Abstract
Background
Sickle Cell Anemia (SCA) is a genetic disease caused by the c.20 A > T mutation in HBB gene, generally characterized by sickle erythrocytes, chronic hemolytic anemia, and vaso-occlusive events. This study aimed to investigate genetic modulators of anemia severity, chronic hemolytic rate, and clinical manifestations in pediatric SCA patients from Angola, where the disease is a severe public health problem.
Methods and Results
The study was conducted on 200 SCA children living in Luanda or Caxito province. Their clinical phenotype was collected from patients’ hospital records. Hematological and biochemical phenotypes were characterized in steady state condition. Twelve polymorphic regions in VCAM1, CD36 and NOS3 genes were genotyped using PCR, RFLP, and Sanger sequencing. CD36 gene promoter variants showed a significant impact on anemia severity. Particularly, the rs1413661_C allele was associated with lower hemoglobin levels, and increased number of hospitalizations and transfusions. This is the first report associating this SNP with SCA phenotypic heterogeneity. Moreover, the rs1041163_C allele in VCAM1 was associated with lower LDH levels; inversely the rs2070744_C allele in NOS3 was related with higher LDH levels and number of hospitalizations, being a risk factor for increased hemolytic rate.
Conclusion
This study highlights, for the first time in the Angolan population, the importance of the genetic modifiers of vascular cell adhesion and nitric oxide metabolism in SCA pediatric phenotypic variability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sickle Cell Anemia (SCA) is a genetic chronic hemolytic anemia due to homozygosity for a single nucleotide alteration in the beta-globin gene (HBB:c.-20 A > T) that leads to a glutamic acid being replaced by a valine in the sixth amino acid of the mature β-globin chain of hemoglobin. This substitution originates a hemoglobin variant named S (HbS) that, upon deoxygenation, forms polymers inside the red blood cells (RBCs), sickling them and leading to premature extravascular and intravascular hemolysis. Clinically, SCA is a complex multisystem disease with high heterogeneity of symptoms, such as recurrent episodes of vaso-occlusion and consequent end-organ ischemia-reperfusion injury and infarction, chronic inflammation, and frequent infection episodes [1, 2].
SCA is the most common and severe form of sickle cell disease (SCD), which can be caused by compound heterozygosity for the HbS allele and other different HBB mutated allele. SCD is a major worldwide health problem, affecting between 300,000 and 400,000 neonates globally each year, and it is estimated that 75% of these births occur in Sub-Saharan Africa [1, 2]. On the African continent, the disease has a mortality rate of 50–90% among undiagnosed children under the age of five, which may contribute up to 5% of child mortality [3, 4]. Such is the case of Angola where 12,000 babies are estimated to be born with SCD each year, but most will die without a correct diagnosis [5]. This high mortality rate might be explained by the difficulty that patients and their families have in getting proper health care, medicines, and health education. Other factors that increase morbidity and mortality of this disease in Africa are the co-existence of several infectious diseases and malnutrition.
Despite the adverse environmental factors aforementioned, SCD has a remarkably high phenotype diversity also due to several genetic modifiers, some of which can be notoriously beneficial. In this context, the main factors associated with milder SCD phenotypes are the high levels of fetal hemoglobin and the coinheritance of α-thalassemia[6, 7]. However, these two biomarkers can only explain a small fraction of the observed phenotypic variability. Thus, in order to improve the knowledge about SCA in Angola, where it remains largely unknown, we aimed to investigate the role of genetic variants in genes related with RBCs vascular adhesion (VCAM1 and CD36) and vascular tonus (NOS3) in the modulation of clinical manifestations, anemia severity, and chronic hemolytic rate in Angolan children with SCA.
It is known that the exacerbated hemolytic process in SCA accounts for the diminished life span of the sickle RBCs, from the normal 120 days to only about 17 days [8]. Due to this chronic hemolytic process, large amount of cell-free plasma hemoglobin is released and greatly affects the bioavailability of Nitric Oxide (NO) by scavenging it. NO is a ubiquitous uncharged gas with potent vasodilation and antiadhesive properties that functions as a signaling molecule with a well-established role in vascular homeostasis, platelet aggregation inhibition and transcription repression of the cell adhesion molecules [9, 10]. Moreover, cell-free hemoglobin, heme and heme-iron catalyze the production of free oxygen radicals, further limiting NO bioavailability and activating the endothelium. On the other hand, lysed RBCs also release arginase that destroys L-arginine, the precursor of NO. Therefore, in these patients, the vascular balance is skewed towards a vasoconstriction state, with endothelial activation and proliferation [9]. Nitric oxide synthase 3 (encoded by NOS3 gene) is the enzyme responsible for the production of nitric oxide in endothelial cells. Some NOS3 gene variants have been implicated in decreased NO production and consequently increasing susceptibility for vascular diseases [10]. Consequently, in this study, one of our aims was to investigate the role of NOS3 common variants on the modulation of the phenotypic consequences of this NO-resistance state, namely on the chronic hemolytic anemia severity and adverse clinical events.
On the other hand, chronic inflammation is a common feature of SCD. Therefore, in SCD patients, the sialoglycoprotein vascular cell adhesion molecule-1, encoded by VCAM1 gene, is highly expressed at the surface of endothelial cells of both large and small vessels, following cytokine stimulation, and sickle RBCs are particularly prone to adhere to them [11,12,13,14]. Several VCAM1 variants have been studied and associated to phenotypic differences between SCA patients, individually or grouped in haplotypes [15,16,17,18,19,20]. In addition, under hypoxic conditions, the polymerization of HbS and sickling of RBCs cause alterations in their cell membrane properties, leading to reduced cellular deformability and unusual cell adherence to the vascular endothelium. One of the adhesion molecules involved in these interactions is the Cluster of Differentiation-36 (CD36). It is a transmembrane protein belonging to the class B scavenger receptor family expressed in a variety of cells, such as, monocytes, macrophages, adipocytes, endothelial cells, platelets, and in erythroblasts during erythropoiesis process. However, in these latter cells, CD36 protein is lost before the cell matures and enters the bloodstream circulation as reticulocytes [21]. Conversely, in SCA, the erythropoiesis is intensely increased (stress erythropoiesis) and is characterized by lifelong reticulocytosis. Consequently, a great number of immature RBCs, still containing the CD36 protein, are released into the circulation and are therefore implicated in adhesiveness to endothelial cells lining the blood vessels [21, 22]. Thus, in this study, we sought to determine the role of VCAM1 and CD36 variants in the pathophysiological mechanism of RBCs adhesion to the activated endothelium in SCA, and the implicated modulation of patients’ clinical manifestations, anemia severity, and chronic hemolytic rate.
Materials and methods
Patient population and data source
This cross-sectional study is part of a larger study in an Angolan SCD cohort conducted in Hospital Pediátrico David Bernardino, in Luanda, Hospital Geral do Bengo, in Caxito, and Centro de Investigação em Saúde de Angola (CISA), in Caxito. For this investigation, two hundred children homozygous for Hb S (SCA patients), were enrolled. Patient’s eligibility criteria included: Angolan ancestry, age ≥ 3 years old, previous diagnosis of SS (obtained by the study of hemoglobin fractions), never treated with hydroxyurea, and no blood transfusion in the three months prior to blood collection. The study’s aim and general procedures were explained to the children’s parents (or legal guardians) and they provided informed written consent prior to their enrolment in this study. This work was approved by the Ethical Committee of Ministry of Health of Angola and by the Ethical committees of all participating institutions.
The study medical appointments were done in the context of patients’ routine medical follow-up. In the first clinic consultation conducted by the pediatrician, a complete physical exam was performed, and an anamnesis questionnaire was obtained, which included demographic characteristics and current symptoms. In addition, retrospective clinical data were collected from the patients’ hospital records, including characteristics of SCA first manifestation, number of blood transfusions/year, number of hospitalizations/year, stroke events (yes/no), osteomyelitis events (yes/no), splenomegaly events (yes/no), splenectomy events (yes/no), hepatomegaly events (yes/no).
For each participant, about 4 mL of peripheral whole blood sample was collected in EDTA tubes and dry serum tubes. Blood samples were used for hematological and biochemical analyses and for DNA extraction. Patients enrolled in the study were followed-up in pediatric consultations every three months.
Hematological and biochemical parameters
The peripheral blood sample of each participant was used for a complete blood count evaluation in a XT-2000i Hematology Analyzer (Sysmex Corporation, Kobe, Japan). The following hematological parameters were measured: hemoglobin, mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), red blood cells width (RDW), reticulocyte count, white blood cells, neutrophil, and platelet count. Biochemical blood tests performed included the measurement of lactate dehydrogenase (LDH), creatinine, urea, total bilirubin, aspartate aminotransferase and alanine aminotransferase and were determined using a Cobas C11 equipment (Roche Diagnostics, Basel, Switzerland) and Mindray BA-88 A (Mindray, Shenzhen, China). Hematological and biochemical parameters considered for each participant were an average of, at least, three different time-point measurements, performed in steady state periods. Patients were considered to be in steady state if they were afebrile, did not receive a blood transfusion nor experienced any vaso-occlusive episode during the previous three months. The patients’ anemia severity was classified as mild, moderate or severe, according to their level of hemoglobin and age as discriminated by the WHO guidelines [23].
Genotyping
Genomic DNA was isolated from peripheral blood sample of each patient using the QIAamp DNA Blood Mini Kit (Qiagen GmbH, Hilden, Germany) according to the manufacturer’s recommendations. DNA samples were quantified using the Qubit™ dsDNA HS fluorometric assay (ThermoFisher Scientific Inc., Waltham, MA, USA) and stored at 4ºC. The genotyping of twelve polymorphic regions in three putative hemolysis modifier genes (CD36, VCAM1 and NOS3) was performed using PCR based methodologies with customized primers (Supplementary Table 1).
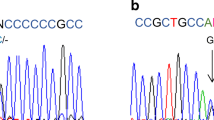
CD 36 gene genotyping
The 5’UTR and the exon 10 of the CD36 gene were amplified in two fragments of 314 and 390 bp, respectively. To genotype the first one, automated Sanger sequencing reactions were performed using the commercial kit BigDye Terminator v 1.1. Cycle Kit (Applied Biosystems) according to the manufacturer’s instructions, in a Biometra Thermocycler. Fluorescent signals and strand sizes were then discriminated through capillary electrophoresis in the automated sequencer 3130XI Genetic Analyzer (Applied Biosystem), and results were analyzed using FinchTV v1.4.0 software (Geospiza, Inc.). The second PCR fragment was used to characterize the SNP rs3211938 by RFLP using the Nde I endonuclease (ThermoFisher Scientific). The presence of the rs3211938_T allele gives rise to two fragments of 144 and 246 bp; the presence of the rs3211938_G allele did not result in fragment restriction. The reaction products were resolved in 2% agarose gels and stained with ethidium bromide.
VCAM1 gene promoter genotyping
VCAM1 gene promoter was amplified in an 860 bp PCR fragment, which was Sanger sequenced as described above.
NOS3 gene genotyping
Three polymorphic regions in NOS3 gene were analyzed. The rs2070744 located at the gene promoter was characterized by PCR amplification of a 244 bp DNA fragment followed by restriction with the endonuclease Nae I. The presence of the rs2070744_C allele gives rise to two fragments of 168 and 76 bp. Reaction products were resolved in 2% agarose gels stained with ethidium bromide. The variable number of tandem repeats (VNTR) in intron 4 was characterized by PCR. Post-amplification, PCR products were evaluated on ethidium bromide stained 3% agarose gels. Fragment sizes of 169, 196, and 223 bp corresponding to NOS3 alleles 4a, 4b, and 4c, originated by the amplification of 4x, 5x or 6x the 27 bp repeat, respectively, were observed. The SNP rs1799983, located in exon 7, was studied by PCR-RFLP. The PCR amplified fragments of 248 bp were digested with the endonuclease Mbo I. The presence of the T allele gives rise to two fragments of 158 and 90 bp. Reaction products were resolved in 2% agarose gels stained with ethidium bromide.
Haplotype reconstruction
Haplotype reconstruction was performed using PHASE software v2.1 according to the developer’s instructions (http://stephenslab.uchicago.edu/phase/download.html) [24, 25]. Haplotypes were reconstructed for genetic variants within the VCAM1 promoter (rs1409419, rs3917024, rs3917025, rs3783598, rs1041163, rs3783599), NOS3 (rs2070744, intron 4_VNTR, rs1799983) and for genetic variants located at CD36 promoter (rs1984112 and rs1413661).
In silico analysis
Population allele and genotype frequencies were listed for each observed variant using Ensembl website (www.ensembl.org), [26]. SNPs’ sequences were retrieved using the NCBI SNP search engine (http://www.ncbi.nlm.nih.gov/snp).
Statistical analysis
The statistical analysis was performed using the SPSS software (IBM Corp. Released 2018. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp). For descriptive analysis, continuous variables were represented as mean and standard deviation, median, minimum, and maximum values. To evaluate the Gaussian distribution of variables, Shapiro-Wilk normality tests were applied. Analyses involving numerical and continuous variables with normal and/or homogeneous distribution were performed using parametric ANOVA (post hoc-Hochberg) and independent t-tests. For variables that do not follow the normal distribution, the Mann-Whitney test was applied. Regarding the analysis of categorical variables, contingency tables were constructed, and the Chi-square test or Fisher’s exact test were calculated. Statistical significance was defined as p-value < 0.05. The genetic variants analyzed in our study were evaluated for potential association with clinical, hematological, and biochemical parameters. The dominant and codominant genetic test models were applied, whether individually or as part of specific haplotypes. Only polymorphisms with a minor allele frequency (MAF) ≥ 3% were considered for the association studies. The Pearson correlation method was used to evaluate the relationship between the variables “number of hospitalizations” and “number of transfusions”.
Results
Population description - clinical and hematological phenotypes
This study was performed on 200 SCA patients, age ranging between 3 and 12 years old, 97 males, 103 females, living in Angola and followed-up in Hospital Pediátrico David Bernardino, Luanda, or Hospital Geral do Bengo, Caxito. Their hematological and biochemical phenotypes characterized in steady state condition, anemia severity according to WHO guidelines [23], and clinical phenotypes including their SCA first clinical manifestation and other clinical adverse events, are shown in Table 1.
On average, children presented their first disease manifestation at the age of 14.2 months (median 8, maximum of 96 months). A four-year-old child had not yet presented any manifestation related to the disease. He was diagnosed as SCA due to a neonatal screening performed outside Angola. Dactylitis was the most frequent first disease expression (observed in 68.5% of the cases), followed by the vaso-occlusive pain crisis (23.5%) and severe anemia (7.5%). Other typical disease manifestations were observed in these patients, such as jaundice (n = 54, 27.5%), hepatomegaly (n = 35, 17.5%), splenomegaly (n = 21, 10.5%), osteomyelitis (n = 6, 3%) and overt stroke (n = 6, 3.0%).
As expected, these children have a chronic hemolytic anemia, detected by a diminution of the number of RBCs (2.9 ± 0.6 × 1012/L) and hemoglobin level (7.4 ± 1.0 g/dL) and a high level of serum hemolytic markers, LDH (430.7 ± 155.5 U/L), total bilirubin (1.5 ± 1.4 mg/dL), as well as higher reticulocyte count (10.3 ± 4.3%). To better characterize their chronic anemia, we classified its severity as mild (Hb between 11 and 11.4 g/dL), moderate (Hb between 8.0 and 10.9 g/dL), and severe (Hb bellow 8.0 g/dL), accordingly to WHO guidelines for children between 5 and 11 years old [23]. Based on these criteria none of the children revealed a mild anemia, 48/200 (24%) have moderate anemia, and 152/200 (76%) have severe anemia.
Most children (71.5%) have already required blood transfusions; an average of 0.4 transfusion per year of life was administrated. However, for some children a greater number of blood transfusions per year was needed (maximum 30 events over 8 years of life). On the other hand, fifty-seven of the 200 SCA children (28.5%) have never been transfused. It was observed that children with severe anemia required a larger number of blood transfusions per year (mean 0.436 ± 0.541 events) in comparison with children with moderate anemia (mean 0.168 ± 0.271 events), p < 0.001. In addition, children with severe anemia have a larger number of hospitalizations per year (mean 0.525 ± 0.518) in comparison with children with moderate anemia (0.297 ± 0.362), p < 0.001. Furthermore, it was also observed that children with severe anemia have a larger probability of displaying jaundice, Odds Ratio = 3.231 [C.I. 95% = 1.286–8.117].
Genetic findings
Twelve genetic variants (SNPs, indel, and VNTR) were characterized in VCAM1, CD36 and NOS3 genes and their allelic and genotype frequencies were calculated and are presented in Table 2. These results were compared to the reported in 1000 Genomes Project Consortium, phase 3 (Ensembl, released 105), [26]. In addition, we were able to reconstruct 16 haplotypes, which are presented in Supplementary Table 2. All studied polymorphisms were in Hardy-Weinberg equilibrium except for the rs3211938 in the CD36 gene, and rs1409419 and rs3917025 in the VCAM gene promoter.
Association of genetic variants with hematological, biochemical, and clinical phenotypes
The association studies were performed between the genetic variants as well as haplotypes (both with the minor frequency of ≥ 3%) and the hematological, biochemical, and clinical manifestations presented in Table 1. The dominant and codominant genetic test models were applied, and the statistically significant results are shown in Table 3.
Concerning the CD36 gene, genotypes containing at least one promoter variant, the rs1984112 (AG + GG) or rs1413661 (GC + CC), were significantly associated with lower levels of hemoglobin (p = 0.031 and p = 0.022, respectively), thus both are responsible for worsening anemia. Moreover, when using the codominant genetic test model, genotypes containing the rs1413661_C variant were associated with a larger number of hospitalizations per year (p = 0.021). In addition, these genotypes were also found associated with a greater need of blood transfusions per year (p = 0.008), however this observation has a strong positive correlation (+ 0.787; p < 0.001) with the higher hospitalization rate.
Regarding the association studies performed between the genetic variants and the levels of hemolytic markers (LDH, total bilirubin, and reticulocyte count), LDH was the only biochemical marker that revealed a significant association with some genetic variants, probably because it is a more proximal marker related with intravascular hemolysis. It was observed that one genetic alteration in VCAM1 gene promoter was improving the intravascular hemolysis, since genotypes containing the C allele at rs1041163 (TC + CC) were associated with lower levels of LDH (p = 0.014). Conversely, in NOS3 gene, genotypes containing the C allele at rs2070744 (TC + CC) were associated with higher levels of LDH (p = 0.047), thus worsening intravascular hemolysis.
A similar result was obtained when the two different alleles of the SNP rs2070744 were analyzed in the context of specific haplotypes in NOS3 gene. The NOS3_ Haplotype V (which includes rs2070744_C allele + VNTR_4b allele + rs1799983_G allele) was associated with higher LDH levels (p = 0.046), whereas the NOS3_haplotype II (which includes rs2070744_T allele + VNTR_4b allele + rs1799983_G allele) was associated with lower LDH levels (p = 0.034). The NOS3 rs207074_TC and CC genotypes, in addition to being associated with a higher hemolytic rate, were also associated with a greater number of hospitalizations/year (p = 0.008). The same was observed for NOS3_haplotype V, that includes the C allele, when comparing with other NOS3 haplotypes (p = 0.020).
Discussion
SCA, despite being a monogenic disease, shows a remarkable high clinical heterogeneity due to environmental and genetic modifier factors. The latter may be specific of certain populations or ethnic groups, and there is a concerning lack of knowledge of these factors in Africa, namely in Angola, where the disease is highly prevalent. In this study, our results revealed that in Angolan SCA children the hemolytic rate is clearly modulated by genetic modifiers related with NO metabolism, a natural gas that regulates the vascular tonus due to its potent vasodilation and antiadhesive properties. Concerning the variants studied in NOS3 gene, we observed that those located in the promoter seems to be the most important considering their modifier effect. The most frequent allele and genotype of SNP rs2070744 (T allele frequency of 0.902; TT genotype frequency of 0.810) revealed to have a protective effect on hemolysis as they were associated with lower levels of serum LDH. This association was validated by observing that NOS3_haplotype II (that contains rs2070744_T allele + VNTR_4b allele + rs1799983_G allele) was also associated with lower LDH when compared with other haplotypes in NOS3. Conversely, NOS3_haplotype V (that contains rs2070744_C allele + VNTR_4b allele + rs1799983_G allele) was significantly associated with higher LDH levels, reflecting a more severe hemolytic rate. In agreement, the rs2070744_C allele was also observed as a risk factor for hospitalizations. These results agree with other studies already reported in different populations, which have also classified this SNP as a modifier of various manifestations of SCD. In fact, the T allele of rs2070744 was reported as protective of SCA hemolysis since it was associated with lower bilirubin levels in a study performed in pediatric SCA patients living in Portugal but mostly of sub-Saharan African ancestry [18]. On the other hand, the C allele of this SNP was associated to several adverse SCD subphenotypes. For instance, it was associated with an increased susceptibility to acute chest syndrome in SCD African-American adult females [27]. It was also observed that Brazilian SCD patients with homozygosity for the C allele tended to have a severe clinical phenotype with increased pain events [28], while in adult Egyptian SCD patients it increased the incidence of vaso-occlusive crises and acute chest syndrome [29]. This SNP was also associated with an increased prevalence of SCD proliferative retinopathy in adult Greek SCD patients [30]. Moreover, in Ghana, SCD patients with rs2070744_TC or CC genotypes had a higher risk of developing leg ulcers and other complications associated with the disease [31]. In India, this SNP was linked to more severe SCA phenotypes, defined by a Severity Index ≥ 6.1, which was calculated based on frequency of painful crises, hospitalization, blood transfusion, infection and specific complications occurring since birth [32]. Considering our results and all the aforementioned reported observations, we can reinforce the role of NOS3 rs2070744 as a modulator of NO metabolism in SCA patients, being its C variant a risk factor that worsens the hemolytic phenotype as well as other several adverse SCA clinical manifestations.
A significant interethnic disparity in the genomic distribution of NOS3 clinically relevant polymorphisms among different populations of the world has been reported. Concerning the rs2070744, the variant allele C is more common in Caucasians (42.0%) than in African-Americans (17.5%) or Asians (13.8%) [33]. In addition, this C variant is found with a low frequency (14%) in general African population (1000 Genomes Project, phase 3) [26]. In agreement with these observations, our Angolan SCA patients have an even lower frequency of the rs2070744_C allele (9.8%). Therefore, we can hypothesize that the rs2070744_C allele have achieved a lower frequency on the African continent due to a negative selective pressure performed together by SCA and other frequent severe pathologies in Africa, in which this SNP is also a risk factor, such as Essential Hypertension [34], Chronic Kidney Failure and End-Stage Renal Disease [35].
Because in SCA there is a generalized state of inflammation, endothelial cells, both of large and small blood vessels, highly express cell surface VCAM-1 following cytokine stimulation. Sickle RBCs have a propensity to adhere to endothelial VCAM-1 via Very Late Antigen-4 expressed on their membrane surface [14]. Thus, it has been accepted that VCAM1 gene variants could be modulators of phenotypic differences in SCA, and several polymorphisms in VCAM1 covering both the gene and its promoter have already been studied in the context of this pathology [16,17,18,19,20]. Amongst the six VCAM1 promoter variants investigated in our study, the rs1041163 T > C stands out. We have found that patients with the TC or CC genotype have a significantly lower LDH level, suggesting a protective role on chronic hemolysis for this variant. Aligned with its beneficial effect, we have found a significantly higher frequency of this variant in our Angolan SCA patients (TC genotype frequency 0.387; CC genotype frequency 0.060) than in the general African population described in 1000 Genomes Project Consortium, phase 3 (TC genotype frequency 0.292; CC genotype frequency 0.038), (p = 0.011). This discrepancy in genotype frequencies is even more evident (p < 0.001) when comparing our data with what is described for the Yoruba population (with a similar ancestry as Angolan population): TC genotype frequency 0.352, CC genotype frequency 0.018 [26]. These observations are consistent with an enrichment of the SCA African population with the protective VCAM1 rs1041163_C allele.
In SCA, the immature form of RBCs (reticulocytes), which highly express CD36 on the cell surface membrane, are released into the circulation and are consequently implicated in adhesiveness to the endothelial cells by binding to their extracellular matrix proteins. Recently, a study has proven that patients with SCA had significantly more CD36-positive cells than the normal controls, and that this expression was higher in crises than in steady state [22]. For this reason, the interaction of CD36 with the endothelial cells seems to be a potential mechanism by which sickle RBCs adhesion may contribute to worsen SCA hemolytic anemia. Considering this hypothesis, we have characterized three SNPs within CD36 gene and correlated them with anemia severity and level of hemolysis. Our results have shown that the two SNPs located at the gene promoter, rs1984112A > G and rs1413661G > C, are both modulators of anemia severity (Table 3). We have found that patients who have CD36 genotypes containing at least one of these variants (rs1984112_AG or GG) or (rs1413661_GC or CC) have significantly lower level of hemoglobin, and a more severe anemia. These SNPs, despite being located close to each other (only 82 bp apart) seem to exert their effect independently. The first is already known as a SCA modulator in other populations, whereas the latter is here reported for the first time. In fact, in the literature we can find, at least, two reports showing association of the rs1984112_G allele with higher levels of reticulocyte count in SCA, a consequence of an increased chronic hemolytic status [18, 36]. Therefore, our results validate literature reports and confirm that the inheritance of the rs1984112_G allele is a risk factor in SCA pathogenesis, particularly regarding anemia and hemolysis. In addition, other authors have attributed modifying functions to this SNP rs1984112 concerning other pathologies or characteristics, such as modulator of cholesterolemia [37], and of tissue vitamin E uptake [38].
Regarding the second CD36 promoter SNP studied, the rs1413661, as far as we know, there are no reports in the literature about its possible modulatory effect in the context of any pathology. Thus, our study describes for the first time the association of the rs1413661_C allele with lower hemoglobin levels and consequently with severe anemia in the Angolan background of SCA. In addition, we also conclude that the C variant of this SNP is a risk factor for SCA clinical severity since patients who have this variant need more hospitalizations and blood transfusions. To validate these results another SCA affected population should be studied, and to identify its underlying mechanism functional studies should be performed. The hypothesis that this SNP has the aforementioned risk effect is supported by our SCA population having the rs1413661_C allele frequency of 0.670 which is significantly lower (p < 0.001) when compared with what is described for the general Yoruba population (C allele frequency of 0.870) [26]. This evidence might be due to a consequently negative selective pressure under SCA background.
The third SNP studied in CD36 gene, the rs3211938T > G, is located in exon 10 and is a nonsense mutation, giving rise to a premature stop codon, p.Tyr325Ter. It is known that mRNAs containing a premature stop codon elicits the nonsense mediated decay (NMD) mechanism to prevent truncated proteins to be synthetized [39]. Many nonsense mutations have been described in CD36 gene and, interestingly, this type of mutations is particularly common in some African populations from areas where malaria is endemic. Since CD36 is also an endothelial receptor for adhesion of Plasmodium falciparum infected erythrocytes, its absence at RBC surface would suggest a protective effect against severe manifestations of this infectious disease. Nevertheless, absence of CD36 and their consequences on malaria severity are still controversial and remains to be unveiled [40,41,42]. In addition, some authors suggest that the nonexpression of CD36 on reticulocytes and mature RBCs does not modify the clinical course of patients with SCA, because their vaso-occlusion requires the expression modulation of more than one type of adhesion molecules [43]. We have found in our SCA patients a lower frequency of the rs321198_G allele (0.193) comparing to what is reported in 1000 Genomes Project, phase 3, for the Yoruba general population (G allelic frequency of 0.292; p = 0.029) [26]. In addition, no association was found between this SNP and anemia, hemolytic severity or other SCA related deleterious event.
In our study, none of the enrolled SCA patients has ever been treated with HU. This medicine is a ribonucleotide reductase inhibitor largely used for SCD therapy in developed countries. It has an anti-inflammatory effect, increases the level of HbF, decreases expression of RBCs and endothelial-cell adhesion molecules, works as a NO donor, reduces reticulocyte, leucocyte and platelet counts and decreases the expression of the CD36 gene even for months following HU treatment [44,45,46]. Thus, we believe that our genotype/phenotypes association results are not biased by that environmental factor, contrary to what may happen in similar studies performed in SCA populations living in developed countries. Nevertheless, our results should be confirmed on a larger sample size of other similar SCA African/Bantu population, namely in what concerns the novel rs1413661G > C functional effect. Genetic variants that have modulatory effects on SCA, namely mediators of sickle RBCs adhesion to endothelium, may be potential pharmacological targets to combat these specific SCA complications.
Conclusion
Here, for the first time in the Angolan population, we were able to identify genetic modifiers related with red blood cell vascular adhesion and vascular tonus that influence the anemia severity, hemolysis level, and hospitalization rate in SCA children, contributing to the phenotypic variability of SCA in Angola. We validated the role of NOS3 rs2070744 as a modulator of NO metabolism in SCA patients, being its C variant a risk factor that worsens the hemolytic phenotypes and increases the need for hospitalizations. Concerning vascular cell adhesion modulation, we found the rs1041163_C allele in VCAM1 associated with a favorable lower hemolytic rate. Furthermore, the CD36 gene promoter variants (rs1984112 and rs1413661) showed a significant impact on anemia severity. Particularly, the rs1413661_C allele revealed to be a risk factor for severe anemia, as it was associated with lower hemoglobin levels, increased number of hospitalizations and transfusions. This is the first report associating this SNP with SCA hematological heterogeneity. Consequently, further studies in African populations are needed, not only for confirmation purposes, but also to assess the effect of these genetic modifiers on other adverse clinical manifestations of SCA, leading to a better understanding of the inter- and intra-individual clinical variability of this disease.
References
Piel FB, Steinberg MH, Rees DC (2017) Sickle Cell Disease. N Engl J Med 376:1561–1573. https://doi.org/10.1056/NEJMra1510865
Kato GJ, Piel FB, Reid CD et al (2018) Sickle cell disease. Nat Rev Dis Prim 4:18010. https://doi.org/10.1038/nrdp.2018.10
Grosse SD, Odame I, Atrash HK et al (2011) Sickle cell disease in Africa: a neglected cause of early childhood mortality. Am J Prev Med 41:S398–405. https://doi.org/10.1016/j.amepre.2011.09.013
Williams TN (2016) Sickle Cell Disease in Sub-Saharan Africa. Hematol Oncol Clin North Am 30:343–358. https://doi.org/10.1016/j.hoc.2015.11.005
Andrade V, Arango M, Abreu S, Flores I(2014) One Company’s Angola Sickle Cell Program. SPE Int. Conf. Heal. Safety, Environ. D031S054R004
Serjeant GR (2013) The natural history of sickle cell disease. Cold Spring Harb Perspect Med 3:a011783. https://doi.org/10.1101/cshperspect.a011783
Santos B, Delgadinho M, Ferreira J et al (2020) Co-Inheritance of alpha-thalassemia and sickle cell disease in a cohort of Angolan pediatric patients. Mol Biol Rep 47:5397–5402. https://doi.org/10.1007/s11033-020-05628-8
Schnog JB, Duits AJ, Muskiet FAJ et al (2004) Sickle cell disease; a general overview. Neth J Med 62:364–374
Kato GJ, Gladwin MT, Steinberg MH (2007) Deconstructing sickle cell disease: reappraisal of the role of hemolysis in the development of clinical subphenotypes. Blood Rev 21:37–47. https://doi.org/10.1016/j.blre.2006.07.001
Oliveira-Paula GH, Lacchini R, Tanus-Santos JE (2016) Endothelial nitric oxide synthase: From biochemistry and gene structure to clinical implications of NOS3 polymorphisms. Gene 575:584–599. https://doi.org/10.1016/j.gene.2015.09.061
Gee BE, Platt OS (1995) Sickle reticulocytes adhere to VCAM-1. Blood 85:268–274
White J, Lancelot M, Gao X et al (2020) Cross-sectional analysis of adhesion in individuals with sickle cell disease using a standardized whole blood adhesion bioassay to VCAM-1. Blood Cells Mol Dis 81:102397. https://doi.org/10.1016/j.bcmd.2019.102397
Dworkis DA, Klings ES, Solovieff N et al (2011) Severe sickle cell anemia is associated with increased plasma levels of TNF-R1 and VCAM-1. Am J Hematol 86:220
Wautier J-L, Wautier M-P (2020) Cellular and Molecular Aspects of Blood Cell-Endothelium Interactions in Vascular Disorders. Int J Mol Sci 21. https://doi.org/10.3390/ijms21155315
Hoppe C, Klitz W, Cheng S et al (2004) Gene interactions and stroke risk in children with sickle cell anemia. Blood 103:2391–2396. https://doi.org/10.1182/blood-2003-09-3015
Taylor JG 6th, Tang DC, Savage SA et al (2002) Variants in the VCAM1 gene and risk for symptomatic stroke in sickle cell disease. Blood 100:4303–4309. https://doi.org/10.1182/blood-2001-12-0306
Idelman G, Taylor JG, Tongbai R et al (2007) Functional profiling of uncommon VCAM1 promoter polymorphisms prevalent in African American populations. Hum Mutat 28:824–829. https://doi.org/10.1002/humu.20523
Coelho A, Dias A, Morais A et al (2014) Genetic variation in CD36, HBA, NOS3 and VCAM1 is associated with chronic haemolysis level in sickle cell anaemia: A longitudinal study. Eur J Haematol 92:237–243. https://doi.org/10.1111/ejh.12226
Silva M, Vargas S, Coelho A et al (2020) Biomarkers and genetic modulators of cerebral vasculopathy in sub-Saharan ancestry children with sickle cell anemia. Blood Cells Mol Dis 83:102436
Silva M, Coelho A, Vargas S, Faustino P (2022) VCAM1, HMOX1 and NOS3 differential endothelial expression may impact sickle cell anemia vasculopathy. Blood cells, Mol & Dis 93:102639. https://doi.org/10.1016/j.bcmd.2021.102639
Carden MA, Fasano RM, Meier ER (2020) Not all red cells sickle the same: Contributions of the reticulocyte to disease pathology in sickle cell anemia. Blood Rev 40:100637. https://doi.org/10.1016/j.blre.2019.100637
Abdul-Hussein HK, Al-Mammori HS, Hassan MK (2021) Evaluation of the expression of red blood cell CD36, interleukin-6 and interleukin-8 in sickle cell anemia pediatric patients. Cytokine 143:155534. https://doi.org/10.1016/j.cyto.2021.155534
WHO (2011) Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System. https://apps.who.int/iris/bitstream/handle/10665/85839/WHO_NMH_NHD_MNM_11.1_eng.pdf. Accessed 14 Jan 2022
Stephens M, Smith NJ, Donnelly P (2001) A new statistical method for haplotype reconstruction from population data. Am J Hum Genet 68:978–989
Stephens M, Scheet P (2005) Accounting for decay of linkage disequilibrium in haplotype inference and missing-data imputation. Am J Hum Genet 76:449–462
Howe KL, Achuthan P, Allen J et al (2021) Ensembl 2021. Nucleic Acids Res 49:D884–D891. https://doi.org/10.1093/nar/gkaa942
Sharan K, Surrey S, Ballas S et al (2004) Association of T-786 C eNOS gene polymorphism with increased susceptibility to acute chest syndrome in females with sickle cell disease. Br J Haematol 124:240–243. https://doi.org/10.1046/j.1365-2141.2003.04762.x
Vargas AE, da Silva MAL, Silla L, Chies JAB (2005) Polymorphisms of chemokine receptors and eNOS in Brazilian patients with sickle cell disease. Tissue Antigens 66:683–690. https://doi.org/10.1111/j.1399-0039.2005.00506.x
Yousry SM, Ellithy HN, Shahin GH (2016) Endothelial nitric oxide synthase gene polymorphisms and the risk of vasculopathy in sickle cell disease. Hematology 21:359–367. https://doi.org/10.1080/10245332.2016.1142710
Armenis I, Kalotychou V, Tzanetea R et al (2017) Prognostic value of T786C and G894T eNOS polymorphisms in sickle cell disease. Nitric Oxide 62:17–23. https://doi.org/10.1016/j.niox.2016.11.002
Antwi-Boasiako C, Dzudzor B, Kudzi W et al(2018) Association between eNOS Gene Polymorphism (T786C and VNTR) and Sickle Cell Disease Patients in Ghana. Dis (Basel, Switzerland) 6:. https://doi.org/10.3390/diseases6040090
Nishank SS, Singh MPSS, Yadav R et al (2013) Endothelial nitric oxide synthase gene polymorphism is associated with sickle cell disease patients in India. J Hum Genet 58:775–779. https://doi.org/10.1038/jhg.2013.99
Tanus-Santos JE, Desai M, Flockhart DA (2001) Effects of ethnicity on the distribution of clinically relevant endothelial nitric oxide variants. Pharmacogenetics 11:719–725. https://doi.org/10.1097/00008571-200111000-00011
Gamil S, Erdmann J, Abdalrahman IB, Mohamed AO (2017) Association of NOS3 gene polymorphisms with essential hypertension in Sudanese patients: a case control study. BMC Med Genet 18:128. https://doi.org/10.1186/s12881-017-0491-7
Elsaid A, Samir Eid O, Said SB, Zahran RF (2021) Association of NOS3 (rs 2070744) and SOD2Val16Ala (rs4880) gene polymorphisms with increased risk of ESRD among Egyptian patients. J Genet Eng Biotechnol 19:158. https://doi.org/10.1186/s43141-021-00260-w
Kalai M, Dridi M, Chaouch L et al (2017) The role of rs1984112_G at CD36 gene in increasing reticulocyte level among sickle cell disease patients. Hematology 22:178–182. https://doi.org/10.1080/10245332.2016.1253253
Rodrigues AC, Sobrino B, Genvigir FDV et al (2013) Genetic variants in genes related to lipid metabolism and atherosclerosis, dyslipidemia and atorvastatin response. Clin Chim Acta 417:8–11. https://doi.org/10.1016/j.cca.2012.11.028
Lecompte S, Szabo de Edelenyi F, Goumidi L et al (2011) Polymorphisms in the CD36/FAT gene are associated with plasma vitamin E concentrations in humans1–3. Am J Clin Nutr 93:644–651. https://doi.org/10.3945/ajcn.110.004176
Kurosaki T, Maquat LE (2016) Nonsense-mediated mRNA decay in humans at a glance. J Cell Sci 129:461–467. https://doi.org/10.1242/jcs.181008
Fry AE, Ghansa A, Small KS et al (2009) Positive selection of a CD36 nonsense variant in sub-Saharan Africa, but no association with severe malaria phenotypes. Hum Mol Genet 18:2683–2692. https://doi.org/10.1093/hmg/ddp192
Aitman TJ, Cooper LD, Norsworthy PJ et al (2000) Malaria susceptibility and CD36 mutation. Nature 405:1015–1016. https://doi.org/10.1038/35016636
Cabrera A, Neculai D, Kain KC (2014) CD36 and malaria: friends or foes? A decade of data provides some answers. Trends Parasitol 30:436–444. https://doi.org/10.1016/j.pt.2014.07.006
Lee K, Gane P, Roudot-Thoraval F et al (2001) The nonexpression of CD36 on reticulocytes and mature red blood cells does not modify the clinical course of patients with sickle cell anemia. Blood 98:966–971. https://doi.org/10.1182/blood.v98.4.966
Cartron J-P, Elion J (2008) Erythroid adhesion molecules in sickle cell disease: effect of hydroxyurea. Transfus Clin Biol J la Soc Fr Transfus Sang 15:39–50. https://doi.org/10.1016/j.tracli.2008.05.001
Agrawal RK, Patel RK, Shah V et al (2014) Hydroxyurea in sickle cell disease: drug review. Indian J Hematol blood Transfus an Off J Indian Soc Hematol Blood Transfus 30:91–96. https://doi.org/10.1007/s12288-013-0261-4
McGann PT, Ware RE (2015) Hydroxyurea therapy for sickle cell anemia. Expert Opin Drug Saf 14:1749–1758. https://doi.org/10.1517/14740338.2015.1088827
Acknowledgements
We would like to thank all children and caregivers who accepted to participate in the study. We also would like to thank the CISA’s laboratory team for the hematological and biochemical analyses, and the Technology and Innovation Unit of DGH/INSA for Sanger sequencing analyses.
Funding
This work was partially supported by the Fundação Para a Ciência e a Tecnologia/Aga Khan Development Network, Grant number 330842553.
Author information
Authors and Affiliations
Contributions
Conceptualization: PF, APA and MB; Clinical data collection: BS; Clinical analyses and laboratorial molecular experiments: IG, MD, CG, and PL; Interpretation of results: IG, BS, MD, APA, MB and PF; Contribution to manuscript writing: PF, IG, MB, and APA. All authors have read and approved the final version of the manuscript and agree with the order of presentation of the authors.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interest to disclose.
Ethics approval
This study was approved by the Ethical Committee of Ministry of Health of Angola (CE. Nº 040/2018), the Ethical committee of ESTeSL (CE-ESTeSL-Nº.43-2018), INSA and IHMT. This study was performed in line with the principles of the Declaration of Helsinki of 1975, as revised in 2008.
Consent to participate
The aims and study procedures were explained to the children’s parents or legal guardians, and they provided informed written consent to their enrolment.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors Isabel Germano and Brígida Santos contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Germano, I., Santos, B., Delgadinho, M. et al. Genetic modulation of anemia severity, hemolysis level, and hospitalization rate in Angolan children with Sickle Cell Anemia. Mol Biol Rep 49, 10347–10356 (2022). https://doi.org/10.1007/s11033-022-07831-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07831-1