Abstract
Objectives
To compare safety and clinical outcomes of embolization of the superior rectal arteries in patients with hemorrhoidal bleeding using particles and coils versus coils only.
Methods
We retrospectively reviewed data for patients undergoing embolization for chronic hemorrhoidal bleeding from January 2014 to April 2017. Embolization was performed with coils alone or with particles and coils. Clinical scores (Paris bleeding severity score, Goligher classification and quality of life score) were obtained, and embolization was performed with microparticles (300–500 μm) followed by fibered pushable coils. Clinical success was defined as an improvement of > 2 points in the Paris bleeding severity score, without complications. Outcomes were compared between the two groups in a matched-pairs analysis (1:1 scenario), with patients embolized with particles and coils as the study group and patients embolized with coils alone as the control.
Results
We treated 45 consecutive patients. After matched-pairs analysis, the final study population was 38 patients (19 study group and 19 controls). Clinical success did not differ significantly between the two populations: 63% for control group and 68% for the study group (p = 0.790). The median change in clinical score was − 3 [− 6; − 1] for the control group and − 3 [− 4; − 1] for the study group (p = 0.187). Grade 1 complications were reported in 15% of patients, with no major complications.
Conclusions
Embolization was feasible, with a technical success of 100% and no major complications. Clinical success was obtained in 66% in patients with no difference when using combined embolization with particles and coils versus coils only.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, significant progress has been made toward understanding the pathophysiology of hemorrhoidal disease, including its vascular component, in particular [1].
This progress has led to the development of new procedures targeting hemorrhoidal hyperplasia, such as Doppler-guided hemorrhoidal artery ligation (DG-HAL) and the endovascular embolization of hemorrhoidal arteries [2, 3].
We previously reported our experience with hemorrhoidal artery embolization with coils in patients ineligible for surgery presenting with chronic hemorrhoidal bleeding and obtained a mid-term clinical success rate of 72% without complications [4]. This success rate is consistent with the results presented by Tradi et al. [5] in a prospective study in which symptom improvement and patient satisfaction rate of 72% at 12 months were reported using embolization as a first-line treatment.
Although this figure is already satisfactory, it also means that up to 30% of patients experience clinical failure with the current technique and that there may be room for improvement. We therefore decided to evaluate another approach based on a combination of microparticles and coils.
The primary objective of this study was to assess the feasibility and safety of embolization with a combination of particles and coils. The secondary objective was to assess clinical outcomes for embolization with a combination of particles and coils and to compare these outcomes with those for coils only.
Materials and Methods
From January 2014 to April 2015, consecutive patients underwent coil embolization. Patients treated from April 2015 to April 2017 underwent embolization with both particles and coils. The study group consisted of the patients undergoing embolization with both particles and coils, whereas the control group consisted of those treated with coils alone.
All patients were referred for embolization after a consensus had been reached between the proctologist and the interventional radiologist. Clinical evaluation comprised proctological examination and a clinical assessment based on a specific bleeding scale (the Paris bleeding severity score—Appendix 1) [4], Goligher’s classification (Appendix 2) and the quality of life score (Appendix 3).
The procedures were performed by a senior interventional radiologist, trained in hemorrhoidal embolization technique.
In the control group (coils only), embolization was performed using coils to occlude the distal branches of the superior rectal arteries. Based on comparison of the microcatheter diameter and the arterial diameter, we could estimate the caliber of the target artery which conducted to use 2–3 mm, 0.018-inch fibered pushable coils (Cook Nester, Bloomington, Indiana, USA) delivered though a 2.7 Fr microcatheter (Progreat microcatheter Radiofocus—Terumo) inserted into the inferior mesenteric artery via a 5F percutaneous femoral approach. The aim of the embolization was complete occlusion of all branches of the superior rectal artery just above the pubic ramus, as close to the corpus cavernosum recti as possible.
The intervention was performed under local anesthesia, in the angiography room, in patients admitted to the day care hospital. During the intervention, patients received an IV bolus of 3000–5000 IU of heparin. No specific sedation or prophylactic antibiotic treatment was administered. The puncture site was closed with a closure device, and the patient was allowed to leave the hospital after 3 h of monitoring by a specialist nurse.
In the study group (embolization with particles + coils), a diluted mixture of Embosphere® 300–500 μm (Merit Medical, Salt Lake City, USA) was first injected, with a 2.7 Fr microcatheter positioned as close as possible to the hemorrhoidal plexus until blood flow reduction. Then, like in the control group, all branches were then blocked with 0.018-inch fibered pushable coils until complete stasis.
Technical data of the procedure are summarized in Table 2.
After embolization, the patients were clinically followed by an interventional radiologist and a proctologist, to assess symptom change (Paris bleeding severity score, Goligher classification and quality of life score) and to record any complications, at 1 month, 3 months, 6 months and 1 year after the intervention.
Technical success was defined as the occlusion of all visible branches of the superior rectal artery.
Clinical success was defined as an improvement in clinical scores after embolization (by > 2 points for the Paris score for bleeding severity), without severe complications, as previously described [4].
The clinical results for patients treated with particles and coils were compared with those for patients treated with coils alone, in a matched-pair analysis (1:1 scenario) [6].
All patients gave informed consent for embolization treatment, and the study was approved by the appropriate institutional review board.
Statistical Analysis
The matching parameters were pretreatment clinical scores (Paris bleeding score, Goligher’s prolapse classification and quality of life).
Descriptive statistics were used to report the characteristics of the patients. Paired t tests or Wilcoxon matched-pairs signed-rank tests were used for continuous variables, and McNemar’s Chi-squared tests were used for discrete variables, for between-group comparisons. Signed-rank tests were used to compare pre- and post-treatment clinical scores within groups and score changes between groups.
We used SPSS version 23 for statistical analysis (IBM Corp., NY). Data are expressed as mean ± SD, median (IQR) or n (%). p values of 0.05 or below in two-tailed tests were considered to indicate statistical significance.
Results
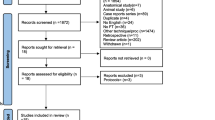
Between January 2014 and April 2017, we treated 45 consecutive patients, 25 with coils alone, and 20 with both particles and coils. We performed a matched-pair analysis (1:1 scenario), in which the study population was reduced to 38 patients (19 with coils alone, 19 with both particles and coils), with no significant differences for the matching variables, as shown in Table 1.
The main technical features of embolization are summarized in Table 2.
Clinical success, defined as an improvement of more than 2 points in Paris bleeding score, did not differ between the two populations: 63% (12/19) for the control group (coils only) and 68% (13/19) for the study group (p = 0.790; Fig. 1).
The median change in clinical score was − 3 [− 6; − 1] for the control group and − 3 [− 4; − 1] for the study group (p = 0.187) (Table 3).
In the study group, three patients were retreated after clinical failure of the first embolization of the superior rectal artery with coils alone. Then, embolization of the middle rectal artery (anatomical variant issuing the internal iliac artery and vascularizing hemorrhoidal plexus) with particles and coils was clinically successful in two of these patients (Fig. 2). In the remaining patient, no improvement in symptoms was observed despite two sessions of embolization with particles and coils.
Hemorrhoidal embolization in a 70-year-old man under oral coagulant treatment for mechanical mitral valve and suffering of chronic hemorrhoidal bleeding responsible of anemia. A Selective angiography of the inferior mesenteric artery; communication with the middle rectal arteries coming from the internal iliac network is noted bilaterally (arrow). B Embolization with eleven coils until complete occlusion of the superior rectal arteries. After initial bleeding stop, the patient is referred 1 year later for bleeding recurrence. C Initial angiography shows complete embolization of the superior rectal arteries. D Forceful selective injection into the right superior rectal artery shows a remaining communication with the middle rectal artery coming from the internal iliac network (arrow head). E Selective angiography of the right middle rectal artery (white arrow show the tip of the microcatheter). F Direct embolization of right middle rectal artery via the internal iliac network with particles and coils until complete occlusion
There was no patient requiring retreatment in the control group.
Two patients for whom embolization with particles and coils yielded an unsatisfactory clinical result received additional treatment involving mini-invasive procedures: hemorrhoidopexy for one and rubber band ligation for the other.
After embolization, 15% of patients reported grade 1 complications (“no deviation from the normal post therapeutic course”) [7]; all of them in the group embolized with particles, consisting of mild pain and bleeding (related to the intervention because they all occurred within 3 days post-embolization), and which resolved with symptomatic treatment.
Discussion
In this study comparing the safety and clinical outcomes of embolization of the superior rectal arteries in patients with hemorrhoidal bleeding, we found no difference between embolization using particles and coils versus coils only.
A clinical success rate of 68% was recorded for embolization with a combination of particles and coils.
This is in contradiction with Zakharchenko et al. [8], who used embolization with 300 µm calibrated particles, reported higher patient satisfaction of 83–94% with no anorectal ischemia, and a decrease in blood flow through the hemorrhoidal arteries from 109 ± 1.2 ml/min/100 g (SD) before treatment to 60.2 ± 4.4 ml/min/100 g (SD) after treatment (p < 0.05).
We can assume that this difference in clinical success, with a higher patient satisfaction rate in their study, may be related to the longer period of follow-up in our group, which may reveal more bleeding recurrence that were not specified in his paper.
Also, this could be explained by the subjective nature of symptom evaluation and the absence of use of specific evaluation scale.
In addition, because he does not use a validated scale allowing to evaluate in a reproducible manner, the severity of bleeding and the overall clinical success may be perceived as higher. The Paris score that our group has developed is under final review and allows better comparison of techniques in the future.
In addition, last but not least, our study was not randomized, and only matched-pairs analysis could be performed.
These results, if confirmed in other setting, could seem in relative contradiction to the current physiopathology explanation of hemorrhoidal bleeding.
Indeed, disease development and hemorrhoidal bleeding result partly from hyperplasia of the hemorrhoidal plexus, a site of increased blood flow [1]. The goal of embolization is, therefore, to reduce this excessive blood flow, to decrease hyperplasia and bleeding.
The hemorrhoid plexus is also a site of arteriovenous communication [9, 10]. More distal embolization would be likely to close these arteriovenous communications more effectively.
Then, one could suppose that the use of particles would allow more distal embolization and thus improve clinical results. It is still possible that going deeper in corpus cavernosum recti with other embolic material (liquid embolic) would bring better results. This is still to be clinically tested.
In our study, all patient with grade 1 complications after embolization (pain, bleeding) demonstrated clinical success. These complications, rapidly resolved after embolization, may be a sign of more distal and perhaps more effective embolization of the hemorrhoidal arteriovenous communication as we had significantly more grade 1 complications in the particles groups.
One area of potential progress, beyond change of embolics, could be a better understanding of the middle rectal artery.
The hemorrhoid plexus is usually vascularized by the superior rectal artery arising from the inferior mesenteric artery. However, anatomical variants occur in some patients, with the middle rectal artery, inconstant, arising from the internal iliac artery, acting as the main artery vascularizing the hemorrhoidal plexus.
We embolized the middle rectal artery in cases in which this variant was identified directly by angiography, indeed it is possible to find a hemorrhoidal plexus vascularized principally by one or both middle rectal arteries and a low intake of blood from the superior rectal artery in the hemorrhoidal plexus.
Sun et al. [11] recently reported a clinical success rate of 91% without complications after the complete occlusion, with coils, of the superior and middle rectal arteries when a connection was found (a unilateral connection in 13.04% and bilateral in 30.43% of patients). They recommended angiography and embolization of both the superior and middle rectal artery.
This is in accordance with our experience; we had three cases of failure after a first embolization of the superior rectal artery, and then embolization of the middle rectal artery was clinically successful in two of these patients. This suggests that distal and complete embolization of all arteries vascularizing the hemorrhoids is needed to improve the symptoms of patients.
We now recommend embolization of the middle rectal artery in first intention if the main blood intake seems to be coming from the middle rectal artery with a thin superior rectal artery.
Finally, like all mini-invasive hemorrhoidal techniques, embolization treats only internal hemorrhoidal disease. Careful patient selection is therefore crucial to reduce failure rates, regardless of the technique used.
To date, we do not have enough argument to recommend hemorrhoidal embolization by particles and coils, as we cannot demonstrate significant clinical benefit compared to embolization by coils alone.
However, further investigation is needed in order to conclude on the interest of particles in hemorrhoidal embolization.
Conclusion
We report the outcomes of embolization with particles and coils for hemorrhoidal bleeding.
This technique was feasible, with a technical efficiency of 100% and no major complications.
No significant difference was observed in the change in clinical success between patients embolized with particles and coils and those embolized with coils only, with an overall clinical success rate of 66% (25/38).
Abbreviations
- DG-HAL:
-
Doppler-guided hemorrhoidal artery ligation
- N:
-
Number
- SD:
-
Standard deviations
- IQR:
-
Interquartile ranges
- QOL:
-
Quality of life
- PDS:
-
Dose area product
References
Aigner F, Bodner G, Gruber H, et al. The vascular nature of hemorrhoids. J Gastrointest Surg Off J Soc Surg Aliment Tract. 2006;10:1044–50. https://doi.org/10.1016/j.gassur.2005.12.004.
Vidal V, Louis G, Bartoli JM, Sielezneff I. Embolization of the hemorrhoidal arteries (the emborrhoid technique): a new concept and challenge for interventional radiology. Diagn Interv Imaging. 2014;95:307–15. https://doi.org/10.1016/j.diii.2014.01.016.
Vidal V, Sapoval M, Sielezneff Y, et al. Emborrhoid: a new concept for the treatment of hemorrhoids with arterial embolization: the first 14 cases. Cardiovasc Intervent Radiol. 2014. https://doi.org/10.1007/s00270-014-1017-8.
Moussa N, Sielezneff I, Sapoval M, et al. Embolization of the superior rectal arteries for chronic bleeding due to haemorrhoidal disease. Colorectal Dis Off J Assoc Coloproctology G B Irel 2017;19:194–99. https://doi.org/10.1111/codi.13430.
Tradi F, Louis G, Giorgi R, et al. Embolization of the superior rectal arteries for hemorrhoidal disease: prospective results in 25 patients. J Vasc Interv Radiol JVIR. 2018;29:884–92. https://doi.org/10.1016/j.jvir.2018.01.778.
Pearce N. Analysis of matched case-control studies. BMJ. 2016;352:i969.
Filippiadis DK, Binkert C, Pellerin O, et al. Cirse Quality Assurance Document and Standards for Classification of Complications: the Cirse Classification System. Cardiovasc Intervent Radiol. 2017;40:1141–6. https://doi.org/10.1007/s00270-017-1703-4.
Zakharchenko A, Kaitoukov Y, Vinnik Y, et al. Safety and efficacy of superior rectal artery embolization with particles and metallic coils for the treatment of hemorrhoids (Emborrhoid technique). Diagn Interv Imaging. 2016;97:1079–84. https://doi.org/10.1016/j.diii.2016.08.002.
Parnaud E, Guntz M, Bidart JM, Bernard A, Chome J. Considération sur la vascularisation normale de la sous muqueuse anale. Rev Proct. 1981;1:44–54.
Aigner F, Gruber H, Conrad F, et al. Revised morphology and hemodynamics of the anorectal vascular plexus: impact on the course of hemorrhoidal disease. Int J Colorectal Dis. 2009;24:105–13. https://doi.org/10.1007/s00384-008-0572-3.
Sun X, Xu J, Zhang J, et al. Management of rectal bleeding due to internal haemorrhoids with arterial embolisation: a single-centre experience and protocol. Clin Radiol. 2018;73:985.e1–6. https://doi.org/10.1016/j.crad.2018.07.105.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the appropriate institutional review board.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Guarantor
The scientific guarantor of this publication is Pr Marc SAPOVAL.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moussa, N., Bonnet, B., Pereira, H. et al. Mid-Term Results of Superior Rectal Artery and Coils for Hemorrhoidal Embolization with Particles Bleeding. Cardiovasc Intervent Radiol 43, 1062–1069 (2020). https://doi.org/10.1007/s00270-020-02441-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-020-02441-5