Abstract
Overexpression, polymorphisms, and mutations of the WT1 gene have been reported in several human tumors including acute myeloid leukemia (AML) and variably correlated with prognosis. Acute promyelocytic leukemia (APL) represents the AML subset disclosing higher WT1 expression levels; however, no WT1 studies specifically focused on APL have been conducted. We screened for the presence of mutations, SNP rs16754, and expression levels of WT1 gene in 103 adult patients with newly diagnosed APL. Fms-like tyrosine kinase (FLT3) mutations were analyzed as well. WT1 mutations were identified in four (4 %) patients. At least one copy of the minor SNP rs16754 allele (WT1 AG or WT1 GG) was detected in 30 (29 %) patients. Six patients (6 %) were homozygous for the minor allele (WT1 GG) and this genotype was associated with higher WT1 mRNA copies (p = 0.018). FLT3 mutations were found in 37 % of patients and correlated with high WT1 mRNA expression (p = 0.004). Patients heterozygous or homozygous for the minor allele and patients homozygous for major (WT1 AA) allele did not differ in terms of presenting features. In adult APL, WT1 gene mutational and polymorphic profile shows similarities with pediatric AML rather than with adult AML.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Wilms tumor 1 (WT1) gene encodes a zinc-finger transcription factor which has emerged as an important regulator of normal and malignant hematopoiesis. WT1 is primarily expressed in the cells of developing genitourinary, central nervous, and hematopoietic systems [1, 2]. WT1 was originally described as a tumor suppressor gene based on its structural and functional loss in patients with WAGR syndrome characterized by Wilms tumor, aniridia, genitourinary malformations, and mental retardation [3, 4]. However, accumulating evidence also points to an oncogenic role for this transcription factor. WT1 is highly expressed in a variety of tumors [5–7] including acute myeloid leukemia (AML) [8, 9]. In addition, its expression is inversely associated with the degree of cell differentiation [10, 11]. Consequently, WT1 is currently considered as a potential target for immunotherapy in both leukemias and solid tumors.
Over the last decade, several studies have documented in AML increased expression levels of WT1 transcript [12–14], mutations in the coding regions of WT1 exons 7 and 9 [15–17], and more recently specific allelic variation (SNP rs16754) [18–20]. Among distinct French-American-British (FAB) AML subsets, AML-M5 is associated with a significantly lower WT1 expression [21] whereas AML-M3 is characterized by the highest WT1 expression levels [13]. Interestingly, a progressive rise in WT1 mRNA expression levels has been described in chronic myelogenous leukemia (CML) [8] and myelodysplastic syndromes (MDS) [22] during disease progression. Yet, conflicting data are currently available on the prognostic impact of these alterations in AML. Two recent studies observed a correlation between high WT1 mRNA expression and improved outcome in acute myeloid leukemia [17, 23].
On the other hand, mutations in the coding region of the WT1 gene are detected in approximately 10 % of adults with cytogenetic normal AML [CN-AML; 10, 15, 24]. While two studies showed an association between WT1 mutation and poor overall survival (OS), disease free survival (DFS) [17, 24] and higher risk of relapse [16, 17], two more recent studies [10, 19] reported lack of WT1 mutational status impact on prognosis. Almost all WT1 mutations in AML cluster in exons 7 and 9. The N-terminal region of exon 7 harbors two mutational hotspot regions located between nucleotide 1285 and 1360 [17] where more than 90 % of the exon 7 mutations are clustered.
The mutational hotspot located in exon 7 also harbors the WT1 SNP rs16754. This is a synonymous SNP consisting of a substitution of the nucleotide adenine with guanine at nucleotide position 1293 and is present in a homozygous (WT1 AA or WT1 GG) or heterozygous state (WT1 AG).
Four main studies investigated the prognostic impact of SNP rs16754 in adult and pediatric AML. Damm et al. [18] identified the combined homozygous and the heterozygous WT1 SNP rs16754 as an independent favorable prognostic marker in adult CN-AML. Subsequently, the Cancer and Leukemia Group B (CALGB) [25] reported that the homozygous form WT1 GG is significantly associated with better DFS and OS. In pediatric AML, Ho et al. [20] observed a better outcome in favorable-risk AML harboring SNP rs16754. On the other hand, Hollink et al. [19] could not identify a prognostic relevance of SNP rs16754 in pediatric AML.
Fms-like tyrosine kinase (FLT3) is a type III receptor tyrosine kinase with important roles in the survival and proliferation of hematopoietic stem cell. Mutations in FLT3 gene occur in 45 % of APL patients [26]. Both internal tandem duplication (ITD) of the juxtamembrane domain and point mutation D835 of the kinase domain (TKD) constitutively activate FLT3. FLT3-ITD mutation is specifically found in AML and is associated with high levels of WT1 transcripts and inferior outcome in both pediatric and adult AML [27, 28].
To date, no studies have investigated in detail WT1 gene variations in APL. Therefore, in addition to WT1 expression level analysis, we carried out a comprehensive study of WT1 mutations and polymorphisms in 103 newly diagnosed APL patients. Finally, we explored the association between mutations, polymorphisms, and WT1 expression level.
Design and methods
Patient samples
Bone marrow samples from newly diagnosed adult APL patients were collected at diagnosis. Of the 103 patients included in the study, 77 patient samples were collected at Policlinico Tor Vergata, Rome and 26 patient samples were collected from La Fé Hospital, Valencia, Spain. Patients were selected as consecutive cases for which both RNA and DNA were available. APL diagnosis was confirmed in all cases at the genetic level by RT-PCR detection of the PML-RARA fusion gene. In all patients included in the study, infiltration of bone marrow by leukemic blasts was >70 %. Written informed consent for the study was obtained from all patients and the study was approved by the IRBs of both participating institutions.
Mutation analysis and SNP rs16754
Genomic DNA was extracted from 103 diagnostic bone marrow samples using Nucleospin blood kit (Macherey-Nagel GmbH & Co., Germany). Polymerase chain amplification of WT1 exons 7 and 9 was performed on genomic DNA by using two primer pairs. The primers used for exon 7 were WT1 ex7 forward: 5′-CTCCAGTGCTCACTCTCCCTC-3′ and WT1 ex7 reverse: 5′- CCTTAGCAGTGTGAGAGCCTG-3′ while exon 9 primers were those reported by Gaidzik et al. [15]. SNP rs16754 and WT1 mutations were confirmed by direct sequencing of the amplified and purified PCR product. Direct sequencing was carried out by using the Big Dye Terminator V3.1 cycle sequencing reaction (Applied Biosystems, Foster City, CA) and the reaction was analyzed on an ABI 3130 Genetic analyzer (Applied Biosystems, USA). Abnormal sequencing results were confirmed by at least two repeated sequencing analysis.
Molecular analysis of FLT3 ITD and TKD
Molecular analysis of FLT3 internal tandem duplication (ITD) in the juxtamembrane and D835 point mutation in the tyrosine kinase domain (TKD) were performed in available samples from 94 patients as described in Noguera et al. [26].
RNA extraction and cDNA synthesis
Total RNA was extracted from leukemic blasts using Trizol (Life technologies, Invitrogen, USA). Reverse transcription was performed on 1 μg total RNA as per standard protocol (Applied Biosystems, Foster City, CA). PML-RARA isoforms were amplified as reported by RT-PCR based method [29].
Expression analysis of WT1 mRNA
Real-time quantitative polymerase chain reaction (RQ-PCR) assay was performed using patient cDNAs (available for 97 cases) on a 7900 real-time PCR system (Applied Biosystems) using the WT1 ProfileQuant Kit as described in the manufacturer’s instructions (Ipsogen, Marseille, France). For analysis of samples and controls, those with detectable WT1 copy numbers were expressed per 104 ABL copies according to EAC criteria [30].
Statistical methods
Chi square test was used to compare the categorical variables between the groups. However, Fisher’s exact test was used wherever chi square test was not appropriate. For WT1 expression analysis, the APL samples were divided into different groups accordingly. To compare continuous variables according to different groups, nonparametric Mann–Whitney U test (comparing two groups) and Kruskal–Wallis test (comparing >2 groups) were used. Results with p values less than 0.05 were considered statistically significant. All statistical analysis was conducted using SPSS 16.
Results
WT1 copy number and patient presenting features
The distribution of WT1 copy number was similar among patients classified as low/intermediate (n = 81) or high risk (n = 17) according to Sanz criteria [31]. The median expression of WT1 copy number in relation to the breakpoint cluster region in the PML gene was also comparable among patients with BCR1 (n = 48), BCR2 (n = 6) and BCR3 (n = 41; data not shown).
Mutational screening of WT1
WT1 mutations were identified in 4 (4 %) out of the 103 newly diagnosed APL patients (Table 1). All four mutations were heterozygous. The three mutations located in exon 7 were frameshift mutations and resulted in a premature stop codon at the protein level. The fourth mutation located in exon 9 was a missense mutation which resulted in replacement of a histidine residue at codon 397 by an arginine.
Analysis of SNP rs16754
The minor allele of the synonymous SNP rs16754 (WT1 AG/GG) was found in 30 (29 %) of the analyzed patients of whom 6 (20 %) were homozygous (WT1 GG). All the four patients who had WT1 mutations were homozygous for major allele (WT1 AA). There was no significant difference in median age, WBC and platelet counts at presentation or PML/RARA fusion isoform between patients with and without SNP rs16754. Finally, analysis of SNP rs16754 according to ethnicity showed that all five analyzable patients of Asian descent included in the study were homozygous or heterozygous for the SNP rs16754 (WT1 AG/GG). Therefore, at variance with the remaining 99 patients of Caucasian origin, there was a prevalence of the G allele in the population of Asian ethnicity (data not shown).
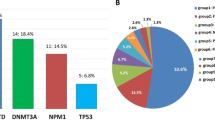
FLT3 mutational status
Out of 94 cases evaluated for FLT3, 35 patients (37 %) had mutations. Of these, 25 patients carried an ITD, 9 cases a TKD, and one patient had concomitant FLT3 ITD and TKD mutations.
Correlation between WT1 mutations, FLT3 mutations, SNP rs16754, and WT1 expression levels
FLT3 ITD and TKD mutations were detected at comparable frequencies in patients with and without WT1 SNP rs16754. WT1 median copy number was significantly higher in patients with (WT1 GG) than in patients heterozygous for the minor allele (WT1 AG) or homozygous for major allele (WT1 AA). However, this difference disappeared combining patients homozygous and heterozygous for minor allele and comparing them with patients homozygous for major allele. We also observed a relatively lower median WT1 copy number in the group of patients with WT1 mutations compared to patients with wild-type WT1 but the difference was not statistically significant (Table 2). Finally, we observed a significantly lower median copy number of WT1 transcript in patients with wild type FLT3 as compared to those harboring FLT3 mutations (p = 0.004, Table 3).
As concerning correlation with outcome, we were unable to carry out the analysis on the whole series due to heterogeneity of treatment context. However, a subanalysis of the relapse cohort revealed that out of seven patients undergoing disease recurrence, five carried WT1 genetic variations (two in the form of mutations and three heterozygous for the rs16754 SNP) while four had FLT3 mutations (three FLT3-ITD and one FLT3-TKD).
Discussion
To the best of our knowledge, the present study is the first comprehensive analysis of WT1 gene variations in a large series of newly diagnosed APL patients. Three of the four WT1 mutations were frameshift mutations located in the exon 7 “hotspot” region already described in AML [17] which result in a premature stop codon. As previously reported, mutations affecting WT1 gene coding region may result in a protein incapable of proper binding to DNA in turn leading to transcriptional abnormalities [15]. All patients with mutations were homozygous for the major allele of SNP rs16754 consistent with data reported by Ho et al in pediatric AML [20].
At variance with previous reports on AML [32], of the four patients with WT1 mutations in our study, two harbored mutation in FLT3-TKD region and none had FLT3-ITD mutation. Two of the four patients with WT1 mutations relapsed shortly after remission including one of those who had FLT3-TKD mutation. This patient was considered as high risk according to Sanz risk score. For AML patients, it has been also reported that WT1 expression is significantly higher in cases harboring mutations in this gene [20, 33, 34]. However in our cohort, patients harboring WT1 mutations had a relatively lower WT1 copy numbers (median, 12750 copies). We recognize however the limitation of these comparisons, which are based on only four cases mutated for WT1.
As to the WT1 SNP rs16754, the frequency of homozygosity for the minor allele in our APL series appears higher than that reported in two studies conducted in adult AML (5.8 % vs. 1.6 % and 2.1 %; Damm et al. [18] and Hollink et al. [19]) but in line with results in pediatric AML [20]. Recently, synonymous SNP rs16754 has been correlated with higher expression levels of WT1 in pediatric AML patients [20]. In keeping with these observations, we found a higher number of WT1 transcripts in patients with the homozygous minor allele (WT1 GG) compared to other allelic variants.
In our cohort, both patients with FLT3-ITD or FLT3-TKD mutations had a high median WT1 copy number. Two recent studies on AML patients have shown that high WT1 expression was specifically correlated with presence of FLT3-ITD mutation [27, 35]. However, in our series, we observed a significant correlation between WT1 expression and FLT3-TKD mutation.
We could not find any significant association between WT1 status and patient presenting features. As concerning clinical outcome, the analysis was hampered by several factors including the very small number of relapses and treatment heterogeneity. In particular, distinct therapeutic options were given for post-induction in the three different regimens adopted by the Gruppo Italiano Malattie Ematologiche dell’Adulto and Programa para el Estudio y la Terapéutica en Hemopatía Maligna groups in the considered period. However, the available data hereby presented on relapsed patients may suggest that WT1 genetic variations could have an impact on prognosis. Larger studies in homogeneously treated patients are needed to better clarify the prognostic role of WT1 gene status in APL.
References
Scharnhorst V, van der Eb AJ, Jochemsen AG (2001) WT1 proteins: functions in growth and differentiation. Gene 273:141–161
Yang L, Han Y, Suarez Saiz F, Minden MD (2007) A tumor suppressor and oncogene: the WT1 story. Leukemia 21:868–876
Riccardi VM, Sujansky E, Smith AC, Francke U (1978) Chromosomal imbalance in the Aniridia-Wilms’ tumor association: 11p interstitial deletion. Pediatrics 61:604–610
Haber DA, Buckler AJ, Glaser T, Call KM, Pelletier J, Sohn RL, Douglass EC, Housman DE (1990) An internal deletion within an 11p13 zinc finger gene contributes to the development of Wilms’ tumor. Cell 61:1257–1269
Oji Y, Miyoshi S, Maeda H, Hayashi S, Tamaki H, Nakatsuka S, Yao M, Takahashi E, Nakano Y, Hirabayashi H, Shintani Y, Oka Y, Tsuboi A, Hosen N, Asada M, Fujioka T, Murakami M, Kanato K, Motomura M, Kim EH, Kawakami M, Ikegame K, Ogawa H, Aozasa K, Kawase I, Sugiyama H (2002) Overexpression of the Wilms’ tumor gene WT1 in de novo lung cancers. Int J Cancer 100:297–303
Koesters R, Linnebacher M, Coy JF, Germann A, Schwitalle Y, Findeisen P, von Knebel DM (2004) WT1 is a tumor-associated antigen in colon cancer that can be recognized by in vitro stimulated cytotoxic T cells. Int J Cancer 109:385–392
Thorner P, Squire J, Plavsic N, Jong R, Greenberg M, Zielenska M (1999) Expression of WT1 in pediatric small cell tumors: report of two cases with a possible mesothelial origin. Pediatr Dev Pathol 2:33–41
Inoue K, Sugiyama H, Ogawa H, Nakagawa M, Yamagami T, Miwa H, Kita K, Hiraoka A, Masaoka T, Nasu K, Kyo T, Dohy H, Nakauchi H, Ishidate T, Akiyama T, Kishimoto T (1994) WT1 as a new prognostic factor and a new marker for the detection of minimal residual disease in acute leukemia. Blood 84:3071–3079
Inoue K, Ogawa H, Sonoda Y, Kimura T, Sakabe H, Oka Y, Miyake S, Tamaki H, Oji Y, Yamagami T, Tatekawa T, Soma T, Kishimoto T, Sugiyama H (1997) Aberrant overexpression of the Wilms tumor gene (WT1) in human leukemia. Blood 89:1405–1412
Virappane P, Gale R, Hills R, Kakkas I, Summers K, Stevens J, Allen C, Green C, Quentmeier H, Drexler H, Burnett A, Linch D, Bonnet D, Lister TA, Fitzgibbon J (2008) Mutation of the Wilms’ tumor 1 gene is a poor prognostic factor associated with chemotherapy resistance in normal karyotype acute myeloid leukemia: the United Kingdom Medical Research Council Adult Leukaemia Working Party. J Clin Oncol 26:5429–5435
Noronha SA, Farrar JE, Alonzo TA, Gerbing RB, Lacayo NJ, Dahl GV, Ravindranath Y, Arceci RJ, Loeb DM (2009) WT1 expression at diagnosis does not predict survival in pediatric AML: a report from the Children’s Oncology Group. Pediatr Blood Cancer 53:1136–1139
Miwa H, Beran M, Saunders GF (1992) Expression of the Wilms’ tumor gene (WT1) in human leukemias. Leukemia 6:405–409
Cilloni D, Gottardi E, De Micheli D, Serra A, Volpe G, Messa F, Rege-Cambrin G, Guerrasio A, Divona M, Lo Coco F, Saglio G (2002) Quantitative assessment of WT1 expression by real time quantitative PCR may be a useful tool for monitoring minimal residual disease in acute leukemia patients. Leukemia 16:2115–2121
Cilloni D, Renneville A, Hermitte F, Hills RK, Daly S, Jovanovic JV, Gottardi E, Fava M, Schnittger S, Weiss T, Izzo B, Nomdedeu J, van der Heijden A, van der Reijden BA, Jansen JH, van der Velden VH, Ommen H, Preudhomme C, Saglio G, Grimwade D (2009) Real-time quantitative polymerase chain reaction detection of minimal residual disease by standardized WT1 assay to enhance risk stratification in acute myeloid leukemia: a European LeukemiaNet study. J Clin Oncol 27:5195–5201
Gaidzik VI, Schlenk RF, Moschny S, Becker A, Bullinger L, Corbacioglu A, Krauter J, Schlegelberger B, Ganser A, Döhner H, Döhner K, German-Austrian AML Study Group (2009) Prognostic impact of WT1 mutations in cytogenetically normal acute myeloid leukemia: a study of the German-Austrian AML Study Group. Blood 113:4505–4511
Hou HA, Huang TC, Lin LI, Liu CY, Chen CY, Chou WC, Tang JL, Tseng MH, Huang CF, Chiang YC, Lee FY, Liu MC, Yao M, Huang SY, Ko BS, Hsu SC, Wu SJ, Tsay W, Chen YC, Tien HF (2010) WT1 mutation in 470 adult patients with acute myeloid leukemia: stability during disease evolution and implication of its incorporation into a survival scoring system. Blood 115:5222–5231
Ho PA, Zeng R, Alonzo TA, Gerbing RB, Miller KL, Pollard JA, Stirewalt DL, Heerema NA, Raimondi SC, Hirsch B, Franklin JL, Lange B, Meshinchi S (2010) Prevalence and prognostic implications of WT1 mutations in pediatric acute myeloid leukemia (AML): a report from the Children’s Oncology Group. Blood 116:702–710
Damm F, Heuser M, Morgan M, Yun H, Grosshennig A, Göhring G, Schlegelberger B, Döhner K, Ottmann O, Lübbert M, Heit W, Kanz L, Schlimok G, Raghavachar A, Fiedler W, Kirchner H, Döhner H, Heil G, Ganser A, Krauter J (2010) Single nucleotide polymorphism in the mutational hotspot of WT1 predicts a favorable outcome in patients with cytogenetically normal acute myeloid leukemia. J Clin Oncol 28:578–585
Hollink IH, van den Heuvel-Eibrink MM, Zimmermann M, Balgobind BV, Arentsen-Peters ST, Alders M, Willasch A, Kaspers GJ, Trka J, Baruchel A, Creutzig U, Pieters R, Reinhardt D, Zwaan CM (2010) No prognostic impact of the WT1 gene single nucleotide polymorphism rs16754 in pediatric acute myeloid leukemia. J Clin Oncol 28:e523–e526
Ho PA, Kuhn J, Gerbing RB, Pollard JA, Zeng R, Miller KL, Heerema NA, Raimondi SC, Hirsch BA, Franklin JL, Lange B, Gamis AS, Alonzo T, Meshinchi S (2011) WT1 synonymous single nucleotide polymorphism rs16754 correlates with higher mRNA expression and predicts significantly improved outcome in favorable-risk pediatric acute myeloid leukemia: a report from the children’s oncology group. J Clin Oncol 29:704–711
Siehl JM, Reinwald M, Heufelder K, Menssen HD, Keilholz U, Thiel E (2004) Expression of Wilms’ tumor gene 1 at different stages of acute myeloid leukemia and analysis of its major splice variants. Ann Hematol 83:745–750
Tamaki H, Ogawa H, Ohyashiki K, Ohyashiki JH, Iwama H, Inoue K, Soma T, Oka Y, Tatekawa T, Oji Y, Tsuboi A, Kim EH, Kawakami M, Fuchigami K, Tomonaga M, Toyama K, Aozasa K, Kishimoto T, Sugiyama H (1999) The Wilms’ tumor gene WT1 is a good marker for diagnosis of disease progression of myelodysplastic syndromes. Leukemia 13:393–399
Miglino M, Colombo N, Pica G, Grasso R, Clavio M, Bergamaschi M, Ballerini F, Ghiso A, Ghiggi C, Mitscheunig L, Beltrami G, Cagnetta A, Vignolo L, Lucchetti MV, Aquino S, Pierri I, Sessarego M, Carella AM, Gobbi M (2011) WT1 overexpression at diagnosis may predict favorable outcome in patients with de novo non-M3 acute myeloid leukemia. Leuk Lymphoma 52:1961–1969
Paschka P, Marcucci G, Ruppert AS, Whitman SP, Mrózek K, Maharry K, Langer C, Baldus CD, Zhao W, Powell BL, Baer MR, Carroll AJ, Caligiuri MA, Kolitz JE, Larson RA, Bloomfield CD (2008) Wilms’ tumor 1 gene mutations independently predict poor outcome in adults with cytogenetically normal acute myeloid leukemia: a cancer and leukemia group B study. J Clin Oncol 26:4595–4602
Becker H, Maharry K, Radmacher MD, Mrózek K, Metzeler KH, Whitman SP, Schwind S, Kohlschmidt J, Wu YZ, Powell BL, Carter TH, Kolitz JE, Wetzler M, Carroll AJ, Baer MR, Moore JO, Caligiuri MA, Larson RA, Marcucci G, Bloomfield CD (2011) Clinical outcome and gene- and microRNA-expression profiling according to the Wilms tumor 1 (WT1) single nucleotide polymorphism rs16754 in adult de novo cytogenetically normal acute myeloid leukemia: a Cancer and Leukemia Group B study. Haematologica 96:1488–1495
Noguera NI, Breccia M, Divona M, Diverio D, Costa V, De Santis S, Avvisati G, Pinazzi MB, Petti MC, Mandelli F, Lo Coco F (2002) Alterations of the FLT3 gene in acute promyelocytic leukemia: association with diagnostic characteristics and analysis of clinical outcome in patients treated with the Italian AIDA protocol. Leukemia 16:2185–2189
Staffas A, Kanduri M, Hovland R, Rosenquist R, Ommen HB, Abrahamsson J, Forestier E, Jahnukainen K, Jónsson ÓG, Zeller B, Palle J, Lönnerholm G, Hasle H, Palmqvist L, Ehrencrona H, Nordic Society of Pediatric Hematology and Oncology (NOPHO) (2011) Presence of FLT3-ITD and high BAALC expression are independent prognostic markers in childhood acute myeloid leukemia. Blood 118:5905–5913
Brunet S, Labopin M, Esteve J, Cornelissen J, Socié G, Iori AP, Verdonck LF, Volin L, Gratwohl A, Sierra J, Mohty M, Rocha V (2012) Impact of FLT3 internal tandem duplication on the outcome of related and unrelated hematopoietic transplantation for adult acute myeloid leukemia in first remission: a retrospective analysis. J Clin Oncol 30:735–741
van Dongen JJ, Macintyre EA, Gabert JA, Delabesse E, Rossi V, Saglio G, Gottardi E, Rambaldi A, Dotti G, Griesinger F, Parreira A, Gameiro P, Diáz MG, Malec M, Langerak AW, San Miguel JF, Biondi A (1999) Standardized RT-PCR analysis of fusion gene transcripts from chromosome aberrations in acute leukemia for detection of minimal residual disease. Report of the BIOMED-1 Concerted Action: investigation of minimal residual disease in acute leukemia. Leukemia 13:1901–1928
Gabert J, Beillard E, van der Velden VH, Bi W, Grimwade D, Pallisgaard N, Barbany G, Cazzaniga G, Cayuela JM, Cavé H, Pane F, Aerts JL, De Micheli D, Thirion X, Pradel V, González M, Viehmann S, Malec M, Saglio G, van Dongen JJ (2003) Standardization and quality control studies of ‘real-time’ quantitative reverse transcriptase polymerase chain reaction of fusion gene transcripts for residual disease detection in leukemia—a Europe Against Cancer program. Leukemia 17:2318–2357
Sanz MA, Lo Coco F, Martín G, Avvisati G, Rayón C, Barbui T, Díaz-Mediavilla J, Fioritoni G, González JD, Liso V, Esteve J, Ferrara F, Bolufer P, Bernasconi C, Gonzalez M, Rodeghiero F, Colomer D, Petti MC, Ribera JM, Mandelli F (2000) Definition of relapse risk and role of nonanthracycline drugs for consolidation in patients with acute promyelocytic leukemia: a joint study of the PETHEMA and GIMEMA cooperative groups. Blood 96:1247–1253
Summers K, Stevens J, Kakkas I, Smith M, Smith LL, Macdougall F, Cavenagh J, Bonnet D, Young BD, Lister TA, Fitzgibbon J (2007) Wilms’ tumour 1 mutations are associated with FLT3-ITD and failure of standard induction chemotherapy in patients with normal karyotype AML. Leukemia 21:550–551
Willasch AM, Gruhn B, Coliva T, Kalinova M, Schneider G, Kreyenberg H, Steinbach D, Weber G, Hollink IH, Zwaan CM, Biondi A, van der Velden VH, Reinhardt D, Cazzaniga G, Bader P, Trka J, European Study Group on WT1 Expression in Childhood AML (2009) Standardization of WT1 mRNA quantitation for minimal residual disease monitoring in childhood AML and implications of WT1 gene mutations: a European multicenter study. Leukemia 23:1472–1479
Heesch S, Goekbuget N, Stroux A, Tanchez JO, Schlee C, Burmeister T, Schwartz S, Blau O, Keilholz U, Busse A, Hoelzer D, Thiel E, Hofmann WK, Baldus CD (2010) Prognostic implications of mutations and expression of the Wilms tumor 1 (WT1) gene in adult acute T-lymphoblastic leukemia. Haematologica 95:942–949
Spassov BV, Stoimenov AS, Balatzenko GN, Genova ML, Peichev DB, Konstantinov SM (2011) Wilms’ tumor protein and FLT3-internal tandem duplication expression in patients with de novo acute myeloid leukemia. Hematology 16:37–42
Acknowledgments
Prof. F. Lo-Coco acknowledges the study support from the Associazione Italiana contro le Leucemie (AIL) and Associazione Italiana per la Ricerca sul Cancro (AIRC).
Disclosures
The authors declare that there are no competing financial interests in relation to the work described in this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gaur, G.C., Ramadan, S.M., Cicconi, L. et al. Analysis of mutational status, SNP rs16754, and expression levels of Wilms tumor 1 (WT1) gene in acute promyelocytic leukemia. Ann Hematol 91, 1855–1860 (2012). https://doi.org/10.1007/s00277-012-1546-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-012-1546-7