Abstract
Acute kidney injury (AKI) is frequent in multiple myeloma (MM) patients and strongly affects prognosis, with particularly poor outcomes in patients requiring hemodialysis. Introduction of the novel therapeutic agents to MM therapy has improved myeloma response and renal outcome. This case series reviews the efficacy of combined systemic and extracorporeal therapy to further optimize time to light chain (serum-free light chain (sFLC)) reduction and renal recovery in MM patients with dialysis-dependent AKI (n = 19). High cut-off (HCO) hemodialysis for extracorporeal sFLC removal was initiated in parallel to chemotherapy. Combined therapy resulted in early sFLC response after a median of 13 (range 4–48) days and 6 (3–22) HCO hemodialysis sessions. Time to sFLC response was shorter in patients recovering renal function. Median time to dialysis independence was 15 (4–64) days. By intent-to-treat analysis, sustained renal recovery was achieved in 73.7% (77.8% adjusted for death) of patients. In multivariate analysis, duration of AKI prior to initiation of therapy was an independent predictor of renal functional outcome. Combining HCO hemodialysis for extracorporeal sFLC elimination and effective chemotherapy is a novel treatment strategy allowing for early and sustained sFLC reduction and a high proportion of renal recovery in these patients. Timely diagnosis and onset of therapy is essential for improving renal outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) and renal failure are among the most frequent and serious complications of multiple myeloma with sustained impact on treatment and patient prognosis. Depending on definition criteria, up to 50% of patients demonstrate AKI at primary diagnosis and up to another 25% of patients at later time points of myeloma disease [1–5]. As much as 10% of patients are in need of renal replacement therapy at primary diagnosis [6]. In primary diagnosis and relapse, elevated serum creatinine resulting from myeloma-associated renal injury is an independent criterion for treatment initiation.
Various factors promote AKI in multiple myeloma patients. In severe AKI, the principal underlying cause is light chain-induced cast nephropathy, often with a preceding trigger. Cast nephropathy accounts for around 70% of dialysis-dependent AKI in multiple myeloma [7]. In the kidney, monoclonal light chains are subject to free glomerular filtration with subsequent proximal tubular reabsorption and degradation. With excessive free light chain production in multiple myeloma, proximal tubular load overwhelms reabsorption capacity with filtered light chains delivered to distal nephron segments where they coaggregate with Tamm–Horsfall protein to form light chain casts. The so formed casts result in tubular luminal obstruction and occlusion of the nephron [8–11]. A number of systemic and local factors promoting aggregate formation have been identified, among them dehydration, hypercalcemia, and acidosis [12, 13]. At proximal tubular sites, high light chain load exerts direct morphologic changes and promotes the release of proinflammatory cytokines. The inflammatory response of the tubulointerstitium rapidly progresses to fibrosis and irreversible renal scarring [14]. Limiting exposure of the kidney to nephrotoxic light chains is one of the most critical determinants for recovery of renal function in cast nephropathy.
Impaired renal function has been recognized as a negative prognostic factor associated with decreased response, shorter survival, and higher early mortality in patients treated with conventional chemotherapy [3, 5]. Prior to introduction of the novel therapeutic agents, prognosis of dialysis-dependent myeloma patients was poor with a median survival of 3–11 months [5, 15]. However, if renal function recovered, survival was comparable to patients without AKI [5]. Introduction of the novel therapeutic agents has substantially shortened time to myeloma response and improved patient outcome. Both, bortezomib- and lenalidomide-based regimens, with a median reported time to response of 42 days and one month, respectively, are highly effective in treating myeloma in patients with impaired renal function [16, 17]. Bortezomib is considered treatment of choice for myeloma patients with impaired renal function, including dialysis-dependent chronic kidney disease, as published in the recent consensus statement of the International Myeloma Working Group (IMWG) [18]. These chemotherapy regimens provide the basis for novel treatment strategies, using concomitant extracorporeal light chain elimination for further reduction of renal exposure to nephrotoxic light chains.
Until present, extracorporeal light chain elimination using plasmapheresis has shown little impact on renal recovery and overall survival [19, 20]. We and others have established extended hemodialysis using a high cut-off (HCO) protein permeable membrane an efficient means for extracorporeal removal of serum-free light chains (sFLC), allowing for rapid and effective reduction in sFLC concentrations [21, 22]. Here, we report outcome data from a series of patients with multiple myeloma and dialysis-dependent AKI, treated with chemotherapy and concomitant HCO hemodialysis for extracorporeal light chain elimination. Using this strategy, we document early sFLC response and sustained renal recovery in a high proportion of patients in both, first-line and relapse treatment.
Subjects and methods
We reviewed our experience in a series of 19 consecutive patients with multiple myeloma and dialysis-dependent AKI, presenting at our center between Nov. 2006 and Oct. 2009. Patients had primary diagnosed, relapsed, or refractory myeloma disease. The Durie and Salmon and ISS staging system was used. All patients had dialysis-dependent AKI stage failure/loss according to RIFLE or stage III according to the AKIN criteria, respectively [23, 24]. Adequate cardiac, hepatic, and pulmonary function allowed administration of systemic chemotherapy.
Chemotherapy and concomitant extracorporeal sFLC elimination were initiated within the first 48 h upon admission in all patients. All patients gave written informed consent prior to initiation of any treatment. Chemotherapy regimens were determined by the institutional hematologist, mainly comprising novel therapeutic agents with bortezomib as the principal agent used. All patients received intensive supportive care including i.v. hydration, urine alkalinization and discontinuation of nephrotoxic substances. Renal biopsy was performed if causes of AKI other than cast nephropathy could not be excluded from clinical, laboratory, and ultrasound findings.
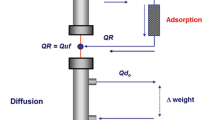
For extracorporeal sFLC elimination, extended 6-h hemodialysis was performed using a HCO, protein-permeable filter (HCO1100, Gambro Dialysatoren GmbH, Hechingen, Germany). The HCO1100 filter is CE-certified for the elimination of plasma proteins up to 45 kD and used strictly within certification in all patients. The filter allows elimination of both κ and λ light chains at respective clearances, in addition to fluid and solute control as otherwise obtained by standard hemodialysis. Blood and dialysate flow were set to 250 and 500 ml/min, respectively, with ultrafiltration according to clinical needs. Albumin loss across the filter was substituted. Treatment schedule was five sessions within the first 7 days, followed by every other day to allow for redistribution of sFLC from extracellular fluid volume. sFLC analysis was performed prior to and after each HCO hemodialysis and during follow-up using an immunoassay (Freelite, The Binding Site, Birmingham, UK). HCO hemodialysis was stopped upon sFLC concentrations <500 mg/l on the day of the next scheduled session, irrespective of renal function. If required, hemodialysis was continued using standard high-flux hemodialysis filters.
Time to sFLC response was calculated as timespan between first and last HCO hemodialysis session. Duration of AKI prior to treatment initiation was defined as the timespan from first in- or outpatient standard hemodialysis to first HCO hemodialysis. Independency of hemodialysis was determined by the institutional nephrologist with an eGFR ≥15 ml/min/1.73 m2, as calculated by the abbreviated MDRD equation [25], at least 14 days after the last extracorporeal treatment (HCO or standard hemodialysis). Long-term renal outcome was assessed according to consensus criteria and Kidney Disease Outcomes Quality Initiative (K/DOQI) classification of chronic kidney disease [26, 27]. Patients free of hemodialysis and again in need of renal replacement therapy during follow-up were not reentered into the analysis. Assessment of myeloma response was performed by M-protein measurement in serum and protein measurement in urine and by serum-free light chain analysis. Myeloma response was defined using the IMWG criteria [28].
All data were calculated by intent-to-treat (ITT) analysis. Nonparametric results are expressed as median and range. Comparisons between outcome groups were analyzed by Mann–Whitney U test. The cox proportional hazards model was used for multivariate analyses of events. Rates of renal recovery were assessed using Kaplan Meier estimates. Significance end point was set to p = 0.05. The statistical package SPSS (version 16.0, SPSS Inc., Chicago, IL, USA) was used for all analyses.
Results
Patient demographics, baseline disease characteristics, and myeloma therapy are given in Table 1. The intent-to-treat cohort consisted of 19 patients. Two deaths occurred, such that complete follow-up was obtained from 17 patients. Median age was 69 (range 50–83) years. Ten patients had newly diagnosed, nine relapsed or refractory myeloma. All patients had ISS stage III disease. Median sFLC concentration at baseline was 8580 (1590–66100) mg/l. All patients showed AKI requiring renal replacement therapy. Median serum creatinine was 6.8 (4.4–11.6) mg/dl, median eGFR 7.0 (3.3–10.9) ml/min/1.73 m2. Five patients were oligo-anuric, 14 patients had preserved diuresis, all with documented Bence–Jones proteinuria above 2 g/day (data not shown). Nine patients had been on conventional hemodialysis between 5 and 37 days prior to admission to our center. Renal biopsy was obtained in six patients, all demonstrating cast nephropathy.
Chemotherapy and concomitant extracorporeal light chain elimination were initiated in parallel within the first 48 h upon admission. Most patients (14/19) received bortezomib-based chemotherapy. Two patients on bortezomib-based regimen were considered refractory with no decrease in sFLC seen at weeks 3 and 6, respectively. These patients were subsequently switched to a lenalidomide-based regimen and showed response. Two patients received high-dose melphalan during course of the disease (Table 1). Two early deaths occurred due to sepsis (day 31) and progressive disease (day 83). All other patients completed chemotherapy and projected number of HCO hemodialyses until sFLC reduction below the threshold defined.
By ITT analysis, sustained renal recovery was achieved in 73.7% (77.8 %, adjusted for death) or 14 out of 19 patients with a median time to independence of hemodialysis of 15 (4–64) days (Table 2). Renal recovery rate over time is depicted in Fig. 1.
Median time to sFLC response was 13 (4–48) days, with a median of 6 (3–22) HCO hemodialysis sessions required to attain sustained sFLC concentrations below 500 mg/l. Time to sFLC response was markedly shorter in patients recovering renal function, as compared to patients remaining dialysis dependent (12 (4–39) vs. 23 (12–48) days), respectively, albeit not attaining significance level in our cohort (p = 0.087) (Fig. 2a). In multivariate analysis, the duration of AKI prior to initiation of therapy was an independent predictor of renal functional outcome. The median duration of AKI was significantly shorter in patients recovering renal function, as compared with patients remaining on hemodialysis (2 (1–18) vs. 33 (9–37) days), respectively, p < 0.001) (Fig. 2b).
Myeloma response and renal outcome of patients completing follow-up is listed in Table 3. Of the 17 patients evaluated, 6 patients achieved partial response resulting in an overall response rate (ORR) of 35%. Six patients had stable disease lasting more than 100 days after initiation of therapy. Four patients are continuously in remission, including one patient who underwent high-dose melphalan treatment. Maximum sFLC reduction was 94.7% (79.6–99.8%) of baseline sFLC concentrations with the sFLC nadir observed at 25 (6–378) days.
According to the consensus criteria, 1/17 patients (6%) attained renal complete response (sustained improvement of baseline creatinine clearance (CrCl) <50 to 60 ml/min or above), 5/17 patients (29%) attained renal partial response (improvement of baseline CrCl <15 to 30–59 ml/min), 3 of which showed creatinine clearances between 50 and 59 ml/min, and 8/17 patients (47%) attained renal minor response (improvement of baseline CrCl <15 to 15–29 ml/min). Classification of renal functional outcome according to K/DOQI resulted in 1/17 patients (6%) in chronic kidney disease (CKD) stage II, 4/17 patients (24%) in CKD stage III, and 9/17 patients (53%) in CKD stage IV. Three out of 17 patients (18%) remained dialysis-dependent in CKD stage V (Table 3). Patients not recovering renal function suffered from refractory myeloma disease, delayed sFLC response, and prolonged dialysis-dependent AKI prior to treatment initiation.
Discussion
Dialysis-dependent acute kidney injury secondary to cast nephropathy is one of the most challenging conditions in multiple myeloma disease with mostly unfavorable outcome prior to introduction of the novel therapeutic agents. Restoring kidney function simplifies myeloma treatment and improves patient survival. In cast nephropathy, limiting light chain exposure of the kidney is the principal therapeutic goal. In view of this, plasmapheresis has been used for extracorporeal light chain elimination in the past, albeit without benefit in randomized trials [19, 20]. In the present investigations, we used HCO hemodialysis as a novel technique for extracorporeal elimination of sFLC.
Introduction of the novel therapeutic agents to myeloma therapy has changed chemotherapy and prognosis in patients with impaired renal function. Bortezomib in combination with high-dose dexamethasone is considered a treatment of choice for patients with renal impairment [18]. In the kidney, due to its inhibitory effect on NFκ-B, bortezomib may have a positive effect on tubulointerstitial inflammation and fibrogenesis [29]. Recovery of AKI and impaired renal function has been reported under bortezomib-based chemotherapy [30, 31]. A recent phase II trial introduced bortezomib–doxorubicin–dexamethasone (PAD) as a combination inducing high rates of myeloma and renal response [32]. With respect to chemotherapy, a high myeloma response rate and the early onset of response are key components for renal recovery. These characteristics are also shared by lenalidomide, a therapeutic alternative also evaluated in patients with impaired renal function and end-stage renal disease [33, 34].
Only a very limited number of trials are published regarding chemotherapy and outcome in the subgroup of myeloma patients with dialysis-dependent AKI. Historical data, using conventional chemotherapy, demonstrate recovery in not more than 26% of patients [2, 5]. Two recent trials have highlighted the potential of the novel therapeutic agents in these patients. Matsue et al. [35], in 12 newly diagnosed patients with dialysis-dependent AKI, showed renal recovery in 67% of patients. The patients mainly received dexamethasone, some thalidomide-based regimen. All patients with myeloma response better than PR recovered renal function. Kastritis et al. [36], among 41 primary diagnoses with impaired renal function receiving thalidomide- or bortezomib-based regimen, reported renal recovery in 80% of a subgroup of patients requiring hemodialysis. However, this subgroup was small, with only ten patients in need of renal replacement therapy.
In light of this, we hypothesized that early onset and effective extracorporeal sFLC elimination may further reduce light chain exposure of the kidney and facilitate renal recovery. In the patients reported, we used HCO hemodialysis in parallel to chemotherapy to reduce sFLC concentrations. Based on kinetic modeling and intraindividual comparison, extended HCO hemodialysis is by far a more efficient technique of extracorporeal sFLC elimination, as compared to plasmapheresis [22, 37]. Using this strategy, combined systemic and extracorporeal therapy allowed for renal recovery in 73.7% of patients by ITT analysis in a cohort with mostly unfavorable prognostic parameters. Almost half of patients had relapsed or refractory myeloma disease. It is appreciated that patients with light chain myeloma only, severe AKI, or Bence–Jones proteinuria ≥2 g/d have a lower probability of renal recovery [31]. Almost all patients fulfilled these criteria. In parallel to chemotherapy, a median of six HCO hemodialysis sessions allowed sustained reduction of sFLC concentrations below 500 mg/l within a median of less than 2 weeks time. In patients recovering renal function, time to sFLC response was markedly shorter than in patients remaining dialysis-dependent, underlining the importance of early light chain reduction. In multivariate analysis, the duration of AKI prior to treatment initiation was an independent predictor of renal recovery. Timely diagnosis and onset of therapy is hence essential for patients to derive maximum benefit from current treatment strategies.
In our cohort, excellent renal response was achieved, despite a relatively low ORR of 35% with 6 out of 17 patients formally achieving partial remission. The apparent discrepancy is explained by the difficulty of response evaluation in myeloma patients with severe renal impairment. Standard IMWG criteria are difficult to apply to this group of patients. Four out of six of our patients with SD had light chain myeloma and did not attain >90% reduction of urinary M-protein to be classified as PR, nonetheless had >85% reduction in sFLC, indicating that these patients responded to treatment. All of them became independent of hemodialysis. Two patients with PD showed a temporary response with a reduction of sFLC >80% at the time of dialysis independence but were progressive at subsequent myeloma staging. We conclude that measuring sFLC concentrations, as compared to urinary M-protein, is the superior parameter to guide extracorporeal therapy and even more for assessment of myeloma response in these patients. In patients with light chain myeloma showing oligo-anuria, determination of Bence–Jones proteinuria is difficult. Upon recovery of renal function, filtration of sFLC increases and excretion of Bence–Jones protein is not consequently less. Furthermore, onset of response cannot be assessed in a timely manner using IMWG criteria but is essential to know in patients where recovery of renal function is essentially dependent on the duration of kidney light chain exposure. It is self-evident, that response evaluation based on sFLC measurement is done with adequate distance to any extracorporeal treatment. Given the fact that serum half-life of sFLC is 3–5 days only, even in patients without residual renal function, this is possible without difficulties.
The question remains, whether in the era of novel therapeutic agents with a short time to myeloma response, as reported with 1 month and 42 days for lenalidomide and bortezomib, respectively, extracorporeal light chain elimination will further improve renal outcome in dialysis-dependent patients with cast nephropathy. Our data show that the time to sustained light chain reduction can be optimized. We calculate a minimum win of 2 weeks time with respect to light chain exposure of the kidney. Given the very limited time frame, within which therapeutic intervention may improve renal outcome, this is a relevant timespan, likely to affect renal and patient prognosis. This is underlined by our finding that renal recovery was achieved after a median of less than 2 weeks time. Consequently, this question is currently addressed in a prospective European multicenter RCT (EuLITE) [38].
References
Alexanian R, Barlogie B, Dixon D (1990) Renal failure in multiple myeloma. Pathogenesis and prognostic implications. Arch Intern Med 150:1693–1695
Bladé J, Fernandez-Llama P, Bosch F, Montoliù J, Lens XM, Montoto S et al (1998) Renal failure in multiple myeloma: presenting features and predictors of outcome in 94 patients from a single institution. Arch Intern Med 158:1889–1893
Kyle RA, Gertz MA, Witzig TE, Lust JA, Lacy MQ, Dispenzieri A et al (2003) Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc 78:21–33
Eleutherakis-Papaiakovou V, Bamias A, Gika D, Simeonidis A, Pouli A, Anagnostopoulos A et al (2007) Renal failure in multiple myeloma: incidence, correlations, and prognostic significance. Leuk Lymphoma 48:337–341
Knudsen LM, Hjorth M, Hippe E (2000) Renal failure in multiple myeloma: reversibility and impact on the prognosis. Nordic Myeloma Study Group. Eur J Haematol 65:175–181
Torra R, Blade J, Cases A, López-Pedret J, Montserrat E, Rozman C et al (1995) Patients with multiple myeloma requiring long-term dialysis: presenting features, response to therapy, and outcome in a series of 20 cases. Br J Haematol 91:854–859
Hutchison CA, Bradwell AR, Cook M, Basnayake K, Basu S, Harding S et al (2009) Treatment of acute renal failure secondary to multiple myeloma with chemotherapy and extended high cut-off hemodialysis. Clin J Am Soc Nephrol 4:745–754
Santostefano M, Zanchelli F, Zaccaria A, Poletti G, Fusaroli M (2005) The ultrastructural basis of renal pathology in monoclonal gammopathies. J Nephrol 18:659–675
Huang ZQ, Sanders PW (1995) Biochemical interaction between Tamm-Horsfall glycoprotein and Ig light chains in the pathogenesis of cast nephropathy. Lab Invest 73:810–817
Ying WZ, Sanders PW (2001) Mapping the binding domain of immunoglobulin light chains for Tamm-Horsfall protein. Am J Pathol 158:1859–1866
Sanders PW, Booker BB, Bishop JB, Cheung HC (1990) Mechanisms of intranephronal proteinaceous cast formation by low molecular weight proteins. J Clin Invest 85:570–576
Sanders PW, Booker BB (1991) Pathobiology of cast nephropathy from human Bence Jones proteins. N Engl J Med 324:1845–1851
Blade J, Rosinol L (2005) Renal, hematologic and infectious complications in multiple myeloma. Best Pract Res Clin Haematol 18:635–652
Basnayake K, Cheung CK, Sheaff M, Fuggle W, Kamel D, Nakoinz S et al (2010) Differential progression of renal scarring and determinants of late recovery in sustained dialysis dependent acute kidney injury secondary to myeloma kidney. J Clin Pathol 63:884–887
Tsakiris DJ, Stel VS, Finne P, Fraser E, Heaf J, de Meester J et al (2010) Incidence and outcome of patients starting renal replacement therapy for end-stage renal disease due to multiple myeloma or light-chain deposit disease: an ERA-EDTA Registry Study. Nephrol Dial Transplant 25:1200–1206
Richardson PG, Barlogie B, Berenson J, Shingal S, Jagannath S, Irwin DH, SUMMIT Investigators et al (2005) Clinical factors predictive of outcome with bortezomib in patients with relapsed, refractory multiple myeloma. Blood 106:2977–2981
Rajkumar SV, Jacobus S, Callander NS, Fonseca R, Vesole DH, Williams ME et al (2010) Lenalidomide plus high-dose dexamathasone versus lenalidomide plus low-dose dexamethasone as initial therapy for newly diagnosed multiple myeloma: an open-label randomised controlled trial. Lancet Oncol 11:29–37
Dimopoulos MA, Terpos E, Chanan-Khan A, Leung N, Ludwig H, Jagannath S et al (2010) Renal impairment in patients with multiple myeloma: a consensus statement on behalf of the International Myeloma Working Group. J Clin Oncol 28:4976–4984
Johnson WJ, Kyle RA, Pineda AA, O’Brien PC, Holley KE (1990) Treatment of renal failure associated with multiple myeloma. Plasmapheresis, hemodialysis and chemotherapy. Arch Intern Med 150:863–869
Clark WF, Stewart AK, Rock GA, Sternbach M, Sutton DM, Barret BJ et al (2005) Plasma exchange when myeloma presents as acute renal failure: a randomized controlled trial. Ann Intern Med 143:777–784
Weisel KC, Heyne N, Hutchison CA, Göhl H, Risler T, Kanz L (2007) Effective light chain elimination via a high cut-off protein permeable filter in patients with light chain myeloma disease. Onkologie 30(suppl 3):80
Hutchison CA, Cockwell P, Reid S, Chandler K, Mead GP, Harrison J et al (2007) Efficient removal of immunoglobulin free light chains by hemodialysis for multiple myeloma: in vitro and in vivo studies. J Am Soc Nephrol 18:886–895
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P (2004) Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) group. Crit Care 8:R204–R212
Mehta RL, Kellum JA, Shah SV (2007) Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 11:R31
Verfoord G, Willems HL, Wetzels JF (2002) Assessment of glomerular filtration rate in healthy subjects and normoalbuminuric diabetic patients: validity of a new (MDRD) prediction equation. Nephrol Dial Transplant 17:1909–1913
Dimopoulos MA, Roussou M, Gavriatopoulou M, Zagouri F, Mikou M, Matsuoka C et al (2009) Reversibility of renal impairment in patients with multiple myeloma treated with bortezomib-based regimens. Clin Lymphoma Myeloma 9:302–306
Kidney Disease Outcomes Quality Initiative (K/DOQI) (2002) Executive summary. Am J Kidney Dis 39(suppl 1):S17–S31
Durie BG, Harousseau JL, Miguel JS, Bladé J, Barlogie B, Anderson K, International Myeloma Working Group et al (2006) International uniform response criteria for multiple myeloma. Leukemia 20:1467–1473
Dimopoulos MA, Kastritis E, Rosinol L, Bladé J, Ludwig H (2008) Pathogenesis and treatment of renal failure in multiple myeloma. Leukemia 22:1485–1493
Chanan-Khan AA, Kaufman JL, Mehta J, Richardson PG, Miller KC, Lonial S et al (2007) Activity and safety of bortezomib in multiple myeloma patients with advanced renal failure: a multicenter retrospective study. Blood 109:2604–2606
Ludwig H, Drach J, Graf H, Lang A, Meran JG (2007) Reversal of acute renal failure by bortezomib-based chemotherapy in patients with multiple myeloma. Haematologica 92:1411–1414
Ludwig H, Adam Z, Hajek R, Greil R, Tóthová E, Keil F et al (2010) Light chain-induced acute renal failure can be reversed by bortezomib-doxorubicin-dexamethasone in multiple myeloma: results of a phase II study. J Clin Oncol 28:4635–4641
Dimopoulos MA, Christoulas D, Roussou M, Kastritis E, Anagnostou D, Koureas A et al (2010) Lenalidomide and dexamethasone for the treatment of refractory/relapsed multiple myeloma: dosing of lenalidomide according to renal function and effect on renal impairment. Eur J Haematol 85:1–5
Dimopoulos M, Alegre A, Stadtmauer EA, Goldschmidt H, Zonder JA, de Castro CM et al (2010) The efficacy and safety of lenalidomide plus dexamethasone in relapsed and/or refractory multiple myeloma patients with impaired renal function. Cancer 116:3807–3814
Matsue K, Fujiwara H, Iwama KI, Kimura S, Yamakura M, Takeuchi M (2010) Reversal of dialysis-dependent renal failure in patients with advanced multiple myeloma: single institutional experiences over 8 years. Ann Hematol 89:291–297
Kastritis E, Anagnostopoulos A, Roussou M, Gika D, Matsuoka C, Barmparousi D et al (2007) Reversibility of acute renal failure in newly diagnosed multiple myeloma patients treated with high dose dexamethasone containing regimens and the impact of novel agents. Haematologica 92:546–549
Wynckel A, Vuiblet V, Schneider N, Kolb B, Melin JP, Journet J et al (2010) Comparison of plasma exchange and hemodialysis using a high cut-off membrane (HCO) for removal of immunoglobulin free light chains in multiple myeloma. J Am Soc Nephrol 21:39A
Hutchison CA, Cook M, Heyne N, Weisel KC, Billingham L, Bradwell A et al (2008) European trial of free light chain removal by extended haemodialysis in cast nephropathy (EuLITE). A randomised control trial. Trials 9:55
Acknowledgements
HCO filters were provided courtesy of Gambro Dialysatoren GmbH, Hechingen, Germany.
Conflict of interest
The authors report no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heyne, N., Denecke, B., Guthoff, M. et al. Extracorporeal light chain elimination: high cut-off (HCO) hemodialysis parallel to chemotherapy allows for a high proportion of renal recovery in multiple myeloma patients with dialysis-dependent acute kidney injury. Ann Hematol 91, 729–735 (2012). https://doi.org/10.1007/s00277-011-1383-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-011-1383-0