Abstract
Objective
The anterolateral ligament (ALL) may limit tibial internal rotation and pivot-shift following anterior cruciate ligament reconstruction. Previous studies, using magnetic resonance imaging (MRI) to identify this structure, have been inconsistent. We aimed to further characterize the anatomy of this ligament with reference to previous work.
Materials and methods
Institutional Review Board approval was gained and a retrospective study of 154 consecutive 1.5-T MRI studies was performed by a consultant musculoskeletal radiologist. Cases with a lateral compartment or cruciate injury and patients under 16 years were excluded. A total of 100 MRIs (98 patients; 63 males: 35 females; mean age, 45.3 years, range, 16–85 years) were included in the study.
Results
The ALL was visualized partially in 94 (94.0 %) of the cases and fully with distinct femoral and tibial fibers in 57 (57.0 %) of the cases. Although the femoral origin was discreet in only 57 (57.0 %) of cases, the tibial insertion (7.64 ± 1.26 mm below the joint-line) and meniscal attachment were demonstrated in all cases where the ligament was seen. Where the femoral origin was not seen, a broad expansion of the ligament was noted. We identified four types of meniscal attachment (complete, central, bipolar, and inferior-only). The thickness of the ALL, at the level of the joint-line, was 1.75 ± 0.57 mm.
Conclusions
The ALL is a consistent structure with meniscal and tibial portions identifiable in the majority of MRI studies of the uninjured knee. There is an attachment to the lateral meniscus with anatomical variation described by our subclassification.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There has been much recent interest in the anterolateral ligament (ALL) of the knee. This structure has been previously described, as far back as Segond’s paper in 1879 [1], with a variety of nomenclature used [2–8]. However, it is only now that the anatomy of the ligament has been studied in detail with improved description of its attachments and dimensions [9–14]. Alongside biomechanical studies, suggesting a role in limiting tibial internal rotation on the femur [15–17], this has led to proposed reconstruction procedures to limit pivot-shift following anterior cruciate ligament (ACL) surgery [18, 19]. Furthermore, radiological studies have been performed in an effort to establish the intra-operative fluoroscopic landmarks for such procedures [20, 21]. However, the methods of detecting injury to this structure and the significance associated with this have yet to be established.
Previous studies, focusing on the magnetic resonance imaging (MRI) appearance of the ALL, have shown mixed results [22–27]. Detection has been studied in cadaveric specimens, injured and uninjured knees with small series offering inconsistent results. Particular discordance exists about the ability to visualize the femoral origin and tibial insertion of the ligament as well as the presence or absence of an attachment to the lateral meniscus. The aim of this study was to establish the normal anatomy of the ALL on MRI. We purposefully chose to exclude knees with evidence of cruciate or lateral meniscal injury to establish normality without having to contend with issues relating to injury of associated structures.
Materials and methods
We studied 154 consecutive MRI scans of the knee performed between November 1, 2014 and December 1, 2014. All the scans were performed on two 1.5-T magnets (MAGNETOM Avanto, Siemens Healthcare, Erlangen, Germany) with a dedicated knee coil. Our standard knee protocol was used in all cases: Knee imaged in a fully extended position; T1-weighted scans in the sagittal plane and proton density scans in the sagittal, coronal, and axial planes. Slice thickness was 3 mm, in the sagittal and coronal planes, and 4 mm in the axial plane.
The imaging was read by a consultant musculoskeletal radiologist with subspecialty fellowship training and 4 years of consultant experience. Reports of all 154 scans were examined and 54 scans were excluded. Exclusions were: ACL deficiency (acute tear, chronic tear, and ACL graft), lateral meniscal tear (acute tear, chronic tear, and meniscal surgery or graft), and age below 16 years. In total, 100 scans (98 patients) were included in the study. There were 63 males and 35 were females with a mean age of 45.3 years (range, 16–85 years). The indications and primary diagnoses for the included scans are summarized in Table 1. The study received Institutional Review Board approval.
The ALL was interrogated in all imaging planes and the presence of femoral, meniscal, and tibial attachments was noted. Depending on the location in the axial and coronal plane, the femoral insertion was classified into three types: at the lateral epicondyle, anterodistal to the lateral epicondyle, and posteroproximal to the lateral epicondyle.
Depending on the configuration in the coronal plane, the meniscal attachment of the ALL was classified into the following four types: complete, central, bipolar, and inferior-only.
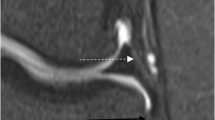
The perpendicular distance of the tibial insertion of the ALL below the joint line was measured on the coronal images from the center of the tibial insertion of the ligament to the subchondral bone surface (Fig. 1). This parameter was chosen to facilitate correlation with previous MRI, anatomical, and surgical studies.
The thickness of the ALL was measured on the coronal images at the level of the tibial subchondral bone (Fig. 1). This reflects thickness of the ligament at the level it was most consistently visualized.
Results
The results are summarized in Table 2.
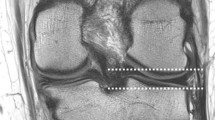
Detection: We were able to demonstrate the ALL throughout its entire length 57 cases (57.0 %) (Fig. 2). In addition, by dividing the ALL into three portions, this structure was visualized partially (in one or two of the three portions) in a further 37 cases (37.0 %). Therefore, the ALL was visualized at least partially in 94 cases (94.0 %) of the 100 cases studied.
Origin and insertion: The femoral ALL origin was seen in 57 cases (57.0 %), the meniscal portion was seen in 94 cases (94.0 %), and the tibial ALL insertion was seen in 94 cases (94.0 %) (Fig. 2).
In all cases where the femoral origin was not visualized, a broad connection to the lateral collateral ligament or iliotibial band existed (Fig. 3).
The femoral ALL origin was found to be very close to that of the lateral collateral ligament but was distinguishable, from this structure, in most. Of those cases where the origin was visible (57 cases), 56 cases (98.2 %) showed an origin directly from the lateral epicondyle of the femur and one case (1.75 %) had an origin anterodistal to the lateral epicondyle. There were no cases where the origin was posteroproximal to the lateral epicondyle.
The tibial insertion was easily identifiable in all cases where the ALL was seen (94 cases). It was found a mean distance of 7.64 ± 1.26 mm below the joint-line lying roughly half-way between Gerdy’s tubercle and the fibula head.
Meniscal attachment: An attachment to the lateral meniscus was also seen in all cases where the ALL was visualized (94 cases). The attachment was inferior-only in 30 cases (31.9 %), complete in 30 cases (31.9 %), bipolar in 29 cases (30.9 %), and central in five cases (5.32 %) (Fig. 4).
The thickness of the ALL was measured at the level of the joint line. The mean thickness was 1.75 ± 0.57 mm.
Discussion
A literature search identified six previous studies focused on the MRI appearance of the ALL. These studies, and their findings, are summarized in Table 3. Although, there is some agreement, there are also areas of disparity between these studies and the findings of our work. To our knowledge, our study represents the largest consecutive series, in the literature, reporting on the normal anatomy of the ALL.
The appearance of the ALL on MRI was first described by Caterine et al. in 2014 [13]. In their study, ten fresh-frozen cadaveric knees underwent MRI and then the findings were confirmed with both dissection and histological analysis. This group was able to identify the ALL in all ten knees. There was also good correlation between their MRI findings and those of their dissection. High detection rates on MRI were also reported by Helito et al. in 2014 [22] (demonstrating the ALL in 97.8 % of 39 uninjured knees) and Porrino et al. in 2015 [23] (100 % of 51 uninjured knees). In contrast, other groups have reported much lower rates of detection. Taneja et al., in a study of 70 consecutively performed MRIs in 2014, found evidence of the ALL (fully or partially) in only 51 % of their series [24]. Looking at the patient group in this particular study shows it was a mix of chronic and acute pain (as well as post-operative) cases. Therefore it could be suggested that the lower detection rate was related to previous injury to the ALL. Indeed, Claes et al., in 2014, only identified the ALL in 76.0 % of 271 ACL-deficient knees [25]. However, other studies have not confirmed this effect of injury to the ALL (alongside an injury to the ACL) on detection. Wodicka et al., in 2014, were able to readily identify the ALL in 100 % of 50 ACL-deficient knees and found evidence of a grade 3 disruption of the ALL in only one of their cases [26]. Therefore, it appears that other factors (such as chronicity of the injury and timing of the MRI) may be of importance. Our demonstration of the ALL (at least partially) in 94.0 % of the cases compares well to previous studies in the uninjured knee. A recent systematic review (including all of the above work) found detection of the ALL on MRI in 93.0 % of cases in their pooled analysis [27]. However, clearly the effect of injury to the knee on this detection rate requires further investigation.
In our study, in all cases when the ALL was identified, the tibial insertion and meniscal portion of the ligament were clearly seen. The relative ease of visualizing these portions of the ALL is confirmed by other studies. Caterine et al. [13] found the tibial and meniscal portions were “easily visible” and Taneja et al. [24] reported visualizing both segments in all cases where they identified the ALL. We found the insertion to be 7.64 mm below the joint line. Again, this shows good agreement with previous MRI studies (Helito et al. [22] and Taneja et al. [24]) as well as anatomical dissection studies that have shown similar measurements. In contrast to our results, Helito et al. [22] were unable to visualize the tibial portion of the ALL in one-fifth of their cases and Porrino et al. [23] found the distal portion of the ALL to be indistinguishable from the iliotibial band in the cases they studied. The reason for this discrepancy is not entirely obvious. It may be suggested that the position of the knee and specific sequences make this easier to determine. Our experience suggests that although the ALL is close to the posterior border of the iliotibial band, clear fibers are visible that define the ALL as a separate structure inserting halfway between Gerdy’s tubercle and the fibula head.
There seems to be agreement, in all published series, that the femoral origin of the ligament is less easily seen. We were only able to visualize this section clearly in 57 (57.0 %) of our cases (60.6 % of cases where any part of the ALL was seen). Although Helito et al. [22] report demonstration of the femoral attachment on 89.7 % of the knees studied, Caterine et al. [13], Taneja et al. [24], and Porrino et al. [23] all found that this was difficult to distinguish from adjacent structures. In the cases where we were unable to clearly define this portion of the ligament, we were able to see a broadened attachment to either the lateral collateral ligament or the iliotibial band superiorly. This seems to represent the “thin and somewhat ill-defined meniscofemoral attachment” reported by Porrino et al. in their study [23]. However, opposed to the findings of this last group, in the remainder of our cases, the femoral portion of the ALL was much more obvious. The significance of this variation has not been previously discussed. Therefore, the specific mechanical properties of the broadened attachment, versus the more defined origin, may warrant further investigation. Where seen as a discreet attachment, the femoral origin came most commonly (98.2 % of the time) from the lateral epicondyle of the femur. This fits with the results of cadaveric anatomical studies including Caterine et al. who, in the dissection arm of their study, found the origin to be either anterodistal or proximoposterior to the epicondyle [13]. We found it difficult to differentiate the origin to this degree of detail, due to the broadening of the footprint at this level and proximity of adjacent structures. Similar difficulties have been expressed by other authors using MRI to study this ligament [23, 24]. Therefore, using this modality, it may be that the attachment can be most usefully approximated to the lateral epicondyle.
The evidence of an attachment of the ALL to the lateral meniscus is another area of disagreement both in MRI and dissection studies. The two radiologists that reviewed images in the study by Taneja et al. found no evidence of a meniscal attachment in any case [24]. Similarly, Dodds et al., in their dissection of 40 cadavers in 2014, suggested that no such connection existed [12]. In conflict with this, our study not only demonstrates the existence of an attachment, in the majority of our cases (94.0 %), but also that these can be subclassified into four separate groups. Caterine et al, [13] Helito et al. [22] and Porrino et al. [23] all found similar attachments in the majority (or all) of their cases. Interestingly, Helito et al. showed a bifurcation in the ALL (3.0 mm above the lateral meniscus) separating the ligament into meniscofemoral and meniscotibial portions [22]. This “superior-only” attachment is not described in any of our groups, but the images published in their study appear similar to our “bipolar” subclassification with our results putting more emphasis on an inferior connection. Helito et al. were also able to show the inferior lateral geniculate artery passing between the meniscus and the ALL (causing branching of the attachment around it) [22]. Although we were able to visualize this relationship in some cases, in others these vessels were less obvious. The attachment found in all of the knees in Porrino et al.’s study [23] (although not clearly defined) suggests an appearance similar to the “complete” seen in our series. Alongside this, cadaveric dissection studies, which support the finding of a meniscal attachment, have not described the variety that our study has noted. However, the detail of this may be less obvious macroscopically and may be affected by the dissection technique. Therefore, MRI may be the optimal modality to further study this. The clinical significance of this subclassification is not yet fully known. It may be that particular attachment patterns are mechanically stronger and this may have significance in the pattern of injury (to both the ALL and the lateral meniscus) that is observed in the injured knee. This is an area for potential further research in the ACL-deficient knee. What is important, given that this is a consistent finding, is that consideration is given to the meniscal attachment in any planned reconstruction procedure.
Potential limitations of our study include the strength of the MRI magnetic field strength used and the interpretation of the images by only a single observer. However, both of these factors may have limited effect on the validity of our results. We used a 1.5-T scanner and this is similar to the groups we have used for comparison [22, 24, 25]. Other groups have used a 3-T magnetic field strength [13, 23] and one might assume that the detection rate would be higher with this. However, high detection rates (and definition of the attachments of the ALL) have been reported with both 1.5-T and 3-T scanners and the only group to compare the two strengths found no difference in the detection rates [24]. Similarly, although other studies have used more than one observer to assess MRI scans, reported inter-observer correlation has been shown to be either “significant” (ƙ = 0.70) [24] or “almost perfect” (ƙ = 0.843–1.000) [22]. Intra-observer error has not been previously studied. Although this was not formally assessed in our study, we believe this would show similar high levels of agreement.
In addition, the position of the knee, thickness of MRI slices and patient factors may affect detection rates. Using thicker slices may limit the ability to distinguish between adjacent structures while thinner slices make visualizing oblique structures (such as the ALL) more difficult. It is difficult to conclusively compare other groups’ methods to our standard knee protocol and ensure the patient groups are similar. Therefore, some of the comparisons made (and conclusions drawn) may not be valid for all patient groups.
We have shown the ALL to be a consistent structure with meniscal and tibial portions identifiable on MRI studies of the uninjured knee. Evidence of an attachment to the lateral meniscus in all cases (when the ligament was seen) was demonstrated although the clinical significance of our subclassification is not yet known.
References
Segond P. Recherches cliniques et expérimentales sur les épanchements sanguins du genou par entorse. Progrès Médical. 1879;1–85.
Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities: Part II – The lateral compartment. J Bone Joint Surg Am. 1976;58:173–9.
Terry GC, Hughston JC, Norwood LA. The anatomy of the iliopatellar band and iliotibial tract. Am J Sports Med. 1986;14:39–45.
Irvine GB, Dias JJ, Finlay DB. Segond fractures of the lateral tibial condyle: brief report. J Bone Joint Surg (Br). 1987;69:613–4.
Campos JC, Chung CB, Lektrakul N, et al. Pathogenesis of the Segond fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology. 2001;219:381–6.
Vieira EL, Vieira EA, da Silva RT, et al. An anatomic study of the iliotibial tract. Arthroscopy. 2007;23:269–74.
Johnson LL. Lateral capsular ligament complex: anatomical and surgical considerations. Am J Sports Med. 1979;7:156–60.
Sanchez II AR, Sugalski MT, LaPrade RF. Anatomy and biomechanics of the lateral side of the knee. Sports Med Arthrosc Rev. 2006;14:2–11.
Vincent JP, Magnussen RA, Gezmez F, et al. The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc. 2012;20:147–52.
Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321–8.
Helito CP, Demange MK, Bonadio MB, et al. Anatomy and histology of the knee anterolateral ligament. Orthop J Sports Med. 2013;1:1–5.
Dodds AL, Halewood C, Gupte CM, Williams A, Amis AA. The anterolateral ligament: anatomy, length changes and association with the Segond fracture. Bone Joint J. 2014;96:325–31.
Caterine S, Litchfield R, Johnson M, Chronik B, Getgood A. A cadaveric study of the anterolateral ligament: re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc. 2014 [Epub ahead of print]
Stijak L, Bumbasirevic M, Radonjic V, et al. Anatomical description of the anterolateral ligament of the knee. Knee Surg Sports Traumatol Arthrosc. 2014 [Epub ahead of print]
Ayeni O, Chahal M, Tran M, Sprague S. Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20:767–77.
Jonsson H, Riklund-Ahlstrom K, Lind J. Positive pivot shift after ACL reconstruction predicts later osteoarthrosis. Acta Orthop Scand. 2004;75:594–9.
Monaco E, Ferretti A, Labianca L, et al. Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol Arthrosc. 2012;20:870–7.
Wroble RR, Grood ES, Cummings JS, Henderson JM, Noyes FR. The role of the lateral extraarticular restraints in the anterior cruciate ligament-deficient knee. Am J Sports Med. 1993;21:257–62.
Monaco E, Maestri B, Conteduca F, Mazza D, Iorio C, Ferretti A. Extra-articular ACL reconstruction and pivot shift—in vivo dynamic evaluation with navigation. Am J Sports Med. 2014;42:1669–74.
Rezansoff AJ, Caterine S, Spencer L, Tran MN, Litchfield RB, Getgood AM. Radiographic landmarks for surgical reconstruction of the anterolateral ligament of the knee. Knee Surg Sports Traumatol Arthrosc. 2014 [Epub ahead of print]
Helito CP, Demange MK, Bonadio MB, et al. Radiological markers for locating the femoral origin and tibial insertion of the knee anterolateral ligament. Am J Sports Med. 2014;42:2356–62.
Helito CP, Helito PV, Costa HP, et al. MRI evaluation of the anterolateral ligament of the knee: assessment in routine 1.5-T scans. Skeletal Radiol. 2014;43:1421–7.
Porrino Jr J, Maloney E, Richardson M, Mulcahy H, Ha A, Chew FS. The anterolateral ligament of the knee: MRI appearance, association with the Segond fracture, and historical perspective. Am J Roentgenol. 2015;204:367–73.
Taneja AK, Miranda FC, Braga CA, et al. MRI features of the anterolateral ligament of the knee. Skeletal Radiol. 2015;44:403–10.
Claes S, Bartholomeeusen S, Bellemans J. High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belg. 2014;80:45–9.
Wodicka R, Jose J, Baraga MG, et al. MRI evaluation of the anterolateral ligament of the knee in the setting of ACL rupture. Orthop J Sports Med. 2014;2:Suppl2.
Van der Watt L, Khan M, Rothrauff BB, et al. The structure and function of the anterolateral ligament of the knee: a systematic review. Arthroscopy. 2015;31:569–82.
Conflict of interest
The author(s) declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kosy, J.D., Mandalia, V.I. & Anaspure, R. Characterization of the anatomy of the anterolateral ligament of the knee using magnetic resonance imaging. Skeletal Radiol 44, 1647–1653 (2015). https://doi.org/10.1007/s00256-015-2218-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-015-2218-1