Abstract
Purpose
This study was designed to investigate the clinical outcome of patients with irresectable, intrahepatic cholangiocarcinoma (IHC) treated with computed tomography (CT)-guided HDR-brachytherapy (CT-HDRBT) for local tumor ablation.
Method
Fifteen consecutive patients with histologically proven cholangiocarcinoma were selected for this retrospective study. Patients were treated by high-dose-rate internal brachytherapy (HDRBT) using an Iridium-192 source in afterloading technique through CT-guided percutaneous placed catheters. A total of 27 brachytherapy treatments were performed in these patients between 2006 and 2009. Median tumor enclosing target dose was 20 Gy, and mean target volume of the radiated tumors was 131 (± 90) ml (range, 10–257 ml). Follow-up consisted of clinical visits and magnetic resonance imaging of the liver every third month. Statistical evaluation included survival analysis using the Kaplan–Meier method.
Results
After a median follow-up of 18 (range, 1–27) months after local ablation, 6 of the 15 patients are still alive; 4 of them did not get further chemotherapy and are regarded as disease-free. The reached median local tumor control was 10 months; median local tumor control, including repetitive local ablation, was 11 months. Median survival after local ablation was 14 months and after primary diagnosis 21 months.
Conclusion
In view of current clinical data on the clinical outcome of cholangiocarcinoma, locally ablative treatment with CT-HDRBT represents a promising and safe technique for patients who are not eligible for tumor resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intrahepatic cholangiocarcinoma (IHC) is a rare primary liver tumor that arises out of the epithelial cells of the bile ducts [1]. Of the primary liver malignancies, it is the second most common tumor having a stake of 10%. Of all malignancies, IHC accounts for <1 percent with a rising incidence in Europe and Northern America [2].
IHC usually present at advanced tumor stages, and due to rapid progression, they are not eligible for primary resection [3]. Surgery represents the only curative option for patients with IHC with the goal of tumor-free resection margins, but there is no evidence for prolonged survival after noncurative resection or tumor debulking [4]. Current 5-year survival rates after curative surgery range from 20 to 40% [5, 6], but even with primary tumor resection the amount of hepatic tumor recurrence is high with reported recurrence rates to 70%. However, because of rapid tumor growth and often late detection, resectability rates are low [7, 8]. The reported median survival after liver surgery ranges from 12 to 36 months compared with 6–12 months in patients with irresectable disease [8–10].
In the palliative situation, the actual standard systemic chemotherapy consists of a combination of gemcitabine and cisplatin. The overall survival in a randomized phase III study with 410 patients was 11.7 months for the gemcitabine/cisplatin patients versus 8.1 months in the gemcitabine alone group, which demonstrates a significant improvement for the combination therapy [11].
Local ablative treatment options are gaining attention as adjuncts to surgery and chemotherapy. The majority of these procedures use thermal energy for local tumor cell destruction generated by radiofrequency (RFA) [12, 13], laser (LITT) [14] or microwave (MWA) [15]. These procedures are only rarely feasible in IHC, which are mostly large in diameter at diagnosis. The presence of microinvasion of the surrounding tissue, not visible on diagnostic imaging, may result in a high rate of local progression after thermoablative procedures because of remaining viable tumor beyond the range of the ablation zone [16]. Cholangiocarcinomas arise regularly from the large bile ducts, which are adjacent to the major vessels. The perfusion of large vessels leads to convective heat loss (cooling effect) during thermal ablation, possibly resulting in an incomplete ablation. In consequence, therapeutic options and treatment success are very limited in IHC and new therapeutic approaches urgently need to be developed and assessed.
The technique of CT-guided high-dose-rate brachytherapy (CT-HDRBT) of hepatic malignancies was established in 2002 and has been used since then with promising outcome, e.g., in colorectal cancer metastases or hepatocellular carcinoma [17, 18]. CT-HDRBT has proven valuable especially in those lesions unfavorable for RFA because of large diameters (up to 10–13 cm), complex shape, or close relation to central bile ducts or vessels, conditions that are common in irresectable IHC [19].
This retrospective study analyzed the clinical outcome of patients with primary IHC, classified as unsuitable for surgery by our surgical department, treated by CT-HDRBT. It was our intent to analyze retrospectively the clinical outcome of these patients and thereby elucidate new strategies for these patients with overall poor prognosis and few therapeutic options.
Methods
This retrospective analysis included all patients with locally irresectable IHC without extrahepatic disease (as determined by CT) treated by CT-HDRBT at our institution between January 2006 and June 2009. All tumors were histologically proven by biopsy. Irresectability was determined by institutional surgeons. Indication for local tumor ablation was confirmed by an interdisciplinary tumor board, and written informed consent was obtained from each patient before the procedure. Important contraindications applied to brachytherapy candidates were total bilirubin >2.5 mg/dl (after internal biliary drainage if severe cholestasis was present), multiple, disseminated liver lesions (n > 5), uncorrectable impaired coagulation, and massive ascites. In contrast to thermal ablation CT-HDRBT, the maximal size of the ablation zone is limited by adjacent radiosensitive organs or structures (e.g., intestine) and by a sufficient remaining liver volume with a radiation below 10-Gy dose. In case of adjacent radiosensitive structures and organs, an adjusted arrangement of brachytherapy catheters could overcome this limitation; the volume limitation could be solved by a treatment in two sessions with a hepatic recovery time of 4–6 weeks in-between. Using CT-HDRBT lesions up to 10–15 cm could be treated, overcoming the size limit of thermal ablation, which is generally reported with 5 cm.
Standard treatment planning consisted of a liver MRI with hepatocytespecific contrast agent (Gd-EOB-DTPA, Primovist, Bayer, Leverkusen, Germany) 1 day in advance to CT-HDRBT to assess technical feasibility. The insertion of brachytherapy catheters into the tumor was performed under analgosedation (midazolam and fentanyl) and local anesthesia (lidocaine). Under CT-fluoroscopic guidance, a direct percutaneous transhepatic puncture and insertion of 6F angiographic sheaths (Terumo, Tokyo, Japan) with standard length of 27.5 cm in Seldinger’s technique into the tumor was performed. Through these sheaths, the closed-ended 6F afterloading catheters (Primed, Halberstadt, Germany) were introduced into the tumor. Arrangement of catheters depended on the size and shape of the lesion and anatomic limitations (e.g., pleural space, adjacent stomach, or spinal cord). Contrast-enhanced CT scans with the catheters in situ were used for further planning, performed by a radiologist and radiation oncologist in consensus. The 3D data were transferred to a radiation planning workstation (Brachyvision, Varian Medical Systems, Palo Alto, CA). Clinical target volume (CTV) was defined as the visible tumor borders in contrast-enhanced CT scans, including the enhancing rim. Catheters, clinical target volume (CTV), and potential risk structures were registered manually followed by semiautomatic calculation of the brachytherapy plan consisting of dwell times and dwell locations of an Iridium-192 source (Gammamed 12i, Varian Medical Systems) inside the catheters to cover the CTV with the intended minimal dose. The desired CTV enclosing dose was 20 Gy, but it was reduced in particular cases with adjacent structures at risk. In the central parts of the tumor doses >50 Gy were accepted. Examples of CT-HDBRT planning are shown in Figs. 1 and 2. In case of very large tumor volume, the clinical target volume was spitted and the partial clinical target volumes were treated one after the other with an interval of 4–6 weeks, allowing the surrounding liver parenchyma to recover. During retraction of the catheters after completion of the brachytherapy procedure, the puncture channels were sealed with resorbable, thrombogenic material (Gelfoam, Pfizer Inc., New York, NY) to avoid bleeding.
The routine follow-up consisted of clinical visits (including tumor marker Ca19–9) and liver MRI with Gd-EOB 6 weeks, 12 weeks, and then every third month after therapy completion (Figs. 1, 2). Additionally CTs of the chest were performed every 6 months. In cases with local tumor progression eligible for repetitive local ablation, patients underwent repetitive brachytherapy to provide “assisted” local tumor control. Local control rates, assisted local control rates, time to progression, patient survival, complications (according to the SIR classification), and additional therapies were documented.
The liver of a 77-year-old patient presenting with a large intrahepatic mass infiltrating segments 2, 3, 4, and 8 of the liver. The left branch of the portal vein showed a thrombosis was infiltrated and the patient was classified irresectable by the institutional surgeons due to an infiltration of the hilum (A). The tumor was treated by CT-HDRBT, in two separate initial sessions, using two catheters in each session. In the first session the right and superior part was treated (B), followed by the lateral and lower parts 6 weeks later (C). The central dark line indicates the clinical target volume, the first surrounding line indicates the 20-Gy isodose. After 3 months the tumor showed a beginning shrinkage (D), 12 months later (E) and after 24 months (F) shrinkage of the tumor is visible with nearly a complete scar in the location of the tumor. Probably due to the radiation and the adjacent portal vein thrombosis the left lobe of the liver shows nearly complete shrinkage with residual local cholestasis
Liver of a 60-year-old patient with irresectable central intrahepatic cholangiocarcinoma (arrow) 8 cm in diameter, which is surrounding all three draining hepatic veins (A). The tumor was treated by CT-HDRBT using a total of four brachytherapy catheters with a tumor-surrounding isodose of 20 Gy (B). After 3 months, the tumor shows beginning shrinkage (arrowheads) and a small area of reduced liver-function, which is demarked by a lowered Gd-EOB enhancement (C). After 9 months, the primary tumor (arrowheads) shows further shrinkage (D) without significant biliary obstruction, indicating that all draining intrahepatic bile ducts were patient. Hepatic veins were included in the radiated tumor mass, but venous drainage was still patent without hepatic vein thrombosis. Nine months after CT-HDRBT, two new lesions with increase of Ca19-9 were detected (E). These metastases were treated by a repetitive CT-HDRBT (F). Altogether five repetitive treatments were performed because of new metastases and an assisted tumor control period without extrahepatic tumor activity of 19 months could be reached. The patient died 28 months after initial CT-HDRBT
Statistical analysis was performed using Graph Prism Version 4 and Sigmaplot Version 8 (SPSS, Chicago, IL). Influence on patients’ survival by complicating factors was compared using the Chi-square test. All quantitative data are expressed as mean ± range, unless otherwise indicated. Univariate analysis of overall survival was performed using the Kaplan–Meier method.
Results
Patients
In our database of 783 CT-HDRBT treatment sessions in 520 patients between 2006 and 2009, we identified 15 patients with primary irresectable IHC. A total of 27 brachytherapy sessions were performed in these 15 patients. The male to female ratio was 1:2, mean age was 66 ± 11 years, and details about the patients and tumor characteristics are obtained in Table 1.
Median time from initial diagnosis was 7 months. Previous therapies consisted of intraarterial chemotherapy in three cases. Four patients had tumor centrally in the liver hilum.
In nine of the patients there was only one tumor present: five patients had two, and one patient had three lesions. The median size of the largest liver lesion was 5.25 (range, 1–12) cm, and the resulting median clinical target volume was 61 (mean, 89 ± 91, range, 2.1–257) ml.
Intrahepatic cholestasis was present in six cases with necessary biliary decompression in two cases. Other complicating conditions, such as (partial) portal vein occlusion, was present in five cases.
Treatment
The median number of brachytherapy catheters used per treatment session was two (range, 1–6). In four patients, initial therapy was conducted with two separate treatment sessions. Median tumor surrounding target dose was 20 Gy; in four cases the target dose had to be reduced to 15 Gy and in one case to 17 Gy because of adjacent risk structures, such as stomach or kidney, with a low tolerance for radiation. Three patients had one additional treatment for local progression during follow-up, and one patient had five reablations.
One patient developed hyperbilirubinemia of up to 51 mg/dl 6 weeks after the second brachytherapy treatment. There was no evidence for biliary obstruction, and other hepatic function tests, such as albumin, INR, and PTT, were in the normal range. The CTV of this second treatment was 68 ml with a tumor surrounding isodose of 20 Gy within 164 ml. There was no case of severe bleeding and no treatment-related death within 30 days after CT-HDRBT.
Clinical Outcome
Median follow-up was 14 months after treatment. Median local control after local ablation was 10 (range, 1–25) months; median assisted local tumor control, including repetitive local ablation, was 11 (range, 1–26) months. Currently six patients are still alive and four of them are regarded as disease-free. These four patients are currently still under local tumor control without any evidence for tumor activity.
Median time to systemic progression was 13 (range, 1–27) months. Six patients showed early tumor progression with multiple new liver lesions within the first 3 months after local ablation. These multiple lesions were impossible to be treated again by local ablation and patients received systemic therapy. In one patient with good local control and no systemic progression 6 months after treatment (8 months after initial diagnosis), a liver transplantation from a living donor was performed; 2.5 years later the patient is still free of disease.
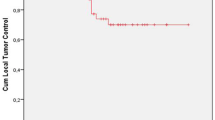
Median overall survival after primary ablation was 14 months; the mean survival was 16 ± 8.4 (range, 4–30) months. There was no significant influence on patients’ survival by a present cholestasis or portal vein thrombosis (P > 0.05). Kaplan–Meier plots of the patients’ survival are illustrated in Fig. 3.
Discussion
Intrahepatic cholangiocarcinoma (IHC) is a rare primary liver malignancy with increasing incidence worldwide. In case of local or clinical irresectability, just recently a standardized chemotherapy regimen was established, leading to a median survival of 11.7 months in a prospectively randomized trial [2, 11].
We could achieve long-lasting tumor control (up to 25 months) with no severe complication according to the SIR classification by the use of CT-HDRBT in 15 patients, which is a promising result. However, the indication for this type of therapy is given only in few patients, because most of them present with resectable tumors—locally too advanced tumors—or systemic disease, or both. This is reflected by the rather low number of 15 patients treated during the period of 4 years at our large center, which is specialized in hepatic malignancies.
Published data concerning local therapy options in intrahepatic cholangiocarcinomas (IHC) are very limited. Using external beam radiation of hilar cholangiocarcinoma and interstitial brachytherapy for extrahepatic cholangiocarcinoma, reported median survival was 9–14 months [20–22]. Photodynamic therapy also has been used in ductal cholangiocarcinoma, as a part of palliative care [23]. These results cannot be easily compared to our results, because external cholangiocarcinoma have different histology compared with IHC and typically become obvious at an earlier stage by biliary obstruction and resulting jaundice. Other reports also investigated local radiation therapy, but this was performed intraoperatively or intraluminally to improve stent patency after biliary stenting [24, 25]. Intra-arterial chemotherapy (hepatic arterial infusion; HAI) also seems to be a promising technique leading to median patients’ survival of up to 13.2 months [26, 27]. In a recently published, small study that investigated six patients treated by a combination of transarterial embolization and radiofrequency ablation, the median survival was 20 months [13]. In this study and the first study using RFA by Chiou et al., large tumor masses >5 cm resulted in residual masses and were found to be difficult to ablate completely [28]. Also typical limitations, such as central localization with the risk of heat loss due to extensive vascularity in the hepatic hilum, were found. Radiofrequency ablation has been used to treat hilar cholangiocarcinoma with biliary obstruction, and the reported mean survival was 18 month in 11 patients. Yamamoto et al. reported about the combination of liver surgery and radiofrequency ablation (12 liver resections, 8 radiofrequency ablations) in 13 patients with hepatic recurrence of IHC [29]. The reported median survival was 51 months, with a maximum survival of up to 155 months. Radioembolization has been used in a cohort of 24 patients with a planned target dose of 120 Gy inside the tumor. The reported median survival was 14.9 months [30].
Transarterial chemoembolization also has been investigated as palliative treatment of IHC with protocols using lipiodol and mitomycin C, doxorubicin-eluting beads, or oxaliplatin-eluting microspheres, which reported median survival between 13 and 30 months [31–33].
Recently an epidemiologic database study about radiation and brachytherapy of cholangiocarcinomas was published, and a median survival of 11 months using brachytherapy compared with 4 months without radiation was found [34]. Due to the inhomogeneity of the epidemiologic database patient collective and the lack of information about the technical approach, these data are not easily to compare with our data. Typically brachytherapy is performed intraluminally via the bile duct or via a percutaneous transhepatic cholangio drainage (PTCD) route, whereas our brachytherapy catheters are applied in the center of the tumor under CT-fluoroscopy guidance.
Our results suggest that CT-HDRBT may lead to prolonged survival in patients with irresectable IHC. The main advantage of CT-HDRBT is its ability to treat large tumor masses, because they often are present in patients with symptomatic IHC at diagnosis. In our series, we had three patients with immured hepatic veins, which we were able control locally. Any thermal ablation method would fail at this point by the cooling effect of the adjacent vessels. By the accurate 3D planning of the CTV in CT datasets, we gain security to cover the whole tumor volume and reduce radiation exposure to neighboring organs and structures. We had no severe complication, but the significance of this is limited due to size of the study population.
The patients tolerated the treatment well and were in general released 48 h after treatment. Due to its local character, CT-HDRBT did not show systemic side effects as they often are found in chemotherapy regimens using 5-FU.
From our point of view, CT-HDRBT might become an important part of a multimodal concept for patients with irresectable IHC. It is able to treat patients who are not suitable for local thermal destruction but with limited disease to the liver and might prolong intervals before or between oncologic chemotherapies. It might even be combined with other therapy regimes, such as intra-arterial chemotherapy, but these considerations were not part of our study.
CT-HDRBT fails in some cases, such as in our study group; six cases had multiple metastases in the remaining liver shortly after the intervention or extrahepatic tumor growth with lymph nodes metastases, peritoneal carcinomatosis with resulting ascites, which of course could not be stopped due to the local character of tumor ablation without systemic effect.
Conclusions
With the very limited therapeutic options in patients with irresectable IHC, CT-HDRBT might develop into an important gap-filler between surgical and systemic treatment, at least in those patients who are not suitable to undergo RFA but still present with limited disease to prolong chemotherapy-free intervals, local control, survival, or even treat with curative intent. This, however, necessitates further studies with larger patient numbers, if possible in a prospective, controlled setting.
References
Olnes MJ, Erlich R (2004) A review and update on cholangiocarcinoma. Oncology 66:167–179
Shaib Y, El-Serag HB (2004) The epidemiology of cholangiocarcinoma. Semin Liver Dis 24:115–125
Jarnagin WR, Shoup M (2004) Surgical management of cholangiocarcinoma. Semin Liver Dis 24:189–199
Jarnagin WR, Fong Y, DeMatteo RP et al. (2001) Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg 234:507–517; discussion 517–519
Shimada K, Sano T, Sakamoto Y et al (2007) Surgical outcomes of the mass-forming plus periductal infiltrating types of intrahepatic cholangiocarcinoma: a comparative study with the typical mass-forming type of intrahepatic cholangiocarcinoma. World J Surg 31:2016–2022
Jonas S, Thelen A, Benckert C et al (2009) Extended liver resection for intrahepatic cholangiocarcinoma: a comparison of the prognostic accuracy of the fifth and sixth editions of the TNM classification. Ann Surg 249:303–309
Lieser MJ, Barry MK, Rowland C et al (1998) Surgical management of intrahepatic cholangiocarcinoma: a 31-year experience. J Hepatobiliary Pancreat Surg 5:41–47
Hammill CW, Wong LL (2008) Intrahepatic cholangiocarcinoma: a malignancy of increasing importance. J Am Coll Surg 207:594–603
Chu KM, Lai EC, Al-Hadeedi S et al. (1997) Intrahepatic cholangiocarcinoma. World J Surg 21:301–305; discussion 305–306
Endo I, Gonen M, Yopp AC et al (2008) Intrahepatic cholangiocarcinoma: rising frequency, improved survival, and determinants of outcome after resection. Ann Surg 248:84–96
Valle J, Wasan H, Palmer DH et al (2010) Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med 362:1273–1281
Guglielmi A, Ruzzenente A, Valdegamberi A et al (2008) Radiofrequency ablation versus surgical resection for the treatment of hepatocellular carcinoma in cirrhosis. J Gastrointest Surg 12:192–198
Carrafiello G, Lagana D, Cotta E et al (2010) Radiofrequency ablation of intrahepatic cholangiocarcinoma: preliminary experience. Cardiovasc Intervent Radiol 33:835–839
Vogl TJ, Straub R, Eichler K et al (2002) Malignant liver tumors treated with MR imaging-guided laser-induced thermotherapy: experience with complications in 899 patients (2,520 lesions). Radiology 225:367–377
Mantero S, Longo I, Fiore GB et al (2003) Hyperthermia in the treatment of cholangiocarcinoma: development and testing of an endobiliary microwave device. Cardiovasc Intervent Radiol 26:379–385
Bi AH, Zeng ZC, Ji Y et al (2010) Impact factors for microinvasion in intrahepatic cholangiocarcinoma: a possible system for defining clinical target volume. Int J Radiat Oncol Biol Phys 78:1427–1436
Ricke J, Mohnike K, Pech M et al (2010) Local response and impact on survival after local ablation of liver metastases from colorectal carcinoma by computed tomography-guided high-dose-rate brachytherapy. Int J Radiat Oncol Biol Phys 78:479–485
Mohnike K, Wieners G, Schwartz F et al (2010) Computed tomography-guided high-dose-rate brachytherapy in hepatocellular carcinoma: safety, efficacy, and effect on survival. Int J Radiat Oncol Biol Phys 78:172–179
Ricke J, Wust P, Wieners G et al (2004) Liver malignancies: CT-guided interstitial brachytherapy in patients with unfavorable lesions for thermal ablation. J Vasc Interv Radiol 15:1279–1286
Ishii H, Furuse J, Nagase M et al (2004) Relief of jaundice by external beam radiotherapy and intraluminal brachytherapy in patients with extrahepatic cholangiocarcinoma: results without stenting. Hepatogastroenterology 51:954–957
Golfieri R, Giampalma E, Renzulli M et al (2006) Unresectable hilar cholangiocarcinoma: multimodality approach with percutaneous treatment associated with radiotherapy and chemotherapy. In Vivo 20:757–760
Takamura A, Saito H, Kamada T et al (2003) Intraluminal low-dose-rate 192Ir brachytherapy combined with external beam radiotherapy and biliary stenting for unresectable extrahepatic bile duct carcinoma. Int J Radiat Oncol Biol Phys 57:1357–1365
Allison RR, Zervos E, Sibata CH (2009) Cholangiocarcinoma: an emerging indication for photodynamic therapy. Photodiagnosis Photodyn Ther 6:84–92
Shin HS, Seong J, Kim WC et al (2003) Combination of external beam irradiation and high-dose-rate intraluminal brachytherapy for inoperable carcinoma of the extrahepatic bile ducts. Int J Radiat Oncol Biol Phys 57:105–112
Qian XJ, Zhai RY, Dai DK et al (2006) Treatment of malignant biliary obstruction by combined percutaneous transhepatic biliary drainage with local tumor treatment. World J Gastroenterol 12:331–335
Cantore M, Mambrini A, Fiorentini G et al (2005) Phase II study of hepatic intraarterial epirubicin and cisplatin, with systemic 5-fluorouracil in patients with unresectable biliary tract tumors. Cancer 103:1402–1407
Hong K, Geschwind JF (2010) Locoregional intra-arterial therapies for unresectable intrahepatic cholangiocarcinoma. Semin Oncol 37:110–117
Chiou YY, Hwang JI, Chou YH et al (2005) Percutaneous ultrasound-guided radiofrequency ablation of intrahepatic cholangiocarcinoma. Kaohsiung J Med Sci 21:304–309
Yamamoto M, Takasaki K, Otsubo T et al (2001) Recurrence after surgical resection of intrahepatic cholangiocarcinoma. J Hepatobiliary Pancreat Surg 8:154–157
Ibrahim SM, Mulcahy MF, Lewandowski RJ et al (2008) Treatment of unresectable cholangiocarcinoma using yttrium-90 microspheres: results from a pilot study. Cancer 113:2119–2128
Herber S, Otto G, Schneider J et al (2007) Transarterial chemoembolization (TACE) for inoperable intrahepatic cholangiocarcinoma. Cardiovasc Intervent Radiol 30:1156–1165
Aliberti C, Benea G, Tilli M et al (2008) Chemoembolization (TACE) of unresectable intrahepatic cholangiocarcinoma with slow-release doxorubicin-eluting beads: preliminary results. Cardiovasc Intervent Radiol 31:883–888
Poggi G, Amatu A, Montagna B et al (2009) OEM-TACE: a new therapeutic approach in unresectable intrahepatic cholangiocarcinoma. Cardiovasc Intervent Radiol 32:1187–1192
Shinohara ET, Guo M, Mitra N et al (2010) Brachytherapy in the treatment of cholangiocarcinoma. Int J Radiat Oncol Biol Phys 78:722–728
Conflict of interests
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schnapauff, D., Denecke, T., Grieser, C. et al. Computed Tomography-Guided Interstitial HDR Brachytherapy (CT-HDRBT) of the Liver in Patients with Irresectable Intrahepatic Cholangiocarcinoma. Cardiovasc Intervent Radiol 35, 581–587 (2012). https://doi.org/10.1007/s00270-011-0249-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-011-0249-0