Abstract
Sickle cell disease (SCD) is a relatively common inherited hemolytic anemia among individuals of African descent. Genetic factors might clarify clinical diversity of the disease and variations in treatment response. Some researchers investigated heme oxygenase-1 (HMOX1) or chemokine receptor 5 (CCR5Δ32) genotypes among SCD patients and their correlation with fetal hemoglobin (HbF) and disease severity. However, there are no such records among Arab nations. We aimed to estimate the prevalence of the HMOX1-413 A>T (rs2071746) and CCR5Δ32 (rs333) polymorphisms, and to assess their effect on SCD phenotype and HbF level among Egyptian patients. Polymerase chain reaction assay was used to determine these polymorphisms among 100 SCD patients and 100 healthy controls. Though not statistically significant, the frequency of individual carrying HMOX-1 polymorphic AT and TT genotypes in both patient and control groups was 92% and 85% respectively. Regarding CCR5Δ32 polymorphisms, all SCD patients harbored the wild genotype (100%), while the heteromutant genotype was encountered in 2% of our controls. Patients harboring mutant HMOX-1 had a less frequent vaso-occlusive crisis (VOC)/lifetime, less VOC in the last year, less incidence of stroke, less frequency of hospitalization, and responded more frequently to hydroxyurea with statistically significant differences (p = 0.028, 0.007, 0.046, 0.007, and 0.011 respectively). No significant associations with HbF level or other hematologic parameters were encountered among our cohort. Our study results suggest a protective effect of mutant HMOX-1 genotypes in ameliorating the phenotypic severity of the disease. HMOX1-413 A>T (rs2071746) polymorphisms might prove to be a prognostic marker among Egyptian SCD, but not CCR5Δ32 (rs333) polymorphisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sickle cell disease (SCD) is a relatively common inherited hemolytic anemia among individuals of African descent [1]. It is characterized by a recurrent painful vaso-occlusive crisis (VOC), resulting in a chronic inflammatory state for its subsequent ischemic injury that might end with organ damage [2]. As a consequence of hemolysis of sickle erythrocyte releasing a high amount of free heme into the plasma which becomes the major source of oxidative stress, vascular inflammation developed among persons with SCD [3].
Hemoglobin S (HbS) originated as a point mutation from the substitution of valine for glutamic acid at position 6 of the β-globin chain, resulting in changes in the solubility and stability of the hemoglobin molecule that promotes polymerization in red blood cells upon deoxygenation [4]. Although the disease is caused by mutation of a single base pair in β-globin gene, vast phenotypic diversity and genetic heterogeneity make the prediction of disease severity and clinical manifestation for providing the appropriate treatment challenging [2, 5, 6].
Many genetic factors such as S-globin haplotype, co-inherited α-thalassemia [7], and fetal hemoglobin (HbF) synthesis have a significant role in moderating the clinical phenotype of SCD, reducing the predisposition for hemoglobin polymerization inside erythrocyte, and subsequently reducing the severity of clinical events such as vascular occlusion, pain, chest syndrome, and stroke [6]. Undoubtedly, the genetic background plays a vital role in determining the average levels of HbF among different population [6]. Although, environmental factors play partially a role in these variations, genetic modulators that are linked or unlinked to β-globin gene cluster seem to have a greater role which is still not fully understood [5, 7].
In SCD, some reviews have suggested that in addition to SNP within some genes of the β-globin gene cluster, other genes outside it such as heme oxygenase-1 (HMOX1) and chemokine receptor 5 (CCR5) can affect disease severity [5, 8]. It has been suggested that these polymorphisms not only associated with the severity of anemia but also with the frequency of pain recurrence, stroke incidence, priapism, leg ulcers, and chest and hepato–biliary complications among other numerous clinical aspects [9].
The HMOX1 gene, which encodes HMOX1 antioxidant enzyme, plays a crucial role in the protection of cells from oxidative stress during heme catabolism initiated by hemolysis [10]. Previous studies reported that HMOX1 gene is overexpressed in sickle cell patients [8]. Moreover, Belcher et al. (2006) [3] demonstrated its vital importance in ameliorating vascular inflammation and vaso-occlusion in transgenic sickle mice [3]. Other studies have shown that polymorphisms of the HMOX1 gene, including rs2071746: A>T, cause an increase in the HbF level; therefore, it can affect the disease severity [6]. Recently, it was also revealed that T allele of the gene (rs2071746: A>T polymorphism) diminishes its expression [8].
Regarding CCR5, Th1 cell–associated chemokine receptor, which plays crucial roles in the immune system through regulation of immune cell migration and its activation during the immune response, has been associated with chronic inflammatory states [11]. Therefore, genetic polymorphism in CCR5 is suggested to be a molecular genetic marker that might indicate the susceptibility to various inflammatory diseases [12, 13]. Several studies revealed that CCR5-Δ32 (rs333) polymorphism, a 32-bp deletion in the coding region in exon 1 of the CCR5 gene, led to downregulation of the gene with less efficient Th1 response [11, 14]. Hence, considering the inflammatory role in the pathophysiology of SCD, CCR5Δ32 allele, which encodes for truncated C-C chemokine receptor type 5 (CCR5), might offer a selective benefit on its carrier. However, CCR5Δ32 role as a protective factor against the disease is still a matter of controversy and its allele frequency varies widely around the world [11].
Many studies aimed to investigate genetic variations that might explain clinical diversity and variable response rates to treatment among SCD patients [2, 5].
In Arab African population, there has been no literature published yet, to the best of our knowledge, on neither HMOX1 nor CCR5Δ32 genotypes among SCD patients, and if these polymorphisms could deliberate a selective benefit on the patients. Thus, we aimed in this foremost study of HMOX1 and CCR5Δ32 genotypes among SCD patients in the Arab African population to estimate the prevalence of the HMOX1-413 A>T (rs2071746) and CCR5Δ32 (rs333) polymorphisms and to assess their correlation with HbF level and their effect on the disease phenotype among Egyptian SCD patients.
Materials and methods
Study population
This study included 100 steady-state Egyptian SCD patients (both homozygous SS and Sβ thalassemia) diagnosed and followed up at the Pediatric Hematology & BMT Unit, Cairo University Children Hospital, Egypt. Their mean age was 13.7 ± 8.9 years (range 2–39 years). There were 47 males and 53 females. One hundred age- and sex-matched unrelated healthy Egyptian children with normal hemoglobin electrophoresis were included as a control group in the study. The study protocol was approved by the Research Ethics Committee of Faculty of Medicine, Cairo University. Informed consents were willingly given by the parents or guardians of participants prior to enrollment in the study. Clinical history was recorded, and clinical and laboratory evaluations were completed at the time of initial presentation and follow-up visits. VOC was defined as pain in the extremities, abdomen, back, chest, or head that led to emergency room visit or an unscheduled clinic and could not be explained except by SCD, with exclusion of chest syndrome, hand–foot syndrome, osteomyelitis, and any pain episode that can be managed entirely at home. Quantitative assessment of hemoglobin variants for diagnosis of SCD was executed by high-performance liquid chromatography (HPLC). All procedures performed in our study were in accordance with the 1964 Helsinki declaration.
Genomic DNA extraction
Venous blood samples were obtained from all participants by sterile venipuncture in EDTA vacutainers. The Gene JET Whole Blood Genomic DNA Purification Mini Kit (Fermentas Life Sciences, Canada) was used for genomic DNA extraction from peripheral blood leukocytes according to manufacturer’s protocol. Samples were stored at − 20 °C in elution buffer until use.
CCR5Δ32 (rs333) genotyping
Genotyping of CCR5Δ32 (rs333) was carried out as previously described (DÌaz et al. 2000) [15]. Polymerase chain reaction (PCR) was performed using a thermocycler (PerkinElmer 9700; PerkinElmer, Foster City, CA, USA) to amplify the specific DNA fragment of CCR5 gene using primer set: CCR5 delta-1: 5′-ACCAGATCTCAAAAAGAAGGT CT-3′ and CCR5 delta-2: 5′-CATGATGGTGAAG ATAAGCCTCACA-3′. The PCR amplification program used was an initial denaturation at 95 °C for 10 min, followed by 30 cycles of 96 °C for 15 s, 58 °C for 60 s, and 72 °C for 60 s, then followed by a final extension step at 72 °C for 10 min. A PCR-amplified product was detected by electrophoresis using 2% agarose gel.
The PCR-amplified product was detected at 206 bp and at 174 bp for wild (CCR5/CCR5) and mutant homozygous (delta-32/delta-32) genotypes respectively. The presence of both bands together indicated a heterozygous genotype carrying both the wild (CCR5) allele and the mutant (CCR5 delta; CCR5Δ32) allele.
HMOX1-413A>T (rs2071746) genotyping
HMOX1-413A/T (rs2071746) SNP was detected using a simple allele-specific PCR. Based on the nucleotide sequence of GenBank S58267, two sets of primer pairs were designed to amplify a 307-bp target sequence which shares the same forward primer but differs only in the 3′-nucleotide end of the reverse primers, making them allele-specific [16].
The primers used were one common forward and two reverse primers for the wild-type, A allele and the variant, T allele.
F: 5′-ACTGGCACTCTGCTTTATGTGTGA-3′
R (− 413) A: 5′-GGAGGCAGCGCTGCTCAGAGTAAT-3′
R (− 413) T: 5′-GGAGGCAGCGCTGCTCAGAGTAAA-3′
The PCR amplification program used an initial denaturation at 95 °C for 10 min, then followed by 35 cycles of 94 °C for 30 s, 60 °C for 30 s, and 72 °C for 30 s, then ended by a final extension step at 72 °C for 10 min. The PCR-amplified product was detected by electrophoresis using 1.5% agarose gel.
The PCR-amplified product was detected at 163 bp for wild genotype (AA). Mutant homozygous (TT) genotype was detected at 140 bp and 23 bp, although 23 bp was too small to be detected by the gel electrophoresis. The presence of all these bands together indicated a heterozygous genotype carrying both the wild-type and the mutant allele (AT).
Statistical data analysis
The data were analyzed using SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA) version 21. Qualitative data were represented as frequency and percentage. Parametric numerical data were represented as mean, standard deviation, and range, while nonparametric data were represented as median and interquartile range. For analyzing the relation between qualitative variables, chi-square test or Fisher’s exact test was selected. The Mann–Whitney test was performed to analyze nonparametric numerical data. p values less than 0.05 were considered significant. Chi-square (v2) test was used to evaluate deviation from Hardy–Weinberg equilibrium (HWE). Genotypic distribution of the studied SNPs was in accordance with the Hardy–Weinberg equilibrium (p > 0.05).
Results
Frequency of HMOX-1 and CCR5 genetic polymorphisms in SCD and control
Out of 100 SCD patients, 67 were homozygous (SS) (31 male and 36 female with mean age 14.09 ± 8.61 years), and 33 sickle β-thalassemia (Sβ) (15 male and 18 female with mean age 12.76 ± 9.68 years). Though not statistically significant, the frequency of HMOX-1 mutant genotypes (AT) and (TT) in both patients and control groups was higher than that in wild genotype (AA). CCR5Δ32 null mutation was predominant in both patients and control groups (100% and 98% respectively) with no significant difference between SCD patients and controls (p > 0.05) (Table 1). No statistically significant differences were found in frequencies of both HMOX-1 and CCR5Δ32 genotypes between SS and Sβ, which justifies further analysis of our results as one category for entire SCD patients (Table 2).
Effect of HMOX-1 and CCR-5 genetic polymorphisms on disease phenotype and HbF level
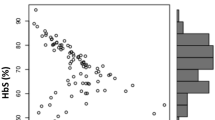
The clinical and laboratory data of SCD were studied according to HMOX-1 and CCR5Δ32 polymorphisms. We compared clinical and laboratory data between wild, heteromutant, and homomutant HMOX-1 genotypes (Tables 3 and 4). The mutant HMOX-1 genotype seems to have a protective effect and was associated with less severe disease phenotype; patients harboring heteromutant or homomutant HMOX-1 genotypes had less frequent VOC/lifetime and over the last year, less frequency of stroke and less frequency of hospitalization with a statistically significant difference (p value = 0.028, 0.007, 0.046, and 0.007 respectively) (Table 4). In addition, clinical response to hydroxyurea (as evidenced by decreased frequency of VOC, hospitalization, and transfusions per year) was more frequently detected with HMOX-1 mutant genotypes than with wild genotype with statistically significant difference (p = 0.011). However, no statistically significant associations were noted in other clinical, hematological, and laboratory parameters including HbF level among SCD patients according to their HMOX-1 genotypes (AA, AT, and TT). Since all SCD had CCR-5 wild genotype (100%), no further study of effect of this genetic polymorphism on disease could be done.
Discussion
Evaluation of genetic variation and its association with the clinical diversity of patients with sickle cell anemia is one of the strategies for elucidating its underlying etiology, pathogenesis, and disease outcomes [2]. This study, to the best of our knowledge, is the first to assess the impact of HMOX-1 and CCR5 allelic polymorphisms among individuals with SCD in Arab African regions.
Our study demonstrated that the frequency of Egyptian individuals harboring HMOX-1 (AT) and (TT) mutant genotypes in both patients (53% and 39% respectively) and unaffected control groups (44.4% and 41.4% respectively) was higher than that of HMOX-1 wild genotype (AA) (8% and 14.1% respectively). In contrast, Jaseb et al. (2017) [8], an Iranian research group, reported that allele A in this polymorphism was the most frequent allele among both SCD patients and healthy control groups [8]. In a Brazilian cohort, the most prevalent allele among SCA patients and unaffected individuals was heterozygous AT (44% and 62% respectively), whereas AA and TT genotypes were equivalent in both control and SCD patients [6].
In regard to the allele frequencies of CCR5Δ32, we found that null allele mutation of CCR5Δ32 was the predominant allele among the Egyptian SCD patients and unaffected individuals (100% and 98% respectively). In a genotype survey study conducted on 4166 subjects across Eurasia, CCR5 allele frequency ranged from 0 to 14% [17]. A similar absence of CCR5Δ32 variant was found among other populations such as native black African, Saudi, Lebanese, Chinese, Korean, Georgian, and American Indian [17] or rarely encountered among others such as Emiratis and Tunisians with frequency of 0.002 and 0.013 respectively [13]. Higher frequencies in certain ethnic populations were reported among Israel, Poland, Portugal, Turkey, Spain, Sweden, Brazil, Italy, Cyprus, and Greece populations (14.3%, 12.1%, 8%, 9.1%, 9.4%, 6%, 4%, 3%, 2.8%, and 2.4% respectively) [12, 18]. These variations in reported frequencies may be attributed to ethnic differences in studied cohorts and differences in sample size.
Our study revealed no significant differences in the frequencies of both HMOX-1 and CCR5Δ32 genotypes between SCD and healthy unaffected individuals. Similar findings were reported in a Brazilian cohort that included 795 SCD patients from various ethnic backgrounds in the northeastern region of Brazil that could not propose the contribution of the CCR5Δ32 mutant allele on the disease outcomes [11]. This finding was in concordance with Nascimento et al.’s results [19]. In contrast to our finding, Chies and Hutz (2003) [5] reported that the CCR5Δ32 allele was more prevalent among SCD patients than that of unaffected individuals (5.1% and 1.3% respectively) [5]. Unfortunately, no particular studies assessing the significant difference of HMOX-1 polymorphism between sickle cell patient groups and controls were found for comparison with our results.
Moreover, our results revealed no significant differences in the frequencies of both HMOX-1 and CCR5Δ32 polymorphisms between SS and Sβ haplotypes. This goes in agreement to that reported by an Iranian study regarding HMOX-1 polymorphism [8].
Furthermore, our study results suggest a protective effect of mutant HMOX-1 genotypes ameliorating phenotypic severity of disease; patients harboring mutant HMOX-1 had less frequent VOC/lifetime, less VOC in the last year, less incidence of stroke, less frequency of hospitalization, and responded more frequently to hydroxyurea with statistically significant differences (p = 0.028, 0.007, 0.046, 0.007, and 0.011 respectively). An efficient response of HMOX-1 might be of importance in protecting patients with SCD by several mechanisms. First, HMOX-1 can ameliorate vaso-occlusion and prevent vascular inflammation through converting damaging heme into biliverdin and carbon monoxide molecules that have antioxidant, anti-inflammatory, and cytoprotective properties [2]. Second, HMOX-1 upregulation has the ability to inhibit leukocyte adhesion and EC adhesion molecule expression [21,22,23]. The elicited injurious role of heme released by chronic red blood cell sickling and lysis is not only because heme is a major source of damaging reactive oxidative species [2], but also for its role in impairing oxidative burst activity of neutrophil to mount its bactericidal effect [24].
On the other hand, other previous studies were quite similar to our findings regarding the nonsignificant association between HMOX-1 (rs2071746: A>T polymorphism) and other clinical/hematological parameters of SCD such as the occurrence of cholelithiasis, acute chest syndrome, and incidence of hospitalization [2, 6, 8, 20]. Whereas, Gil et al. (2013) [6] and Jaseb et al. (2017) [8] found, in contradictory to our finding, that TT genotype of HMOX-1 (rs2071746: A>T polymorphism) was associated with increased levels of HbF (p = 0.0131) [6, 8].
Limitation
The main limitation of our study is the relatively small sample size that may be unpowered to find a significant association with hematological parameters including the level of HbF; however, we were able to show a significant association between HMOX-1 mutant genotype and severity of the disease.
Conclusion
Egyptian SCD patients harboring the mutant HMOX-1 genotypes had a significantly less severe disease and more frequent response to hydroxyurea than those having the wild genotype. Null mutation of CCR5Δ32 genotype was the predominant allele among the Egyptian population. HMOX1-413 A>T (rs2071746) polymorphisms might prove to be a prognostic marker among Egyptian SCD, but not CCR5Δ32 (rs333) polymorphisms.
References
Diallo DA, Guindo A (2014) Sickle cell disease in sub-Saharan Africa: stakes and strategies for control of the disease. Curr Opin Hematol 21(3):210–214
Bean CJ, Boulet SL, Ellingsen D, Pyle ME, Barron-Casella EA, Casella JF, Payne AB, Driggers J, Trau HA, Yang G, Jones K (2012) Heme oxygenase-1 gene promoter polymorphism is associated with reduced incidence of acute chest syndrome among children with sickle cell disease. Blood. 120(18):3822–3828
Belcher JD, Mahaseth H, Welch TE, Otterbein LE, Hebbel RP, Vercellotti GM (2006) Heme oxygenase-1 is a modulator of inflammation and vaso-occlusion in transgenic sickle mice. J Clin Invest 116(3):808–816
Serjeant GR (1992) Sickle cell disease, 2nd edn. Oxford University Press Inc, New York
Chies JA, Hutz MH (2003) High frequency of the CCR5delta32 variant among individuals from an admixed Brazilian population with sickle cell anemia. Braz J Med Biol Res 36(1):71–75
Gil GP, Ananina G, Oliveira MB, Costa FF, Silva MJ, Santos MN, Bezerra MA, Hatzlhofer BL, Araujo AS, Melo MB (2013) Polymorphism in the HMOX1 gene is associated with high levels of fetal hemoglobin in Brazilian patients with sickle cell anemia. Hemoglobin. 37(4):315–324
Geard A, Pule GD, Chetcha Chemegni B, Ngo Bitoungui VJ, Kengne AP, Chimusa ER, Wonkam A (2017) Clinical and genetic predictors of renal dysfunctions in sickle cell anaemia in Cameroon. Br J Haematol 178(4):629–639
Jaseb K, Ramezani A, Far MA, Mohammadi-Asl J, Khosravi A, Saki N (2017) Association between beta globin haplotypes, HBBP1 and HMOX1 polymorphisms in relation to HbF among sickle cell anemia patients: a study in Southwest Iran. Comp Clin Pathol 26(5):1149–1155
Fertrin KY, Costa FF (2010 Aug 1) Genomic polymorphisms in sickle cell disease: implications for clinical diversity and treatment. Expert Rev Hematol 3(4):443–458
Ono K, Mannami T, Iwai N (2003) Association of a promoter variant of the haeme oxygenase-1 gene with hypertension in women. J Hypertens 21(8):1497–1503
Lopes MP, Santos MN, Faber EW, Bezerra MA, Hatzlhofer BL, Albuquerque DM, Zaccariotto TR, Ribeiro DM, Araújo AD, Costa FF, Sonati MD (2014) The CCR5Δ32 polymorphism in Brazilian patients with sickle cell disease. Dis Markers 2014:1–4. https://doi.org/10.1155/2014/678246
Silva-Carvalho WH, de Moura RR, Coelho AV, Crovella S, Guimarães RL (2016) Frequency of the CCR5-delta32 allele in Brazilian populations: a systematic literature review and meta-analysis. Infect Genet Evol 43:101–107
Al-Jaberi SA, Ben-Salem S, Messedi M, Ayadi F, Al-Gazali L, Ali BR (2013) Determination of the CCR5∆ 32 frequency in Emiratis and Tunisians and the screening of the CCR5 gene for novel alleles in Emiratis. Gene. 529(1):113–118
Ghorban K, Dadmanesh M, Hassanshahi G, Momeni M, Zare-Bidaki M, Arababadi MK, Kennedy D (2013) Is the CCR5 Δ 32 mutation associated with immune system-related diseases? Inflammation. 36(3):633–642
DÌaz F, Vega JA, PatiÒo PJ, Bedoya G, Nagles J, Villegas C, Vesga R, Rugeles MT (2000) Frequency of CCR5 ∆32 mutation in human immunodeficiency virus (HIV)-seropositive and HIV-exposed seronegative individuals and in general population of Medellin, Colombia. Mem Inst Oswaldo Cruz, Rio de Janeiro 95(2):237–242
Hansson HH, Maretty L, Balle C, Goka BQ, Luzon E, Nkrumah FN, Schousboe ML, Rodrigues OP, Bygbjerg IC, Kurtzhals JA, Alifrangis M, Hempel C (2015) Polymorphisms in the Haem oxygenase-1promoter are not associated with severity of Plasmodium falciparum malaria in Ghanaian children. Malar J 14:153
Stephens JC, Reich DE, Goldstein DB, Shin HD, Smith MW, Carrington M, Winkler C, Huttley GA, Allikmets R, Schriml L, Gerrard B (1998) Dating the origin of the CCR5-Δ32 AIDS-resistance allele by the coalescence of haplotypes. Am J Hum Genet 62(6):1507–1515
Ferreira-Fernandes H, Santos AC, Motta FJ, Canalle R, Yoshioka FK, Burbano RR, Rey JA, da Silva BB, Pinto GR (2015) Prevalence of CCR5-Δ32 and CCR2-V64I polymorphisms in a mixed population from northeastern Brazil. Genet Mol Res 14(4):11710–11718
Nascimento AF, Oliveira JS, Junior JS, Barbosa AA (2017) Haplotypes and polymorphism in the CCR5 gene in sickle cell disease. Genet Mol Res 16(2). https://doi.org/10.4238/gmr16029675
Vasavda N, Menzel S, Kondaveeti S, Maytham E, Awogbade M, Bannister S, Cunningham J, Eichholz A, Daniel Y, Okpala I, Fulford T (2007) The linear effects of α-thalassaemia, the UGT1A1 and HMOX1 polymorphisms on cholelithiasis in sickle cell disease. Br J Haematol 138(2):263–270
Wagener FA, da Silva JL, Farley T, de Witte T, Kappas A, Abraham NG (1999) Differential effects of heme oxygenase isoforms on heme mediation of endothelial intracellular adhesion molecule 1 expression. J Pharmacol Exp Ther 291(1):416–423
Wagener FA, Eggert A, Boerman OC, Oyen WJ, Verhofstad A, Abraham NG, Adema G, van Kooyk Y, de Witte T, Figdor CG (2001) Heme is a potent inducer of inflammation in mice and is counteracted by heme oxygenase. Blood. 98(6):1802–1811
Soares MP, Seldon MP, Gregoire IP, Vassilevskaia T, Berberat PO, Yu J, Tsui TY, Bach FH (2004) Heme oxygenase-1 modulates the expression of adhesion molecules associated with endothelial cell activation. J Immunol 172(6):3553–3563
Evans C, Orf K, Horvath E, Levin M, De La Fuente J, Chakravorty S, Cunnington AJ (2015) Impairment of neutrophil oxidative burst in children with sickle cell disease is associated with heme oxygenase-1. haematologica. 100(12):1508–1516
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the Research Ethics Committee of Faculty of Medicine, Cairo University. Informed consents were willingly given by the parents or guardians of participants prior to enrollment in the study. All procedures performed in our study were in accordance with the 1964 Helsinki declaration.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 133 kb)
Rights and permissions
About this article
Cite this article
Bakr, S., Khorshied, M., Talha, N. et al. Implication of HMOX1 and CCR5 genotypes on clinical phenotype of Egyptian patients with sickle cell anemia. Ann Hematol 98, 1805–1812 (2019). https://doi.org/10.1007/s00277-019-03697-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-019-03697-9