epidemiology and End Results (SEER) program, the median age at diagnosis is 68 years. More than half of new cases of AML is > 50 years, and about one-third is aged > 75 [2]. The prognosis of elderly AML patients remains poor despite an improved understanding of the genetic landscape of AML and the recent therapeutic advances. Indeed, the estimated 2-year survival rate of patients aged ≥ 65 is less than 20% [3]. In this subset, an adverse cytogenetic karyotype, other biologic features, and clinical risk factors (comorbidities, polypharmacy, poor performance status (PS), cognitive decline) contribute to a poor chemotherapy tolerance and make the AML management a therapeutic challenge [4, 5]. Hypomethylating agents (HMA), such as 5-azacitidine (AZA) or 5-aza-2 deoxycitidine (decitabine, DEC), capable of inhibiting DNA methyltransferases and resulting in the re-expression of key genes critical to growth, differentiation, angiogenesis, signaling, and DNA repair, represent a widely accepted standard of care for AML patients ineligible to intensive chemotherapy [6,7,8]. A subgroup analysis of the AZA-MDS-001 trial highlighted a survival benefit for low blast count AML patients treated with AZA compared with conventional care [9, 10]. Similarly, the randomized phase III trial AZA-AML-001, which enrolled elderly AML patients with a bone marrow blast count > 30%, confirmed the superiority of AZA over conventional therapy (CT) in terms of median overall survival (OS) (12.1 months vs 6.9 months respectively, p = 0.0190). Furthermore, AZA reduced significantly the rates and days of hospitalization for treatment-related adverse events compared with the control arm [11]. A second survival analysis of DACO-016, the pivotal study that compared the efficacy and safety of DEC with investigators choice, demonstrated the benefit of DEC in intermediate–high-risk AML elderly patients [12]. Although HMA seem to be a safe treatment strategy, long-lasting responses are rare [13]. Moreover, predictors of response to HMA are still poorly defined, and no clear recommendations have been published that suggest how to select the appropriate HMA for each patient. A direct comparison of the two HMA has so far not been carried out, and it is difficult to indirectly compare the two trials due to the differences in inclusion criteria, median number of administered cycles, and control arm treatment. Real-life comparisons between the two HMA are scarce. For these reasons, our study was aimed at identifying possible predictors of response to these agents and at investigating the differences in survival, clinical response, and safety profile between AZA and DEC in a consecutive cohort of elderly AML patients treated in the real-life setting.
Patients and methods
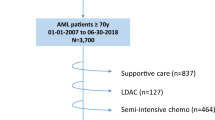
We retrospectively analyzed 110 consecutive elderly AML patients who received HMA as first-line treatment outside of clinical trials at a single institution between August 2007 and July 2019. Seventy-eight patients received subcutaneous AZA 75 mg/m2 for 7 days according to the 5 + 2 + 2 schedule every 4 weeks and 32 patients received intravenous DEC 20 mg/m2 for 5 consecutive days every 4 weeks until disease progression or unacceptable toxicity.
We excluded patients who received HMA as a second-line or salvage therapy after an allogeneic stem cell transplant. The diagnosis of AML was carried out according to the WHO 2016 criteria [14]. Clinical data collected include both disease-related (bone marrow blast count, blood count values, cytogenetics, and biologic features at the onset of the disease) and patient-related (age, comorbidity, renal function) characteristics. The Charlson comorbidity index (CCI) [15] was used as an indicator of comorbidity, and the estimated glomerular filtration rate (eGFR) was calculated through the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [16] for all patients. Data about transfusion requirement during treatment in terms of number of transfusions per cycle was also collected.
The European LeukemiaNet (ELN) recommendations [17] have been used to stratify patients on the basis of the genetic risk profile and to evaluate the degree of response to treatment. The severity of infection complications has been established according to the Common Terminology Criteria for Adverse Events version 5.0 (CTCAE) [18].
Statistical analyses were carried out on the entire patient population and according to the type of HMA used. Differences in the study groups concerning characteristics and treatment responses were estimated using the chi-square test or the Fisher exact test for categorical covariates and the Mann-Whitney U test for continuous variables. OS was calculated from the start of therapy to death from any cause or the date of the last follow-up. Progression-free survival (PFS) was instead calculated from the start of therapy to the date of progression of the disease (PD) or death due to any cause. Probabilities of OS and PFS were estimated using the Kaplan-Meier analysis and compared using the log-rank test. The cut-off of variables used for survival analysis was selected according to the median values for hemoglobin (Hb) level, platelet count, and age in years.
All p values < 0.05 have been considered statistically significant. The possible impact on survival of significant variables found at univariate analysis has been re-examined using the Cox Regression model for multivariate analysis; logistic regression was applied to assess factors associated with optimal treatment response. All statistical analyses were performed using the IBM SPSS Statistics, version 25.
Results
Characteristics of patients
Baseline patients’ characteristics are listed in Table 1. Median age was 75 years (range 58–87). The 57% of patients aged more than the median age at diagnosis. Sixty-two patients (56%) had de novo AML and 44 (40%) had secondary AML (s-AML), while only 4 patients had a therapy-related AML (t-AML). The median white blood cell count (WBC) was 2.57 × 109/L (range 0.37–83.47). Sixty-six out of 110 patients (60%) had ≥ 30% blasts in the bone marrow (BM), and the mean BM blast count was 33% (range 20–90%). Cytogenetics was available for 75 patients. Seven out of 75 patients (9%) carried a complex karyotype, and 4 (5%) had a monosomal karyotype (MK); the other cytogenetic features are shown in Table 1. One out of 4 t-AML had a complex karyotype. A genetic risk assessment, according to the ELN recommendation, has been possible for 38 of the 110 patients (35%): 21 patients had an intermediate risk and 13 an adverse risk, while only 4 patients were considered to have a favorable risk. The majority of patients (93%) had a CCI ≥ 3. At baseline, the median creatinine level was 0.9 mg/dL (range 0.3–10.8) and the eGFR 73 mL/min/1.73m2 (range 4–112). At the time of diagnosis, only 1 patient was affected by end-stage kidney disease and was undergoing hemodialysis.
No notable differences regarding disease characteristics and demographic data were found among patients divided according to the type of HMA received, except for the median BM blasts count that was significantly higher for DEC patients (DEC 59% vs AZA 29%, p < 0.001), as shown in Table 1.
Response to treatment
Sixty-eight out of the 110 patients (62%) received at least 4 cycles of HMA (50 in the AZA cohort and 18 for the DEC cohort, p = 0.59). The evaluation of response after the fourth cycle was available for 66 of the 68 patients: 8 complete remissions (CR, 12%), 18 CRs with incomplete hematologic recovery (CRi, 27%), 11 partial remissions (PR, 17%), and 21 stable diseases (SD, 32%) were recorded. The remaining 8 patients (12%) experienced a PD. Two patients in the DEC group underwent an allogeneic stem cell transplant after 5 and 6 cycles of therapy, respectively.
Overall, considering the best responses obtained across the entire treatment period, 44 of the 110 patients (40%) witnessed a response, including 11 (25%) CR, 24 (55%) CRi, and 9 (20%) PR, after a median time of 3.9 months (range 0.8–12.3). The overall response rate (ORR) was not statistically different between AZA- and DEC-treated patients (37% vs 47%, respectively, p = 0.237; Fig. 1)
In univariate analysis, the variables significantly associated with the achievement of a CR/CRi/PR for the entire population were a platelet count ≥ 79.5 × 109/L (p < 0.001), no requirement of red blood cell transfusions (RBC-T) during treatment (p = 0.001) and a baseline eGFR ≥ 60 mL/min/1.73m2 (p = 0.005). No requirement of RBC-T remained significant in the sub-analysis of the AZA group (p = 0.001), while the eGFR value carried statistical significance in the DEC group (p = 0.011). All factors maintained their significance in multivariate testing, even though with a wide confidence interval, probably due to the low number of patients (data not shown).
Overall survival
The median OS of all patients was 8.0 months (95% CI 6.1–10.0) (Fig. 2). The survival probabilities at 1 year and 2 years were 35.2% and 18.3%, respectively. No differences in terms of median OS were recorded according to the HMA treatment (AZA 8.8 months vs DAC 6.3 months, p = 0.291, Fig. 3).
At univariate analysis, a Hb ≥ 9.25 g/dL at baseline (p = 0.013), a BM blast count < 30% (p = 0.001), all subtypes except t-AML (p = 0.001), a baseline eGFR ≥ 60 mL/min/1.73m2 (p = 0.011), the achievement of a CR/CRi/PR as best response (p < 0.001), and RBC and platelet-transfusion independence during treatment (p < 0.001) were significantly associated with a better OS for the whole cohort (Table 2). Adverse risk category patients had a significantly shorter median OS than intermediate-risk patients: 5.7 months vs 18 months (p = 0.034). No differences in terms of OS were associated with age, WBC count, CCI, and cytogenetic characteristics. Based on the ELN response criteria, patients with a SD after the fourth HMA cycle did not show a significantly shorter survival compared with patients who had achieved at a PR or more (p = 0.312), showing instead a clear advantage in OS compared with patients who did not achieve a response (p < 0.001, Fig. 4, Suppl. Fig. 1). Patients obtaining CR had longer, although not statistically significant, median survival compared with those who achieved CRi, PR, and SD after the fourth cycle (28.1 months (95% CI 9.2–47.0) vs 14.7 months (95% CI 7.4–22.0), p = 0.136). The achievement of a SD as the best response during HMA treatment was instead significantly associated with poor outcome in terms of median OS compared with CR, CRi, and PR (11.3 months (95% CI 9.3–13.3) vs 20.3 months (95% CI 16.2–24.4), p = 0.015). Univariate subgroup analysis confirmed all factors associated with a better OS in AZA-treated patients, while a platelet count ≥ 79.5 × 109/L, an eGFR ≥ 60 mL/min/1.73m2, a ≥ PR response, RBC, and platelet-transfusion independence remained significant among DEC-treated patients, as shown in Table 2. In multivariate analysis, a BM blast count ≥ 30%, a t-AML type, the achievement of a response ≥ PR to HMA, RBC transfusion independence, and the baseline Hb levels proved to independently predict survival (Table 3). The BM blast count, the AML type and a ≥ PR response significantly impacted on survival for the AZA group (Table 3), while no factor was confirmed for the DEC group (data not shown).
Progression-free survival
The median PFS of the entire population was 6.0 months (CI 95% 3.3–8.6) without a significant difference between the AZA and DEC groups (6.2 vs 3.8 months, respectively; p = 0.380 Suppl. Fig. 2a, b). Factors impacting significantly on the median PFS were the Hb level at baseline (p = 0.015), the BM blast count (p = 0.009), all subtypes except t-AML (p = 0.004), baseline eGFR (p = 0.004), optimal response to treatment (p < 0.001), and no requirement of RBC-T (p < 0.001) and platelet transfusion (p < 0.001) during treatment. As for OS, the achievement of a SD similar to a response ≥ PR after the fourth cycle did not affect the median PFS duration (p = 0.398). In multivariate analysis, the median blast count > 30%, the Hb level, t-AML, RBC transfusion independence during treatment and a response ≥ PR maintained significance as predictors of survival. Details regarding multivariate analysis are illustrated in Table 3.
Outcome and safety
After a median time of 4.4 months (range 0.1–46.3), 93 patients (85%) discontinued HMA therapy. All died, except for the 2 allografted patients. The main reason was PD (78%). Other reasons of death were infections (12%) or extra-hematologic complications (10%). The mortality and the cause of death did not differ significantly between the two groups (p = 0.661). The all-cause 30-day mortality of the entire cohort was 4.5%, and it was not significantly different between treatment groups, even if there is an increased trend for DEC (AZA 2.6%, DEC 9.4%; p = 0.119). Excluding early deaths related to rapid progression of disease, the 30-day mortality of the whole population studied was 2.7% (AZA 1.33%, DEC 6.3%, p = 0.146).
At the last follow-up, 17 patients (15%) are still alive and on treatment (10 AZA, 7 DEC) after a median time of 15.6 months (range 1.1–39.1). All patients were referred to our Hematologic Emergency Unit for any infectious complications. At least one infectious complication occurred in 88 patients (80%) after a median time of 41 days since the start of treatment and a median of 16 days from the start of the ongoing cycle. Thirty-seven (34%) patients of the entire cohort experienced a single episode of infection; 27 (25%) and 24 (22%) patients had 2 and ≥ 3 infectious complications, respectively. The number of infectious episodes did not significantly differ among patients according to the type of response achieved during HMA therapy, as well as any significant differences were revealed between patients who obtained SD and PD (p = 0.560). The rates of infections requiring hospitalization were 69% for AZA group and 80% for DEC group (p = 0.128). Pneumonia (46%) was the most frequent infectious event. The occurrence of pneumonia during the first four cycles of therapy did not significantly impact on median survival (p = 0.061). Furthermore, the occurrence of pneumonia was not correlated with age (p = 0.938), CCI (p = 0.177) and BM blast count at diagnosis (p = 0.553). We extensively analyzed the first three infectious events occurred in order of appearance (Suppl. Table 1). As for the first one, no statistically significant differences concerning the type of infection (p = 0.894), the grade of severity (p = 0.549), and the number of neutrophils at the onset of the event (p = 0.058) were found between the two HMA. On the contrary, the occurrence of the first complication was significantly earlier in the DEC group, both in terms of days from the start of treatment (p = 0.006) and of days from the start of the ongoing cycle (p = 0.021) over the AZA group. The severity of the second infection was higher in DEC-treated patients (grade ≥ 3 93% vs 63% of AZA group, p = 0.036). Regarding the third infectious complication recorded, no differences emerged by comparing the two groups of patients.
Long-lasting treated patients
In our cohort, 27 patients received at least 12 cycles of HMA (23 AZA, 4 DEC). The median OS and PFS were 24.4 (95% CI 13.5–47) and 22.3 months (95% CI 7.6–46), respectively. These patients showed a significantly lower blast count (p = 0.021), a higher eGFR at baseline (p = 0.028), a higher median value of lactate dehydrogenase (p = 0.048), a decreased RBC (p = 0.007) and a platelet-transfusion requirement (p = 0.040) compared with the 45 patients who received ≤ 4 cycles, excluding patients still alive and on treatment at the time of the analysis (data not shown).
Discussion
HMA represent the most commonly used therapeutic strategy for unfit AML patients, not eligible for intensive treatment. The results of sponsored trials have shown an advantage of survival associated with an acceptable toxicity compared with that of conventional care [9, 11, 12]. We herein report the results of a retrospective real-life study of unfit AML patients treated with HMA in the last 12 years at a single institution. The choice of HMA type changed over this long period of time, due to the relatively recent introduction of DEC compared with AZA and modifications of indications regarding the amount of blast count, as specified below. More than half of the analyzed population was ≥ 75 years. The median age of 75 years at diagnosis, equal for each HMA group, is in line with the epidemiology of AML and comparable with that of patients enrolled in the AZA-AML-01 and DACO-016 trials and in several real-life experiences reported in literature [11, 12, 19,20,21,22,23,24]. The baseline characteristics were not different across the AZA and DEC groups, except for the median blast count that was significantly higher in the DEC group. This imbalance may be due to the different drug availability considering that up to 2017 AZA was not reimbursed by the Italian National Health System for AML with more than 30% BM blasts. After a median time of almost 4 months, the ORR of the entire cohort was 40% (AZA 37%, DAC 47%), resulting higher than the ORR of clinical trials and other real-life experiences [11, 12, 21,22,23,24]. The MD Anderson Cancer Center (MDACC) group reported an ORR of 29% for 114 elderly AML patients who received front-line HMA compared with that of the 557 patients who underwent intensive chemotherapy, with no difference between AZA and DEC (26% and 31%, respectively) [22]. Tawfik et al [25], analyzing 32 patients who received HMA, reported an ORR of 26.5%. A recently published retrospective analysis on 306 AML patients treated front-line with DEC showed a lower ORR (33.7%) than in our experience [24]. These differences are most likely attributable to the relatively small number of patients of our cohort, especially those who underwent DEC. The median OS of our entire cohort was 8.0 months with no differences according to the type of HMA used. The median OS of the AZA group (8.8 months) was consistent with reported real-life experiences which showed a median OS between 8.1 and 13.1 months [13, 26,27,28]. On the contrary, the median OS of the DEC group (6.3 months) is lower than that of literature data [12, 23, 24], again presumably due to the sample size and also because of the strict patient selection criteria in clinical trials. To date, no factor has emerged as clearly associated with the effectiveness of HMA therapy, in terms of response, OS, and PFS. In fact, a great heterogeneity of results has been reported in the literature. Quintas-Cardama et al. [22] have recognized advanced age, unfavorable cytogenetic characteristics, a worse PS, a high creatinine level, and a blast value at diagnosis as independent predictors of poor outcome at multivariate analysis in AZA-treated patients. Maurillo et al. [27] analyzing the outcome of 82 patients treated with AZA in the Italian-named patient program, reported that a de novo AML and a WBC count < 10,000/μL were associated with a higher probability of response, while a WBC count ≥ 10,000/μL was the only factor significantly associated with a reduced OS. The French compassionate–named patient program allowed 149 patients not eligible to intensive chemotherapy to receive AZA as front-line treatment [19]. The analysis of this cohort revealed a predictive value of the cytogenetic risk on CR achievement. Adverse cytogenetics, a WBC count > 15 × 109/L and an Eastern Cooperative Oncology Group (ECOG) PS ≥ 2 independently prognosticated for a poor OS, unlike age and marrow blast count. An elevated WBC, an adverse cytogenetic category, an ECOG > 2, and age had a statistically significant impact on OS in the retrospective analysis of the largest AZA-treated cohort (n = 710) reported by Falantes et al [21]. In our experience, a BM blast count < 30%, a subgroup other than t-AML, a response ≥ PR, Hb levels higher than the median value of the whole cohort (9.25 g/dL), and transfusion independence were associated with a better OS for the whole cohort. The same factors, with the addiction of an eGFR ≥ 60 mL/min/1.73m2, were also correlated with a better PFS in multivariate analysis; furthermore, a platelet count ≥ 79.5 × 109/L, no requirement of RBC-T during treatment and a baseline eGFR ≥ 60 mL/min/1.73 m were significantly associated with achievement of a CR/CRi/PR.
Controversies still exists regarding the predictive role of cytogenetics in patients treated with epigenetic therapy. Some experiences have suggested that the poor prognosis of an unfavorable cytogenetic risk and of a TP53 mutant genetic status may be mitigated with DEC therapy in AML [29, 30]. A post hoc analysis of the DACO-016 study highlighted improved response rates and PFS for patients with a MK who underwent DEC in comparison with that of the control arm [31]. On the contrary, the pooled analysis of the Italian AML consortium observational real-world study recognized a significant increased mortality in DEC-treated patients with adverse cytogenetics according to the Medical Research Council (MRC) classification [24]. Unfortunately, the prognostic value of the cytogenetic risk has not been confirmed in our experience probably due to the lack of data for a not negligible proportion of patients. Nevertheless, genetic risk assessment based on the ELN recommendations clearly distinguished survival outcome for adverse and intermediate risk categories, despite the small percentage of patients’ data available, at univariate analysis. The amount of RBC and platelet-transfusion requirement per cycle had a strong prognostic value in our analysis: no transfusion requirement during therapy was significantly associated with a better outcome, both for AZA- and DEC-treated patients in univariate analysis. While the prognostic role of RBC transfusion requirement is well-documented for both HMA [32, 33], a correlation between platelet-transfusion need and survival among AZA-treated patients has to the best of our knowledge not been previously reported. In this regard, our retrospective study suggests that platelet-transfusion independence obtaining during HMA treatment could be an important predictor of better survival also in the AZA subgroup, albeit this was not confirmed in multivariate analysis.
A significant benefit in survival for patients who obtained a RBC and platelet-transfusion independence without CR has been observed in the DACO-016 study [33], suggesting that CR is not the only therapeutic goal of treatment with HMA. Similar considerations could be made for AZA concerning the reported survival advantage over conventional treatment even in patients who did not achieve a CR in the AZA-AML-01 trial [11]. In our study, a SD after the 4th cycle of HMA based on the ELN criteria was associated with an OS and PFS similar to those observed in patients with a ≥ PR response. Our findings reinforce the indication to continue HMA therapy as long as possible, if tolerated, since not achieving an early CR does not necessarily translate into a therapeutic failure in unfit AML patients. Although cell count stabilization could theoretically lead to improved survival rate due to the less number of complications, we did not demonstrate differences in terms of infectious events according to type of response. Further prospective investigation in real-life setting is warranted in order to answer these questions.
However, the duration of all types of response are short and, in agreement with other reports [13], the main cause of death remains AML progression, underlying the importance of combining HMA with other drugs. In this regard, assessment of response based on BM blast count, discriminating a SD from PD, could be useful to select patients who may benefit of new combination treatments.
In our study, infections were the second reason of death, demonstrating that the risk of infection during HMA therapy is becoming a relevant issue, in line with the emergent need of identifying possible infection risk factors and, accordingly, the most correct preventive strategies [34]. Indeed, primary antimicrobial prophylaxis is not routinely performed in our center, but it is guided from clinical history of the single patient and adapted to the epidemiological infectious data, certainly changed during the years. Nevertheless, we believe that the availability of a dedicated Hematologic Emergency Unit, which all patients being referred to, makes reliable our attempt in giving real-life experience concerning the infectious complications during HMA therapy, despite the long period considered, the lacking of standardized antimicrobial prophylaxis and the development of new antimicrobial agents over the years. Pneumoniae was the most frequent infection complication in our experience. Despite the relatively small sample size and the retrospective nature of the study, we could document an earlier appearance of the first infection complications in the DEC group than in AZA-treated patients. Furthermore, the severity of the second infective episodes was greater in the DEC group than in AZA-treated patients. These results may be related to the higher blast count (> 30%) in the DEC patients over the AZA group or to the greater myelosuppressive effect of DEC. In line with our observations, other retrospective comparisons found no notable differences between the two HMA according to response to treatment and survival [35,36,37], although DEC appears to be more myelotoxic then AZA in the real-life setting [35]. Moreover, Smith et al. [38] analyzing 487 elderly AML patients who received HMA reported a longer hospitalization, mainly due to infections, and a significant inferior OS in the DEC group. Talati et al. [39] described a superior OS for non-MK AZA-treated patients compared with DEC. On the contrary, patients treated with DEC had a significant survival advantage compared with those treated with AZA in the MDACC experience [22]. A more recent large SEER-Medicare linked database population-based study confirmed this assumption, showing an inferior OS for the AZA cohort compared with the DEC case series [40]. In conclusion, our retrospective study, despite the lack of robust correlation with genetic features, provides a valid comparison between the two HMA, identifying several clinical factors predictive for OS and suggesting no difference in efficacy among AZA and DEC in the real-life setting.
References
Döhner H, Weisdorf DJ, Bloomfield CD (2015) Acute myeloid leukemia. N Engl J Med 373(12):1136–1152. https://doi.org/10.1056/NEJMra1406184
Acute myeloid leukemia - Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/amyl.html. Accessed 15 February 2020
Thein MS, Ershler WB, Jemal A, Yates JW, Baer MR (2013) Outcome of older patients with acute myeloid leukemia: an analysis of SEER data over 3 Decades. Cancer. 119(15):2720–2727. https://doi.org/10.1002/cncr.28129
Appelbaum FR, Gundacker H, Head DR, Slovak ML, Willman CL, Godwin JE, Anderson JE, Petersdorf SH (2006) Age and acute myeloid leukemia. Blood. 107(9):3481–3485. https://doi.org/10.1182/blood-2005-09-3724
Prassek VV, Rothenberg-Thurley M, Sauerland MC, Herold T, Janke H, Ksienzyk B (2018) Genetics of acute myeloid leukemia in the elderly: mutation spectrum and clinical impact in intensively treated patients aged 75 years or older. Haematologica. 103(11):1853–1861. https://doi.org/10.3324/haematol.2018.191536
Pleyer L, Greil R (2015) Digging deep into “dirty” drugs - modulation of the methylation machinery. Drug Metab Rev 47(2):252–279. https://doi.org/10.3109/03602532.2014.995379
Herman JG, Baylin SB (2003) Gene silencing in cancer in association with promoter hypermethylation. N Engl J Med 349(21):2042–2054. https://doi.org/10.1056/NEJMra023075
Derissen EJB, Beijnen JH, Schellens JHM (2013) Concise drug review: azacitidine and decitabine. Oncologist. 18(5):619–624. https://doi.org/10.1634/theoncologist.2012-0465
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, Santini V, Finelli C, Giagounidis A, Schoch R, Gattermann N, Sanz G, List A, Gore SD, Seymour JF, Bennett JM, Byrd J, Backstrom J, Zimmerman L, McKenzie D, Beach C, Silverman LR, International Vidaza High-Risk MDS Survival Study Group (2009) Efficacy of AZA compared with conventional care regimens in the treatment of higher-risk MDS. Lancet Oncol 10(3):223–232. https://doi.org/10.1016/S1470-2045(09)70003-8
Fenaux P, Mufti GJ, Hellström-Lindberg E, Santini V, Gattermann N, Germing U, Sanz G, List AF, Gore S, Seymour JF, Dombret H, Backstrom J, Zimmerman L, McKenzie D, Beach CL, Silverman LR (2010) Azacitidine prolongs overall survival compared with conventional care regimens in elderly patients with low bone marrow blast count acute myeloid leukemia. J Clin Oncol 28(4):562–569. https://doi.org/10.1200/JCO.2009.23.8329
Dombret H, Seymour JF, Butrym A, Wierzbowska A, Selleslag D, Jang JH, Kumar R, Cavenagh J, Schuh AC, Candoni A, Récher C, Sandhu I, Bernal del Castillo T, al-Ali HK, Martinelli G, Falantes J, Noppeney R, Stone RM, Minden MD, McIntyre H, Songer S, Lucy LM, Beach CL, Döhner H (2015) International phase 3 study of azacitidine vs conventional care regimens in older patients with newly diagnosed AML with >30% blasts. Blood. 126(3):291–299. https://doi.org/10.1182/blood-2015-01-621664
Kantarjian HM, Thomas XG, Dmoszynska A, Wierzbowska A, Mazur G, Mayer J, Gau JP, Chou WC, Buckstein R, Cermak J, Kuo CY, Oriol A, Ravandi F, Faderl S, Delaunay J, Lysák D, Minden M, Arthur C (2012) Multicenter, randomized, open-label, phase III trial of decitabine versus patient choice, with physician advice, of either supportive care or low-dose cytarabine for the treatment of older patients with newly diagnosed acute myeloid leukemia. J Clin Oncol 30(21):2670–2677. https://doi.org/10.1200/JCO.2011.38.9429
Al-Ali HK, Jaekel N, Niederwieser D (2014) The role of hypomethylating agents in the treatment of elderly patients with AML. J Geriatr Oncol 5(1):89–105. https://doi.org/10.1016/j.jgo.2013.08.004
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, Bloomfield CD, Cazzola M, Vardiman JW (2016) The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 127(20):2391–2405. https://doi.org/10.1182/blood-2016-03-643544
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, Dombret H, Ebert BL, Fenaux P, Larson RA, Levine RL, Lo-Coco F, Naoe T, Niederwieser D, Ossenkoppele GJ, Sanz M, Sierra J, Tallman MS, Tien HF, Wei AH, Löwenberg B, Bloomfield CD (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 129(4):424–447. https://doi.org/10.1182/blood-2016-08-733196
National Cancer Institute, Division of Cancer Treatment & Diagnosis (2017) Common Terminology Criteria for Adverse Events (CTCAE) version 5.0 | Protocol Development | CTEP. https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm. Accessed 16 February 2020
Thépot S, Itzykson R, Seegers V, Recher C, Raffoux E, Quesnel B, Delaunay J, Cluzeau T, Marfaing Koka A, Stamatoullas A, Chaury MP, Dartigeas C, Cheze S, Banos A, Morel P, Plantier I, Taksin AL, Marolleau JP, Pautas C, Thomas X, Isnard F, Beve B, Chait Y, Guerci A, Vey N, Dreyfus F, Ades L, Ifrah N, Dombret H, Fenaux P, Gardin C, On behalf of the Groupe Francophone des Myélodysplasies (GFM), the Acute Leukemia French Association (ALFA); the Groupe Ouest-Est des Leucémies Aiguës; Maladies du Sang (GOELAMS) (2014) Azacitidine in untreated acute myeloid leukemia: a report on 149 patients. Am J Hematol 89(4):410–416. https://doi.org/10.1002/ajh.23654
Ramos F, Thépot S, Pleyer L, Maurillo L, Itzykson R, Bargay J, Stauder R, Venditti A, Seegers V, Martínez-Robles V, Burgstaller S, Récher C, Debén G, Gaidano G, Gardin C, Musto P, Greil R, Sánchez-Guijo F, Fenaux P, European ALMA Investigators (2015) Azacitidine frontline therapy for unfit acute myeloid leukemia patients: clinical use and outcome prediction. Leuk Res 39(3):296–306. https://doi.org/10.1016/j.leukres.2014.12.013
Falantes J, Pleyer L, Thépot S, Almeida AM, Maurillo L, Martínez-Robles V, Stauder R, Itzykson R, Pinto R, Venditti A, Bargay J, Burgstaller S, Martínez MP, Seegers V, Cortesão E, Foncillas MÁ, Gardin C, Montesinos P, Musto P, Fenaux P, Greil R, Sanz MA, Ramos F, for the European ALMA + Investigators (2018) Real life experience with frontline azacitidine in a large series of older adults with acute myeloid leukemia stratified by MRC/LRF score: results from the expanded international E-ALMA series (E-ALMA+). Leuk Lymphoma 59(5):1113–1120. https://doi.org/10.1080/10428194.2017.1365854
Quintás-Cardama A, Ravandi F, Liu-Dumlao T, Brandt M, Faderl S, Pierce S, Borthakur G, Garcia-Manero G, Cortes J, Kantarjian H (2012) Epigenetic therapy is associated with similar survival compared with intensive chemotherapy in older patients with newly diagnosed acute myeloid leukemia. Blood. 120(24):4840–4845. https://doi.org/10.1182/blood-2012-06-436055
Filì C, Candoni A, Zannier ME, Olivieri J, Imbergamo S, Caizzi M, Nadali G, di Bona E, Ermacora A, Gottardi M, Facchinelli D, Ciancia R, Lazzarotto D, Dubbini MV, Festini G, Gherlinzoni F, Michieli MG, Semenzato G, Fanin R (2019) Efficacy and toxicity of Decitabine in patients with acute myeloid leukemia (AML): a multicenter real-world experience. Leuk Res 76:33–38. https://doi.org/10.1016/j.leukres.2018.11.015
Bocchia M, Candoni A, Borlenghi E, Defina M, Filì C, Cattaneo C, Sammartano V, Fanin R, Sciumè M, Sicuranza A, Imbergamo S, Riva M, Fracchiolla N, Latagliata R, Caizzi E, Mazziotta F, Alunni G, di Bona E, Crugnola M, Rossi M, Consoli U, Fontanelli G, Greco G, Nadali G, Rotondo F, Todisco E, Bigazzi C, Capochiani E, Molteni A, Bernardi M, Fumagalli M, Rondoni M, Scappini B, Ermacora A, Simonetti F, Gottardi M, Lambertenghi Deliliers D, Michieli M, Basilico C, Galeone C, Pelucchi C, Rossi G (2019) Real-world experience with decitabine as a first-line treatment in 306 elderly acute myeloid leukaemia patients unfit for intensive chemotherapy. Hematol Oncol 37(4):447–455. https://doi.org/10.1002/hon.2663
Tawfik B, Sliesoraitis S, Lyerly S, Klepin HD, Lawrence J, Isom S, Ellis LR, Manuel M, Dralle S, Berenzon D, Powell BL, Pardee T (2014) Efficacy of the hypomethylating agents as frontline, salvage, or consolidation therapy in adults with acute myeloid leukemia (AML). Ann Hematol 93(1):47–55. https://doi.org/10.1007/s00277-013-1940-9
Pleyer L, Burgstaller S, Girschikofsky M, Linkesch W, Stauder R, Pfeilstocker M, Schreder M, Tinchon C, Sliwa T, Lang A, Sperr WR, Krippl P, Geissler D, Voskova D, Schlick K, Thaler J, Machherndl-Spandl S, Theiler G, Eckmüllner O, Greil R (2014) Azacitidine in 302 patients with WHO-defined acute myeloid leukemia: results from the Austrian Azacitidine Registry of the AGMT-Study Group. Ann Hematol 93(11):1825–1838. https://doi.org/10.1007/s00277-014-2126-9
Maurillo L, Venditti A, Spagnoli A, Gaidano G, Ferrero D, Oliva E, Lunghi M, D’Arco AM, Levis A, Pastore D, Di Renzo N, Santagostino A, Pavone V, Buccisano F, Musto P (2012) Azacitidine for the treatment of patients with acute myeloid leukemia: report of 82 patients enrolled in an Italian Compassionate Program. Cancer. 118(4):1014–1022. https://doi.org/10.1002/cncr.26354
Bernal T, Martínez-Camblor P, Sánchez-García J, de Paz R, Luño E, Nomdedeu B, Ardanaz MT, Pedro C, Amigo ML, Xicoy B, del Cañizo C, Tormo M, Bargay J, Valcárcel D, Brunet S, Benlloch L, Sanz G, Spanish Group on Myelodysplastic Syndromes; PETHEMA Foundation; Spanish Society of Hematology (2015) Effectiveness of azacitidine in unselected high-risk myelodysplastic syndromes: results from the Spanish registry. Leukemia. 29(9):1875–1881. https://doi.org/10.1038/leu.2015.115
Lübbert M, Rüter BH, Claus R, Schmoor C, Schmid M, Germing U et al (2012) A multicenter phase II trial of decitabine as first-line treatment for older patients with acute myeloid leukemia judged unfit for induction chemotherapy. Haematologica. 97(3):393–401. https://doi.org/10.3324/haematol.2011.048231
Welch JS, Petti AA, Miller CA, Fronick CC, O’Laughlin M, Fulton RS, Wilson RK, Baty JD, Duncavage EJ, Tandon B, Lee YS, Wartman LD, Uy GL, Ghobadi A, Tomasson MH, Pusic I, Romee R, Fehniger TA, Stockerl-Goldstein KE, Vij R, Oh ST, Abboud CN, Cashen AF, Schroeder MA, Jacoby MA, Heath SE, Luber K, Janke MR, Hantel A, Khan N, Sukhanova MJ, Knoebel RW, Stock W, Graubert TA, Walter MJ, Westervelt P, Link DC, DiPersio JF, Ley TJ (2016) TP53 and decitabine in Acute Myeloid Leukemia and Myelodysplastic Syndromes. N Engl J Med 375(21):2023–2036. https://doi.org/10.1056/NEJMoa1605949
Wierzbowska A, Wawrzyniak E, Pluta A, Robak T, Mazur GJ, Dmoszynska A, Cermak J, Oriol A, Lysak D6, Arthur C, Doyle M, Xiu L, Ravandi F, Kantarjian HM (2018) Decitabine improves response rate and prolongs progression-free survival in older patients with newly diagnosed acute myeloid leukemia and with monosomal karyotype: a subgroup analysis of the DACO-016 trial. Am J Hematol 93(5):E125–E127. https://doi.org/10.1002/ajh.25062
Gavillet M, Noetzli J, Blum S, Duchosal MA, Spertini O, Lambert JF (2012) Transfusion independence and survival in patients with acute myeloid leukemia treated with 5-azacytidine. Haematologica. 97(12):1929–1931. https://doi.org/10.3324/haematol.2012.065151
He J, Xiu L, De Porre P, Dass R, Thomas X (2015) Decitabine reduces transfusion dependence in older patients with acute myeloid leukemia: results from a post hoc analysis of a randomized phase III study. Leuk Lymphoma 56(4):1033–1042. https://doi.org/10.3109/10428194.2014.951845
Pagano L, Busca A, Candoni A, Criscuolo M, Giovanni Della Porta M, Fianchi L, Lessi F, Marchesi F, Teresa Voso M (2018) Risk of infection in elderly patients with AML and MDS treated with hypomethylating agents. Acta Biomed 89(Suppl 11):5–39. https://doi.org/10.23750/abm.v89i11-S.7988
Imbergamo S, Visentin A, Kostic I, Pravato S, Scomazzon E, Laurino M, Binotto G, Lessi F, Berno T, Gurrieri C, Semenzato G, Trentin L (2018) Azacitidine or decitabine frontline therapy for acute myeloid leukemia in elderly patients? EHA Open Access Library 06/14/18; Abstract 216256; PB1741 https://library.ehaweb.org/eha/2018/stockholm/216256/silvia.imbergamo.azacitidine.or.decitabine.frontline.therapy.for.acute.myeloid.html?f = menu = 14*media = 3*speaker = 664538.
Mehra M, He J, Potluri R, Loefgren C (2017) Utilization of hypomethylating agents and associated outcomes in elderly Acute Myeloid Leukemia (AML) patients: a population based study. Blood 130(Supplement 1):2157–2157. https://doi.org/10.1182/BLOOD.V130.SUPPL_1.2157.2157
Ebaid A, Cingam S, Boyce T, Babu D, Liu Q, Win K, Arana Yi C (2019) Comparative analysis for effectiveness of azacitidine versus decitabine in Acute Myeloid Leukemia and Myelodysplastic Syndromes with marrow fibrosis: a single institution experience. Blood 134(Supplement_1):5099. https://doi.org/10.1182/blood-2019-131881
Smith BD, Beach CL, Mahmoud D, Weber L, Henk HJ (2014) Survival and hospitalization among patients with acute myeloid leukemia treated with azacitidine or decitabine in a large managed care population: a real-world, retrospective, claims-based, comparative analysis. Exp Hematol Oncol 3(1):10. https://doi.org/10.1186/2162-3619-3-10
Talati C, Kuykendall A, Al-Ali N, Komrokji R, Padron E, Sallman D, List A, Sweet K, Extermann M, Lancet J (2017) Improved responses with azacitidine compared to decitabine in patients with acute myeloid leukemia in patients ≥70 with poor-risk cytogenetics. Clin Lymphoma Myeloma Leuk 17:S295. https://doi.org/10.1016/j.clml.2017.07.085
Zeidan A, Wang R, Wang X, Shallis R, Podoltsev N, Bewersdorf JP, Huntington S, Neparidze N, Giri S, Gore S, Davidoff A, Ma X (2019) Clinical outcomes of older patients (pts) with acute myeloid leukemia (AML) receiving hypomethylating agents (HMAs): a large population-based study in the United States. Blood 134(Supplement_1):646–646. https://doi.org/10.1182/blood-2019-127398
Author information
Authors and Affiliations
Contributions
MB and SP wrote the manuscript and analyzed data; GC and DD performed molecular analyses; MMan performed cytogenetic analysis; ES, RL, and ADP followed patients and collected data; and MMar and RF revised the final version of the paper.
Corresponding author
Ethics declarations
Conflicts of interest
MB received honoraria from Novartis, Pfizer, Incyte, and Celgene. All the other authors declare that they have no conflict of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the responsible institution and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this kind of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 119 kb)
Rights and permissions
About this article
Cite this article
Pepe, S., Scalzulli, E., Colafigli, G. et al. Predictive factors for response and survival in elderly acute myeloid leukemia patients treated with hypomethylating agents: a real-life experience. Ann Hematol 99, 2405–2416 (2020). https://doi.org/10.1007/s00277-020-04217-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-020-04217-w