Abstract
In this study, we compared the long-term effects of different iron chelation regimens (deferoxamine, deferiprone, deferoxamine + deferiprone, and deferasirox) in preventing or reversing endocrinopathy (diabetes mellitus, hypothyroidism, or hypogonadism) and bone disease (measured through DEXA) in 165 adults with β-thalassemia major (TM) (mean age 39.9 ± 8.3 years, 43 % males). After five consecutive years of therapy, patients on deferasirox had the highest decrease in the prevalence of any endocrinopathy compared to other chelators which either had no change (deferiprone and deferoxamine) or had an increase (deferoxamine + deferiprone), p = 0.015. This was attributed to a lower proportion of patients on deferasirox developing new-onset endocrinopathy and higher proportion showing reversal of disease, compared to other chelators. A serum ferritin level of >1300 ng/mL predicted the development of new endocrinopathy (p = 0.025) while a level of <200 ng/mL predicted reversal of existing endocrinopathy (p = 0.147). A significant increase in mean BMD T-score (p < 0.001) and a considerable decrease in osteoporosis prevalence were observed in patients receiving deferasirox but not other chelators. Iron chelation therapy with deferasirox has a role in the prevention of endocrinopathy and reversal of existing disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endocrinopathies are common in regularly transfused patients with β-thalassemia major (TM) and have been closely associated with transfusional iron overload. Recent studies report the development of at least one endocrinopathy in children before they reach 10 years of age, with a rising incidence throughout adulthood when around two thirds of adults can have at least one form of endocrine dysfunction [1–4]. Iron accumulation in endocrine glands such as the pituitary and pancreas has been observed in magnetic resonance imaging (MRI) studies and was associated with gland dysfunction [5, 6]. Elevated serum ferritin levels have also been associated with the development of endocrine disease [7]. Osteoporosis is another concern in TM patients as it is commonly associated with adverse outcomes including pain, deformity, and increased fracture risk [8]. Although the pathogenesis of bone disease in these patients is multifactorial, iron toxicity has been strongly implicated [8]. These observations suggest a role for iron chelation therapy in the prevention or management of endocrine and bone disease, although studies that specifically addressed these effects remain limited, especially ones comparing different iron chelation regimens. In this study, we aimed to evaluate and compare the effects of different iron chelators on the development or reversal of endocrine and bone disease in a group of TM adults that received their respective chelators for at least 5 years. Such data would increase our understanding of the effects of iron chelation therapy on essential organ systems beyond the liver and heart, where most available studies were concentrated.
Material and methods
This was a retrospective cohort study of all TM adults attending our center that have remained on the same chelation therapy for a minimum of 5 years. For all patients demographic data at the start of observation (baseline), type of chelator, and average serum ferritin (SF) across the 5-year period were collected. A single endocrinologist evaluated patients at the start and end of observation after 5 years to assess for the presence and absence of endocrinopathies which were defined as follows:
-
Diabetes mellitus was defined as fasting blood glucose >126 or >200 mg/dL at any time or fasting blood glucose >126 mg/dL in an oral glucose tolerance test (OGTT) or a second hour blood glucose level >200 mg/dL in an OGTT.
-
Hypogonadism was defined (in males) as testosterone level <230 ng/dL (8 nmol/L) in association with specific symptoms and signs of hypogonadism like reduced libido, decreased spontaneous erections, declining testicular volume, loss of body hair, or decreased muscle mass. In females, hypogonadism was defined as low ovarian estrogen and progesterone levels in association with oligo-amenorrhea.
-
Hypothyroidism was defined as low levels of fT3 and fT4 (with or without a rise in serum level of thyroid stimulating hormone [TSH], to define primary or secondary etiology)
-
Osteoporosis was defined according to the WHO criteria (WHO Technical Report, ISCD Official Position Paper 2007) as a low T-score level (<2.5 SD) at the lumbar spine or femoral neck on a dual-energy X-ray absorptiometry (DEXA) examination while a T-score between −1 and−2.5 was defined as osteopenia and a T-score >−1 was considered normal.
For each patient, three measurements of bone mineral density (BMD) 18 months apart were conducted during the 5-year span. These were conducted on the femoral neck and lumbar spine using DEXA (Hologic Bone Densitometer QDR, Hologic Inc., Waltham, MA, USA).
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. A written informed consent was obtained from all subjects participating in this study.
Statistical analysis
Descriptive analysis is provided as means ± standard deviations, medians, or percentages. Bivariate comparisons were made using the chi-squared and Fisher’s exact tests for categorical variables and the independent samples t test, Mann–Whitney U test, and Kruskal–Wallis test for continuous variables. Receiver operating characteristic (ROC) curve analysis was used to identify serum ferritin levels that best predict the development of new endocrinopathy by identifying levels with the highest sum of sensitivity and specificity. Paired samples t test was used to analyze longitudinal changes in BMD for each iron chelator. All p values are two sided with the level of significance set at <0.05.
Results
A total of 165 patients were included in this analysis. Their mean age was 39.9 ± 8.3 years (range 20–68) including 71 (43 %) males. A total of 40 (24.2 %) patients were receiving deferoxamine (mean dose over the 5-year study period 37.4 mg/kg/day), 18 (10.9 %) were receiving deferiprone (mean dose 74.7 mg/kg/day), 50 (30.3 %) were receiving simultaneous deferoxamine + deferiprone (mean dose deferoxamine 30.9 mg/kg/day and deferiprone 56 mg/kg/day), and 57 (34.5 %) were receiving deferasirox (mean dose 26.3 mg/kg/day). The median serum ferritin level over the 5-year observation period was 555 ng/mL (range 63–6140): deferoxamine 469 ng/mL, deferiprone 834 ng/mL, deferoxamine + deferiprone 595 ng/mL, and deferasirox 476 ng/mL (p = 0.110).
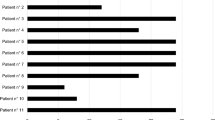
Analysis of endocrine disease
At baseline, a total of 121 (73.3 %) patients had an endocrinopathy, 16 (9.7 %) had diabetes, 65 (39.4 %) had hypothyroidism, and 108 (65.5 %) had hypogonadism. There were no statistically significant differences in the prevalence of any of the evaluated endocrinopathies between different iron chelators at baseline (Fig. 1). However, after five consecutive years of therapy on each iron chelator, a statistically significant difference was noted between different iron chelators with regard to the percentage change in endocrinopathy prevalence (Fig. 2). Patients on deferasirox therapy had the highest decrease in the prevalence of any endocrinopathy (−1.8 %) compared to other chelators which either had no change (deferiprone and deferoxamine) or an increase (+6 % for deferoxamine + deferiprone), p = 0.015. Looking at individual endocrinopathies, patients on deferasirox had a decrease in the prevalence of hypogonadism (−3.4 %) and diabetes (−1.8 %), while no change was noted for hypothyroidism. Patients on deferoxamine had a decrease in the prevalence of hypothyroidism (−2.5 %), yet an increase in the prevalence of diabetes (+2.5 %) and hypogonadism (+5 %). Patients on deferiprone had an increase in the prevalence of diabetes (+5.5 %) and no change in the prevalence of other endocrinopathies. Patients on deferoxamine + deferiprone had an increase in the prevalence of all endocrinopathies: +2 % for diabetes, +6 % for hypothyroidism, and +4 % for hypogonadism (Fig. 2).
Table 1 summarizes the incident cases that explain the differences in prevalence after 5 years. Upon evaluation of patients who did not have the endocrinopathy at baseline, one patient on each of deferoxamine, deferiprone, and deferoxamine + deferiprone developed diabetes, while no new cases were observed on deferasirox. One patient on each of deferoxamine and deferasirox newly developed hypothyroidism, three patients did so on deferoxamine + deferiprone, and none did on deferiprone. Two patients developed new onset of hypogonadism on each of deferoxamine and deferoxamine + deferiprone while none did on deferiprone or deferasirox. Upon evaluation of patients who already had the endocrinopathy at baseline, one patient on deferasirox had reversal of diabetes, one had reversal of hypothyroidism, and two had reversal of hypogonadism. Two patients on deferoxamine had reversal of hypothyroidism. None of the patients on deferiprone or deferoxamine + deferiprone had reversal of their endocrinopathy.
Neither age nor gender had a statistically significant role in the development of new endocrinopathies or reversal of existing ones (Table 2). However, there was a statistically significant difference in median serum ferritin level between patients who developed new endocrinopathy (1471 ng/mL) and those who did not (562 ng/mL), p = 0.023 (Table 2). On ROC curve analysis, a serum ferritin level of >1300 ng/mL was the best predictor for the development of new endocrinopathy within 5 years in patients who did not have an existing one at baseline (area under the curve [AUC]: 0.810, p = 0.025) (Fig. 3). The serum ferritin level of <200 ng/mL was the best predictor for reversal of endocrinopathy in those who had an existing one at baseline, although this prediction did not reach statistical significance (AUC 0.746, p = 0.147). To determine whether the observed effects of iron chelation therapy on the prevention of the development of new endocrinopathy can be explained by differences in serum ferritin control, we compared the proportion of patients with a serum ferritin level >1300 ng/mL across the four chelation regimens and the values were as follows: deferoxamine (n = 6), 15 %; deferiprone (n = 6), 33.3 %; deferoxamine + deferiprone (n = 14), and 28 %; deferasirox (n = 7), 12.3 % (p = 0.080).
Analysis of bone disease
In the analysis of mean BMD change between the farthest two measurements apart (36 months), a significant change (favorable increase) in mean BMD T-score SD at the femoral neck was observed in patients receiving deferasirox (−2.17 ± 1.03 to−2.01 ± 0.66, p < 0.001) but not other chelators: deferoxamine (−2.29 ± 1.13 to −2.45 ± 1.47, p = 0.969), deferiprone (−1.90 ± 1.05 to −2.06 ± 0.52, p = 0.984), deferoxamine + deferiprone (−2.16 ± 1.17 to −2.12 ± 0.98, p = 0.769). Similarly, a significant change in mean BMD T-score SD at the lumbar spine was observed in patients receiving deferasirox (−2.84 ± 1.11 to −2.12 ± 0.78, p < 0.001) but not other chelators: deferoxamine (−2.92 ± 1.06 to −2.93 ± 0.90, p = 0.489), deferiprone (−2.54 ± 1.00 to −2.69 ± 0.67, p = 0.423), deferoxamine + deferiprone (−2.92 ± 1.21 to −2.55 ± 0.87, p = 0.516). Figure 4 illustrates prevalence of osteoporosis (−2.5 SD BMD T-score at the femoral neck or lumbar spine) for each chelator at the three evaluated time points, noting a considerable decrease in prevalence on deferasirox therapy but not other chelators.
Discussion
Our study confirmed that endocrinopathies are highly prevalent morbidities in TM patients, which should not to be dismissed. Data from earlier studies on Italian patients with TM showed prevalence rates for diabetes to be 5–17 %, hypothyroidism 11–31 %, and hypogonadism 44–65 % [1, 3, 9]. These rates are close to the prevalence of endocrinopathies at baseline in our study, with slight variations that may be attributed to the age at the time of assessment, variations in the assessment techniques, or variability of concomitant patient, disease, or treatment-related factors. The effect of iron overload was also apparent, with values >1300 ng/mL being predictive of the development of new morbidity. This threshold is relatively lower than what has been reported in earlier studies, which was often in excess of 2500 ng/mL [3, 7]. However, our study did not set a priori serum ferritin threshold for the analysis of its effects on outcomes [7], and we resorted to a ROC curve for identification of the best predictive cut-off in patients at risk (without pre-existing endocrinopathy). This finding calls for revisiting target iron control when prevention of endocrine disease is the desired outcome.
The differential effects of iron chelators on the development of new or reversal of existing endocrinopathy warrant further discussion. Very few studies reported longitudinal changes in endocrine disease with iron chelation therapy. Although the prevalence of endocrine disease was noted to decrease in the past 30 years with more optimal iron chelation and serum ferritin control [3], new cases in patients receiving iron chelation therapy continue to be observed. Data from early 2000 on patient cohorts mostly receiving deferoxamine reported incidence rates of 14 % for new onset of endocrinopathy with each 5 years of advancing age [4], in agreement with deferoxamine data in our study (∼17 % developed a new endocrinopathy although 3 % had reversal). A more recent study reported no significant changes in the prevalence of endocrine disease (diabetes, hypothyroidism, hypogonadism, hypoparathyroidism) in patients receiving deferasirox for a median duration of 6.5 years [9]. Our data support these protective effects of deferasirox towards the development of new endocrinopathies and further demonstrate that it is able to reverse the pathology in a subset of patients (∼6 % in those with existing disease). Earlier studies showed similar effects of reversal of endocrinopathy with aggressive chelation using the combination of deferoxamine + deferiprone or deferiprone + deferasirox [10, 11]. However, none of the patients on deferiprone monotherapy or deferoxamine + deferiprone in our study had reversal of endocrine disease, with the latter group having the highest incidence of new-onset disease (27.3 %). This latter observation may be a result of combination therapy being commonly reserved for patients with severe iron overload; and such patients may have had preclinical organ damage prior to inclusion in this study. Collectively, and when looking at the development of new endocrine disease as well as reversal of existing one, our data suggest a most favorable role for deferasirox therapy over other chelators. Deferasirox has shown consistent reduction in serum ferritin levels and liver iron concentration, being a surrogate of total body iron, over 5 years of therapy [12]. It has also shown favorable effects on liver pathology (reversal of fibrosis) and preservation of heart function concomitant with reduction of cardiac iron overload [13, 14]. Our data adds endocrine disease to the spectrum of such clinical benefits.
Favorable changes in BMD were also observed with deferasirox but not other chelators, with noted decrease in osteoporosis prevalence after 5 years of therapy. These effects resonate and confirm recently reported data showing similar effects of deferasirox on bone disease over a median duration of 6.5 years [9]. The effects of deferasirox on bone health may extend beyond amelioration of iron toxicity. Aside from the effects of iron overload, bone disease in TM patients is majorly driven by the underlying ineffective erythropoiesis and subsequent effects on the bone microenvironment [8]. A recent study on TM patients, showed that compared with other iron chelators, deferasirox therapy is associated with higher levels of circulating erythroid burst-forming units indirectly reflecting improved bone marrow activity [15]. Whether these effects contribute to subsequent improvement of low BMD merits further evaluation.
Our study is not without limitations. The incidence of change in endocrine status was restricted to a small proportion of patients from the study sample. We were unable to assess and account for the utilization of medications for the treatment of specific endocrinopathies or osteoporosis to realize whether these were unevenly distributed across chelator groups. However, as our patients are treated at a single center under the same management team, variations in the treatment of endocrinopathies are expected to be minimal. Similarly, we were unable to evaluate the effect of chelator dose on observed outcomes, although, similarly, extreme variations in management should be uncommon with most patients following label-indicated dosing recommendations for each chelator thus allowing for generalizability of data in similar practice. Lastly, we were not able to account for the effect of patient compliance to therapy and whether it can explain the differences in chelation effects.
In conclusion, our study demonstrated that endocrine and bone disease continue to pose a significant source of morbidity for patients with TM. Appropriate chelation therapy, however, has a role in the prevention of development of new morbidity and even reversal of existing disease. The favorable role of deferasirox therapy stands out in this context and merits further evaluation through clinical trials.
References
Borgna-Pignatti C, Rugolotto S, De Stefano P, Zhao H, Cappellini MD, Del Vecchio GC, Romeo MA, Forni GL, Gamberini MR, Ghilardi R, Piga A, Cnaan A (2004) Survival and complications in patients with thalassemia major treated with transfusion and deferoxamine. Haematologica 89:1187–1193
Habeb AM, Al-Hawsawi ZM, Morsy MM, Al-Harbi AM, Osilan AS, Al-Magamsi MS, Zolaly MA (2013) Endocrinopathies in beta-thalassemia major. Prevalence, risk factors, and age at diagnosis in Northwest Saudi Arabia. Saudi Med J 34:67–73
Gamberini MR, De Sanctis V, Gilli G (2008) Hypogonadism, diabetes mellitus, hypothyroidism, hypoparathyroidism: incidence and prevalence related to iron overload and chelation therapy in patients with thalassaemia major followed from 1980 to 2007 in the Ferrara Centre. Pediatr Endocrinol Rev 6(Suppl 1):158–169
Cunningham MJ, Macklin EA, Neufeld EJ, Cohen AR, Thalassemia Clinical Research N (2004) Complications of beta-thalassemia major in North America. Blood 104:34–39
Noetzli LJ, Panigrahy A, Mittelman SD, Hyderi A, Dongelyan A, Coates TD, Wood JC (2012) Pituitary iron and volume predict hypogonadism in transfusional iron overload. Am J Hematol 87:167–171
Noetzli LJ, Mittelman SD, Watanabe RM, Coates TD, Wood JC (2012) Pancreatic iron and glucose dysregulation in thalassemia major. Am J Hematol 87:155–160
Belhoul KM, Bakir ML, Saned MS, Kadhim AM, Musallam KM, Taher AT (2012) Serum ferritin levels and endocrinopathy in medically treated patients with beta thalassemia major. Ann Hematol 91:1107–1114
Haidar R, Musallam KM, Taher AT (2011) Bone disease and skeletal complications in patients with beta thalassemia major. Bone 48:425–432
Casale M, Citarella S, Filosa A, De Michele E, Palmieri F, Ragozzino A, Amendola G, Pugliese U, Tartaglione I, Della Rocca F, Cinque P, Nobili B, Perrotta S (2014) Endocrine function and bone disease during long-term chelation therapy with deferasirox in patients with beta-thalassemia major. Am J Hematol 89:1102–1106
Farmaki K, Tzoumari I, Pappa C, Chouliaras G, Berdoukas V (2010) Normalisation of total body iron load with very intensive combined chelation reverses cardiac and endocrine complications of thalassaemia major. Br J Haematol 148:466–475
Farmaki K, Tzoumari I, Pappa C (2011) Oral chelators in transfusion-dependent thalassemia major patients may prevent or reverse iron overload complications. Blood Cells Mol Dis 47:33–40
Cappellini MD, Bejaoui M, Agaoglu L, Canatan D, Capra M, Cohen A, Drelichman G, Economou M, Fattoum S, Kattamis A, Kilinc Y, Perrotta S, Piga A, Porter JB, Griffel L, Dong V, Clark J, Aydinok Y (2011) Iron chelation with deferasirox in adult and pediatric patients with thalassemia major: efficacy and safety during 5 years’ follow-up. Blood 118:884–893
Pennell DJ, Porter JB, Cappellini MD, Chan LL, El-Beshlawy A, Aydinok Y, Ibrahim H, Li CK, Viprakasit V, Elalfy MS, Kattamis A, Smith G, Habr D, Domokos G, Roubert B, Taher A (2012) Deferasirox for up to 3 years leads to continued improvement of myocardial T2* in patients with beta-thalassemia major. Haematologica 97:842–848
Deugnier Y, Turlin B, Ropert M, Cappellini MD, Porter JB, Giannone V, Zhang Y, Griffel L, Brissot P (2011) Improvement in liver pathology of patients with beta-thalassemia treated with deferasirox for at least 3 years. Gastroenterology 141:1202–1211
Forni GL, Podesta M, Musso M, Piaggio G, Musallam KM, Balocco M, Pozzi S, Rosa A, Frassoni F (2013) Differential effects of the type of iron chelator on the absolute number of hematopoietic peripheral progenitors in patients with beta-thalassemia major. Haematologica 98:555–559
Acknowledgments
The authors thank Khaled Musallam, MD PhD, of EVIDA MEDICAL LTD, London, UK, for the medical editorial assistance. Financial support for medical editorial assistance was provided by Novartis Farma SpA.
Author’s contributions
MP was responsible for the study’s concept design, for data analysis and interpretation, and for drafting the manuscript. All of the authors were responsible for the data collection and assembly, for the manuscript’s critical revision for intellectual content, and for approving the manuscript prior to submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Sources of funding
None.
Rights and permissions
About this article
Cite this article
Poggi, M., Sorrentino, F., Pugliese, P. et al. Longitudinal changes of endocrine and bone disease in adults with β-thalassemia major receiving different iron chelators over 5 years. Ann Hematol 95, 757–763 (2016). https://doi.org/10.1007/s00277-016-2633-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-016-2633-y