Abstract
Background and Aims
Percutaneous radiofrequency ablation (RFA) demonstrated good results for the treatment of hepatocellular carcinoma (HCC) in cirrhotic patients; it is still not clear whether the overall survival and disease-free survival after RFA are comparable with surgical resection. The aims of this study are to compare the overall survival and disease-free survival in two groups of cirrhotic patients with HCC submitted to surgery or RFA.
Methods
Two hundred cirrhotic patients with HCCs smaller than 6 cm were included in this retrospective study: 109 underwent RFA and 91 underwent surgical resection at a single Division of Surgery of University of Verona.
Results
Median follow-up time was 27 months. Overall survival was significantly longer in the resection group in comparison with the RFA group with a median survival of 57 and 28 months, respectively (P = 0.01). In Child–Pugh class B patients and in patients with multiple HCC, survival was not significantly different between the two groups. In patients with HCC smaller than 3 cm, the overall survival and disease-free survival for RFA and resection were not significantly different in univariate and multivariate analysis. Whereas in patients with HCC greater than 3 cm, surgery showed improvement in outcome in both univariate and multivariate analysis.
Conclusions
Surgical resection significantly improves the overall survival and disease-free survival in comparison with RFA. In a selected group of patients (Child–Pugh class B, multiple HCC, or in HCC ≤3 cm), the results between the two treatments did not show significant differences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the most frequent primary liver neoplasm, and its incidence is increasing worldwide.1 Because of the underlying cirrhosis, the treatment of this malignancy requires a multimodality approach: although surgical resection has the best results in terms of overall survival and disease-free survival, other treatments demonstrated to be successful in improving survival.2
Percutaneous ethanol injection (PEI) and percutaneous radiofrequency ablation (RFA) proved their efficacy and safety in patients with small HCC not eligible for surgery.3 RFA has shown a greater effectiveness than PEI in obtaining complete tumor necrosis with fewer number of treatments.4 More recently, RFA has been also successfully offered in patients eligible for liver resection or transplantation.5,6 Few studies in literature evaluate the outcomes of percutaneous treatments in comparison with surgical treatment.7–9
The aim of this study is to compare the prognosis of cirrhotic patients with HCC who were submitted to surgical resection or RFA.
Material and Methods
From January 1996 to August 2006, 260 patients with chronic liver disease and HCC were submitted to liver resection or RFA at a single Division of Surgery of the Department of Surgery and Gastroenterology of the University of Verona, Italy. Two hundred patients with single or multiple (≤3 nodules) HCC measuring ≤6 cm were included in this retrospective study.
Diagnosis of HCC was based on accordance two imaging techniques (US, CT, or MRI) showing an arterial enhancement in a focal lesion ≥2 cm or with a combined criteria of an imaging technique and serum alpha-fetoprotein (AFP) level greater than 400 ng/dl, according to the European Association for Study of the Liver (EASL) consensus conference criteria. A fine-needle biopsy was performed in patients with uncertain diagnosis.10
Before surgery or RFA, all patients were submitted to complete liver function tests (bilirubin, alkaline phosphatase, AST, ALT, GGT, albumin, prothrombin time), blood count, creatinine level, chest x-rays, liver ultrasound, and abdominal triple phase computed tomography (CT) and/or contrast-enhanced magnetic resonance (MR).
Resection Group
During the study period, 91 patients were submitted to surgical resection of HCC. The characteristics of the patients submitted to surgery are reported in Table 1.
Surgical resection was considered the treatment of choice for patients with Child–Pugh class A cirrhosis and single HCC. Resection was also performed in selected patients with multiple HCC or with Child–Pugh class B cirrhosis. All surgical resections had negative resection margins confirmed with histology. Surgical specimen examination confirmed the presence of liver fibrosis in all patients. The type of resection included 28 wedge resections, 51 segmentectomies, 8 bisegmentectomies, and 2 major resections (≥3 segments).
RFA Group
During the study period, 109 patients submitted to RFA were included in this study. The characteristics of the patients submitted to RFA are reported in Table 1.
Percutaneous RFA was considered the treatment of choice for patients with Child–Pugh class B cirrhosis or with multiple tumors. A small number of patients with Child–Pugh class A cirrhosis and single tumor was treated with RFA. In these patients, ablative therapy was indicated because tumors were ill-located requiring major hepatic resection or refusal of surgery. All patients included in the study did not have general contraindication to surgery.
All the patients underwent RFA with a percutaneous approach under real-time ultrasonographic guidance in an operative room setting under conscious sedation or general anesthesia. An expandable, electrode-needle type probe, connected to a radiofrequencies generator (RITA Medical System, CA, USA) was utilized in all patients. In the first period from 1998 to 2000, we utilized a four-hook electrode-needle connected to a 50-Watt radiofrequency generator (RITA model 500, RITA Medical System, CA, USA). After 2000, a new model, expansible nine-hook needle linked to a 150-Watt generator was utilized (RITA model 1500, RITA Medical System, CA, USA).
Evaluation of treatment response was performed with CT or MR after 30 days. Evaluation of tumor response after RFA was based on the World Health Organization (WHO) criteria in which complete tumor response is defined as the absence of arterial enhancement within or at the periphery of all treated tumors determined by imaging observation (CT or MRI).11 HCC with incomplete response were reevaluated for a new RFA session.
Post Treatment Follow-up
Patients were monitored for recurrences every 3 months by physical examination, serum AFP level and imaging studies (CT or MR) were performed every 6 months. All patients with intrahepatic recurrence were evaluated for new treatment with ablative therapies (PEI or RFA), transarterial chemoembolization, or surgery in relation to the severity of liver dysfunction and tumor stage.
Statistical Analysis
All data were collected and analyzed with a statistical computer software (SPSS 14.0, SPSS, IL, USA). Categorical variables were compared using the chi-square test and continuous variables using the Student’s t test. Overall survival and disease-free survival analyses were carried out using the Kaplan–Meier methods; comparisons between different groups were carried out using the log rank test.
Multivariate analyses for survival and disease free survival were carried out using the Cox’s regression model.
Results
Resection Group
No operative mortality was observed in the patients included in this group; 33 (36.2%) patients suffered from postoperative complications. The mean follow-up for patients submitted to resection was 32 months (range 3–120 months).
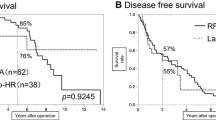
Median survival time was 57 months (95%CI = 36–77 months) with a 3-year and 5-year survival rate of 64% and 48%, respectively.
Median disease-free survival was 36 months (95%CI = 27–44 months) with a 3-year and 5-year disease-free survival rate of 56% and 27%, respectively.
RFA Group
There were no mortality after the procedure, and 11 (10%) patients suffered of minor complications. The mean follow-up in the RFA group was 23 months (range 3–92 months).
After single or multiple treatment (range 1–4 RFA sessions), complete necrosis of the tumor was obtained in 89 patients, the rate of complete necrosis was related to HCC size, 93.3% in patients with tumors ≤3 cm and 80.3% in patients with tumors larger than 3 cm (P = 0.05).
Median survival was 28 months (95%CI = 24–32 months) with 3-year and 5-year survival rate of 42% and 20%, respectively.
Median disease-free survival for the RFA group was 16 months (95%CI = 11–20) with a 3-year and 5-year disease-free survival rate of 22% and 22%, respectively.
Comparison Between the Two Groups
Overall survival was significantly longer in the resection group in comparison with the RFA group (P = 0.001) (Table 2). In Child–Pugh class A patients, surgery showed better results with a median survival of 64 months in comparison to 33 months in the RFA group (P = 0.01). Survival for patients with Child–Pugh class A cirrhosis and single HCC was significantly longer in the resection group in comparison to the RFA group with a median survival of 65 and 38 months, respectively (P = 0.05). In patients with multiple HCCs or Child–Pugh class B cirrhosis, we did not observe differences in survival between the two groups. (Table 2).
Multivariate analysis identified that Child–Pugh class B, AFP level grater than 20 ng/dl, and RFA treatment were significantly related with survival, the relative hazards were 2.1, 2.7, and 3.2, respectively (Table 3).
Comparison Between the Two Groups in HCCs ≤3 cm
Survival analysis in patients with tumors ≤3 cm identified that survival was longer in patients in the resection group in comparison to the RFA group with a median survival time of 65 and 37 months, respectively; the difference did not reach statistical significance. Subgroup survival analyses of patients with single or multiple HCC in Child–Pugh A and B patients did not show significantly different survival rates between the two groups (Table 2). Multivariate analysis in patients with HCC ≤3 cm identified that only Child–Pugh class was significantly related with survival (Table 3).
Comparison Between the Two Groups in HCCs >3 cm
In patients with tumors greater than 3 cm, the overall survival was significantly longer in the resection group with a median survival of 40 months compared to 24 months for the RFA group (P = 0.01; Table 2). Survival for patients with HCC larger than 3 cm and Child–Pugh class A cirrhosis was significantly longer in the resection group compared with the RFA group with a median survival time of 64 and 27 months, respectively (P = 0.05). Subgroup analysis in patients with Child–Pugh class A cirrhosis and single HCC confirmed longer median survival time for the resection group but the difference did not reach statistical significance (Table 2). Whereas surgical resection did not show superior results compared to the RFA group in Child–Pugh class B patients or in multiple HCC. Multivariate analysis in patients with HCC greater than 3 cm identified that Child-Pugh class B, serum AFP level grater than 20 ng/dl, and RFA were significantly related with worse prognosis with relative hazards of 1.7, 2.6, and 2.6, respectively (Table 3).
Disease-free Survival
Disease-free survival for the resection group was significantly longer in comparison to the RFA group with a median recurrence-free time of 36 and 16 months, respectively (P = 0.001).
Disease free survival analysis in patients with tumors ≤3 cm showed similar results between the two groups with 5-year disease-free survival of 36% in the RFA group and 19% in the resection group (P = 0.70; Table 4). Multivariate analysis confirms that the type of treatment was not significantly related with recurrence (Table 5).
In patients with HCCs >3 cm, median disease-free survival was significantly longer in the resection group compared with the RFA group, 36 and 12 months respectively (P = 0.001; Table 4). Multivariate analysis for HCCs grater than 3 cm identified that RFA treatment and multiple tumors were significantly related with higher recurrence rate with relative hazards of 2.5 and 2.1, respectively (Table 5).
Discussion
The management of hepatocellular carcinoma on cirrhosis involves nowadays many treatment options in relation to the tumor stage and the severity of underlying chronic liver disease.10,12,13 Among these, liver transplantation has the best results in terms of overall survival and disease-free survival, but only few patients can be submitted to this treatment because of organ shortage.14,15
Liver surgery for hepatocellular carcinoma has improved its results in patients with and without chronic liver disease during the last decades with mortality lower than 5% in most series.6,16 Long-term outcome after surgery is good with a 5-year survival rate of 50%, but recurrence of the disease is still a major issue with more than 70% of patients who suffer recurrent disease.17
Local ablative techniques, in particular RFA, gained much consent in the last years for its low complications rate and for its efficacy in local necrosis of the tumor.3,18 The indications for these treatments, the real impact in HCC natural history, and the long-term survival are still matter of debate. Moreover, RFA has been successfully applied in the setting of liver transplantation as a bridge procedure to control the tumor progression during the waiting list period.15
Recent studies in literature compared local ablative therapies with surgical resection. In a previous retrospective multicenter study, the authors identified that surgical resection has still the best results in terms of overall survival and disease-free survival.7 On the contrary Wakai et al., in a retrospective study in HCCs smaller than 4 cm, identified that results of local ablative therapy are comparable with surgery in HCCs smaller than 2 cm with a 10-year actuarial survival rate of 45% for ablative therapy and 58% for surgical resection (P = 0.08), whereas surgery showed superior results in larger HCCs.9 More recently, Hong et al. found that RFA is as effective as surgery in small HCC (≤4 cm), also with preserved liver function (Child–Pugh class A) without differences in overall survival and disease-free survival.8
In literature, only one prospective randomized trial had been recently published. In this study, the authors identified that surgery and RFA have similar results for single HCCs smaller than 5 cm in terms of overall survival and disease-free survival.19
The results of the current study confirm that surgery has still superior results in comparison to RFA and that these differences are more clearly demonstrated in HCCs larger than 3 cm. The current study has some limitations because it is retrospective with a relatively small sample and because the two groups of patients have differences in severity of chronic liver disease and in tumor stage. However, we think that these biases did not influence the statistical analysis in the subgroups and in the multivariate analyses.
In the current study, we included in the analysis only patients submitted to surgical or ablative treatment with curative intent because the strong prognostic value of complete response of treatment both in surgical therapies and in RFA has been clearly demonstrated.20,21 With regard to tumor size, we choose the 3-cm cutoff value because RFA showed higher tumor necrosis rate in HCCs smaller than 3 cm.18
In tumor smaller than 3 cm, we observed a longer median survival time for patients submitted to surgical resection, 65 vs 37 months, respectively, but the difference did not reach statistical significance (P = 0.12). Also, multivariate analysis showed that type of treatment did not influence the survival in this group of patients.
Although these data emphasized the efficacy of RFA in small HCCs, surgical resection still has better results also in small HCCs. The role of RFA in these patients should be evaluated in relation with the severity of chronic liver disease where the lower risk of the procedure without impairment of liver function could give some advantages in these patients. Moreover, RFA could be preferred to surgical resection in patients candidate for liver transplantation.
Surgical resection proved its efficacy in HCCs larger than 3 cm in which hepatectomy can remove small peritumoral satellites and microvascular invasion that are frequently observed in larger tumors.22 In these patients, the results of surgery was clearly superior to RFA in both univariate and multivariate analyses.
In conclusion, this retrospective study shows that RFA have comparable results with surgical resection in patients with more severe liver dysfunction (Child–Pugh class B) or multiple nodules. In single small HCCs (≤3 cm), surgery has still better results but the difference with RFA did not reach statistical significance in univariate and multivariate analysis.
In larger HCCs (>3 cm and <6 cm), surgical resection has still demonstrated its efficacy in terms of long-term survival and disease-free survival. More studies are necessary to demonstrate if RFA can be a curative therapeutic option in patients candidate for surgical resection for HCCs smaller than 3 cm.
References
Bosch FX, Ribes J, Cleries R, Diaz M. Epidemiology of hepatocellular carcinoma. Clin Liver Dis 2005;9(2):191–211.
Carr B. Hepatocellular carcinoma: current management and future trends. Gastroenterology 2004;127(5 Suppl 1):S218–S224.
Poon RT, Fan ST, Tsang FH, Wong. Locoregional therapies for hepatocellular carcinoma: a critical review from the surgeon’s perspective. Ann Surg 2002;235(4):466–486.
Sutherland LM, Williams JA, Padbury RT, Gotley DC, Stokes B, Maddern GJ. Radiofrequency ablation of liver tumors: a systematic review. Arch Surg 2006;141(2):181–190.
Ng KKC, Lam CM, Poon RT, et al. Thermal ablative therapy for malignant liver tumors: a critical appraisal. J Gastroenterol Hepatol 2003;18:616–629.
Curley S. Radiofrequency ablation of malignant liver tumors. Ann Surg Oncol 2003;10:338–347.
Vivarelli M, Guglielmi A, Ruzzenente A, Cucchetti A, Bellusci R, Cordiano C, Cavallari A. Surgical resection versus percutaneous radiofrequency ablation in the treatment of hepatocellular carcinoma on cirrhotic liver. Ann Surg 2004;240(1):102–107.
Hong SN, Lee SY, Choi MS, Lee JH, Koh KC, Paik SW, Yoo BC, Rhee JC, Choi D, Lim HK, Lee KW, Joh JW. Comparing the outcomes of radiofrequency ablation and surgery in patients with a single small hepatocellular carcinoma and well-preserved hepatic function. J Clin Gastroenterol 2005;39(3):247–252.
Wakai T, Shirai Y, Suda T, Yokoyama N, Sakata J, Cruz P, Kawai H, Matsuda Y, Watanabe M, Aoyagi Y, Hatakeyama K. Long-term outcomes of hepatectomy vs percutaneous ablation for treatment of hepatocellular carcinoma < or =4 cm. World J Gastroenterol 2006;12(4):546–552.
Bruix J, Sherman M, Llovet JM, et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol 2001;35:421–430.
Miller AB, Hoogstraten B, Staquet M, Winkler A. Reporting results of cancer treatment. Cancer 1981;47:207–214.
El-Serag HB, Mallat DB, Rabeneck L. Management of the single liver nodule in a cirrhotic patient: a decision analysis model. J Gastroenterol 2005;39(2):152–159.
Taura K, Ikai I, Hatano E, Fujii H, Uyama N, Shimahara Y. Implication of frequent local ablation therapy for intrahepatic recurrence in prolonged survival of patients with hepatocellular carcinoma undergoing hepatic resection: an analysis of 610 patients over 16 years old. Ann Surg 2006;244(2):265–273.
Hashikura Y, Kawasaki S, Terada M, et al. Long-term results of living-related donor liver graft transplantation: a single center analysis of 110 patients. Transplantation 2001;72:95–99.
Mazzaferro V, Battiston C, Perrone S, Pulvirenti A, Regalia E, Romito R, Sarli D, Schiavo M, Garbagnati F, Marchiano A, Spreafico C, Camerini T, Mariani L, Miceli R, Andreola S. Radiofrequency ablation of small hepatocellular carcinoma in cirrhotic patients awaiting liver transplantation: a prospective study. Ann Surg 2004;240(5):900–909.
Grazi GL, Ercolani G, Pierangeli F, Del Gaudio M, Cescon M, Cavallari A, Mazziotti A. Improved results of liver resection for hepatocellular carcinoma on cirrhosis give the procedure added value. Ann Surg 2001;234(1):71–78.
Poon RT, Fan ST, Lo CM, Liu CL, Lam CM, Yuen WK, Yeung C, Wong J. Extended hepatic resection for hepatocellular carcinoma in patients with cirrhosis: is it justified? Ann Surg 2002;236(5):602–611.
Guglielmi A, Ruzzenente A, Battocchia A, Tonon A, Fracastoro G, Cordiano C. Radiofrequency ablation of hepatocellular carcinoma in cirrhotic patients. Hepatogastroenterology 2003;50:480–484.
Chen MS, et al. A prospective randomized trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma. Ann Surg 2006;243(3):321–328.
Sala M, Llovet JM, Vilana R, et al. Initial response to percutaneous ablation predicts survival in patients with hepatocellular carcinoma. Hepatology 2004;40(6):1352–1360.
Guglielmi A, Ruzzenente A, Sandri M, Pachera S, Pedrazzani C, Tasselli S, Iacono C. Radiofrequency ablation for HCC in cirrhotic patients: prognostic factors for survival. J Gastrointest Surg 2007;11(2):143–149, Feb.
Toyosaka A, Okamoto E, Mitsunobu M, Oriyama T, Nakao N, Miura K. Intrahepatic metastases in hepatocellular carcinoma: evidence for spread via the portal vein as efferent vessel. Am J Gastroenterol 1996;91(8):1610–1615.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guglielmi, A., Ruzzenente, A., Valdegamberi, A. et al. Radiofrequency Ablation Versus Surgical Resection for the Treatment of Hepatocellular Carcinoma in Cirrhosis. J Gastrointest Surg 12, 192–198 (2008). https://doi.org/10.1007/s11605-007-0392-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-007-0392-8