Abstract
Purpose
To evaluate the safety and efficacy of transjugular intrahepatic portosystemic shunt (TIPS) in the control of bleeding from ectopic varices.
Methods
From 1995 to 2004, 24 cirrhotic patients, bleeding from ectopic varices, mean age 54.5 years (range 15–76 years), were treated by TIPS. The etiology of cirrhosis was alcoholic in 13 patients and nonalcoholic in 11 patients. The location of the varices was duodenal (n = 5), stomal (n = 8), ileocolic (n = 6), anorectal (n = 3), umbilical (n = 1), and peritoneal (n = 1).
Results
TIPS controlled the bleeding in all patients and induced a decrease in the portacaval gradient from 19.7 ± 5.4 to 6.4 ± 3.1 mmHg. Postoperative complications included self-limited intra-abdominal bleeding (n = 2), self-limited hemobilia (n = 1), acute thrombosis of the shunt (n = 1), and bile leak treated by a covered stent (n = 1). Median follow-up was 592 days (range 28–2482 days). Rebleeding occurred in 6 patients. In 2 cases rebleeding was observed despite a post-TIPS portacaval gradient lower than 12 mmHg and was controlled by variceal embolization; 1 patient underwent surgical portacaval shunt and never rebled; in 3 patients rebleeding was related to TIPS stenosis and treated with shunt dilatation with addition of a new stent. The cumulative rate of rebleeding was 23% and 31% at 1 and 2 years, respectively. One- and 2-year survival rates were 80% and 76%, respectively.
Conclusion
The present series demonstrates that bleeding from ectopic varices, a challenging clinical problem, can be managed safely by TIPS placement with low rebleeding and good survival rates.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Variceal hemorrhage is a frequent complication of portal hypertension. Esophageal and gastric varices are the most common cause of gastrointestinal bleeding. However, ectopic varices may develop anywhere in the abdomen except in the cardioesophageal junction (small intestine, colon, rectum, peritoneum, umbilicus) and represent an unusual cause of hemorrhage, accounting for up to 5% of all variceal bleeding [1]. Management of bleeding from ectopic varices is challenging because high rebleeding rates are observed following local treatment of varices and portacaval shunt surgery is associated with a high postoperative morbidity and mortality.
Nonsurgical transjugular intrahepatic portosystemic shunt (TIPS) represents a significant advance because it relieves portal hypertension and is much less invasive than portacaval shunt surgery [2].
The aim of this study was to evaluate the efficacy of TIPS on the control of bleeding from ectopic varices in cirrhotic patients.
Materials and Methods
Patients
From 1995 to 2004, 24 cirrhotic patients were evaluated for bleeding from ectopic varices. The population consisted of 19 males and 5 females with a mean age of 54.5 years (range 15–76 years). The cause of portal hypertension was as follows: alcoholic cirrhosis (13 patients), chronic hepatitis B (1 patient), autoimmune hepatitis (1 patient), sclerosing cholangitis (2 patients), secondary biliary cirrhosis (1 patient), sarcoidosis (1 patient), and cryptogenic cirrhosis (5 patients). On admission, 10 patients had ascites and 2 patients developed bleeding-induced hepatic encephalopathy.
According to the Child-Pugh classification, 5 patients were class A, 12 patients were class B, and 7 patients were class C. The mean Pugh score was 8.1 (median 8; range 5–11). The mean serum albumin was 24.7 g/L (range 15–40 g/L), the mean serum bilirubin was 40 μmol/L (range 16–116 μmol/L) and the mean INR was 1.69 (range 1.1–5.7). The mean MELD score was 13.8 (median 13.3; range 5.5–34.5).
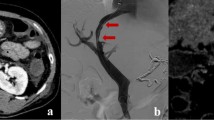
The site of bleeding was diagnosed by endoscopy and/or CT scan and visualized by portography during the TIPS procedure. The varices were duodenal (n = 5), ileocolic (n = 6), anorectal (n = 3), stomal (n = 8), umbilical (n = 1), and peritoneal (n = 1).
TIPS Procedure
The TIPS procedure was performed under neuroleptanalgesia as reported previously [3]. The portal vein was catheterized using a transjugular approach; the tract between the hepatic vein and the intrahepatic portal vein was dilated using a balloon angioplasty catheter and the shunt was created using Memotherm or Luminex stents (Angiomed, Karlsruhe, Germany). The portacaval gradient was measured before and after TIPS placement. The stent was dilated to 10 mm or 12 mm depending on the results, aiming at a gradient less than 12 mmHg, a threshold value commonly associated with the risk of variceal rebleeding [4], and absence of visualization of ectopic varices. Antibioprophylaxis was given for 24 hr and anticoagulation was never used.
Follow-up
All the patients were followed at a specialized outpatient clinic. The presence and severity of ascites or encephalopathy was recorded. Encephalopathy was classified as mild (isolated episodes with a well-identified precipitating factor), moderate (recurrent episodes easily managed by diet and/or medication) or severe (not controlled by medical therapy and requiring hospitalization). Routine biochemical tests including liver enzymes, albumin, and coagulation parameters were measured. The patency of the shunt was assessed with duplex Doppler ultrasonography according to a standardized protocol 1–3 days after TIPS, every 3 months during the first year, and every 6 months thereafter [5]. If rebleeding occurred or if Doppler ultrasound suggested shunt dysfunction [5], the shunt was catheterized and the portohepatic gradient was measured. When the gradient was higher than 12 mmHg, dilatation of the shunt was performed and a new stent was placed if needed; embolization of varices with coils was performed when rebleeding occurred despite a portacaval gradient lower than 12 mmHg. The follow-up was ended on December 1, 2004. Median follow-up was 592 days (range 28–2482 days).
Statistical Analysis
Results are expressed as mean ± SD. The cumulative rates of shunt patency, rebleeding, and survival were calculated by using the Kaplan-Meier method.
Results
TIPS Procedure
The TIPS procedure was performed successfully in all patients. Hemodynamic measurements demonstrated that the pre-TIPS portacaval gradient decreased from 19.7 ± 5.4 mmHg to 6.4 ± 3.1 mmHg following the procedure. The post-TIPS gradient was lower than 12 mmHg in all patients.
Early post-TIPS complications occurred in 4 patients: 2 had self-limited intra-abdominal bleeding, 1 had a self-limited hemobilia, and 1 developed a bile leak successfully treated with a covered stent.
Shunt Patency
The cumulative shunt dysfunction rate (defined as a portacaval gradient higher than 12 mmHg) was of 51% (95% confidence interval (CI): 27–85%) at 12 months (Fig. 1). Twenty-one episodes of dysfunction were observed in 11 patients. Of them, 2 patients had four episodes of dysfunction, 2 patients had three episodes of dysfunction, and 7 patients had one episode of dysfunction. All episodes of dysfunction were treated by TIPS revision; 1 patient underwent surgical portacaval shunt after repeated rebleeding episodes from stomal varices despite three angiographic interventions. Shunt occlusion was observed in 2 patients, one of whom had a bile leak.
Hepatic Encephalopathy
Seven patients (29%) had mild hepatic encephalopathy after TIPS. Severe hepatic encephalopathy occurred in 2 patients (8%); it was successfully treated by shunt occlusion with a detachable balloon in 1 patient. This patient never rebled from colic varices but ascites reappeared after occlusion.
Rebleeding
One patient bled from an ulcer following sclerotherapy of rectal varices performed prior to the TIPS, and 6 patients rebled from ectopic varices. The cumulative rates of variceal rebleeding were 23% (95% CI: 6–28%) and 31% (95% CI: 9–53%) at 1 and 2 years, respectively (Fig. 2). Two patients rebled from colic varices; the gradient at rebleeding, as measured at the time of TIPS venography, was less than 12 mmHg (5 mmHg and 11 mmHg); rebleeding was successfully controlled by variceal embolization of the veins feeding the varices. Two patients rebled from stomal varices; rebleeding was controlled by shunt dilatation in one, while the other required a surgical portacaval shunt for repeated rebleeding episodes which could not be controlled by serial angiographic interventions; he never rebled thereafter. One patient rebled from colic varices 3 days after TIPS; early thrombosis of the shunt due to a biliary fistula was demonstrated and treated using a polytetrafluoroethylene (PTFE)-covered stent. One patient rebled from duodenal varices due to shunt stenosis; this was treated by shunt dilatation and placement of a new stent.
Survival
Seven patients died from different causes during follow-up: bleeding from a sclerotherapy-induced rectal ulcer (n = 1), car accident (n = 1), liver failure (n = 4), and from an unknown cause (n = 1). The cumulative survival rates were 80% (95% CI: 62–98%) and 76% (95% CI: 54–94%) at 1 and 2 years, respectively (Fig. 3).
Discussion
Ectopic varices may occur at various abdominal sites including small bowel, colon, rectum, stomas, umbilicus, retroperitoneum, biliary tract, vagina, and bladder. The prevalence of ectopic varices in patients with portal hypertension is quite high, particularly for duodenal and anorectal varices [1, 6]. However, ectopic varices are an unusual cause of gastrointestinal hemorrhage accounting for between 1% and 5% of all variceal bleeding [7, 8].
The diagnosis is challenging as endoscopic visualization is often difficult or impossible, particularly when patients bleed from ileocolic varices. In such cases, angiography, CT, and MRI are useful to localize the site of bleeding [9, 10].
In a review of 169 cases of bleeding ectopic varices, 17% occurred in the duodenum, 17% in the jejunum or ileum, 14% in the colon, 8% in the rectum, 9% in the peritoneum, 26% in stomas, and a few from infrequent sites such as the ovary and vagina [1].
Treatments of bleeding from ectopic varices include local treatment performed either endoscopically, radiologically, or surgically and portal decompressive surgery or TIPS. The efficacy of pharmacologic treatment with beta-blockers has never been evaluated. Endoscopic sclerotherapy has been tried for duodenal, anorectal, and stomal varices but, almost invariably, rebleeding occurred and ulcers following sclerotherapy may result in life-threatening hemorrhage [11, 12].
Variceal embolization after portal vein catheterization can control bleeding but rebleeding is not unusual due to the development of new collaterals feeding the ectopic varices. Surgical ligation of varices is also a temporary measure that does not allow definitive control of variceal bleeding. This is not surprising as none of these methods relieves the portal hypertension.
Portacaval shunt surgery has been used in some patients; however, the postoperative morbidity and mortality rates are high particularly in patients with decompensated liver disease. Decompressive surgery is very efficient at avoiding variceal rebleeding but it may precipitate liver failure or induce recurrent hepatic encephalopathy [13]. A surgical shunt was performed successfully in one Pugh class A patient of this series following TIPS failure.
TIPS is a hemodynamic equivalent of a side-to-side small-diameter portacaval shunt; it is much less invasive than surgery and can be performed even in patients with decompensated liver disease [2]. TIPS has been widely used for the treatment of bleeding from gastroesophageal varices as well as refractory ascites. This procedure is safe, with a 1–2% incidence of early life-threatening complications; the rate of hepatic encephalopathy is much lower than that observed after portavacal shunt surgery but shunt dysfunction due to progressive stenosis following pseudointimal hyperplasia inside the stent is a significant problem. Accordingly, shunt function must be monitored closely with duplex Doppler ultrasonography and/or shunt catheterization and angiographic interventions are frequently needed [4]. The use of stents covered with PTFE has been reported to markedly reduce the incidence of shunt stenosis and will probably represent a major advance in the future [14].
The rebleeding rate after TIPS placement was low in the present series (23% at 1 year). It has been shown previously that decreasing the portacaval gradient below a threshold value of 12 mmHg almost completely abolishes the risk of bleeding from esophageal varices; this may not hold true in patients with large gastric or ectopic varices as variceal tension, a determinant of the risk of bleeding, is influenced by the diameter of the varix. In the present series, rebleeding occurred in 2 patients with huge colic varices despite a low post-TIPS portacaval gradient. In such patients, variceal embolization can be performed in addition to the TIPS procedure [15]. The occurrence of encephalopathy was mostly controllable. Only 2 patients developed chronic disabling neurologic symptoms, and TIPS occlusion was required in one of them. The survival rate in this small population was very good, taking into account that 80% of patients were Pugh class B and C.
The role of TIPS has been assessed previously by several case reports [15–21] and by two small studies in patients with bleeding ectopic varices. Haskal et al. [22] reported that among 9 patients treated for small bowel (n = 6) and colic bleeding varices (n = 3), only 1 rebled requiring embolization and 2 died during hospitalization. In the study by Shibata et al. [23], TIPS was performed in 5 patients with parastomal varices and 7 patients with anorectal varices; none of them rebled, 2 patients died within 1 month, and 3 patients developed post-TIPS encephalopathy.
The largest series, published more recently, involved 21 cirrhotic patients with bleeding ectopic varices [24]. The authors emphasized that large ectopic varices rebled in 4 patients despite a post-TIPS portacaval gradient lower than 12 mmHg. They suggested that variceal embolization must be performed routinely at the time of TIPS placement.
Bleeding from ectopic varices is often a difficult clinical problem; CT scan and MRI have improved the diagnostic accuracy over recent years. The TIPS procedure is clearly beneficial in this setting and must be considered early to prevent rebleeding. In addition, given the high rate of TIPS dysfunction in these patients with bare stents TIPS, improved outcomes may be anticipated in the future with the use of PTFE-covered stents [14].
References
Norton ID, Andrews JC, Kamath PS (1998) Management of ectopic varices. Hepatology 28:1154–1158
Boyer TD (2003) Transjugular intrahepatic portosystemic shunt: Current status. Gastroenterology 124:1700–1710
Pomier-Layrargues G, Villeneuve JP, Deschenes M, et al. (2001) Transjugular intrahepatic portosystemic shunt (TIPS) versus endoscopic variceal ligation in the prevention of variceal rebleeding in patients with cirrhosis: A randomised trial. Gut 48:390–396
Casado M, Bosch J, Garcia-Pagan J, et al. (1998) Clinical events after transjugular intrahepatic portosystemic shunt: Correlation with hemodynamic findings. Gastroenterology 114:1296–1303
Lafortune M, Martinet JP, Denys A, et al. (1995) Short- and long-term hemodynamic effects of transjugular intrahepatic portosystemic susnts: A Doppler/manometric correlative study. AJR Am J Roentgenol 164:997–1002
Hosking SW, Smart HL, Johnson AG, et al. (1989) Anorectal varices, hemorrhoids and portal hypertension. Lancet I:349–352
Kinkhabwala M, Mousavi A, Iyer S, et al. (1977) Bleeding ileal varicosity demonstrated by transhepatic portography. AJR Am J Roentgenol 129:514–516
Khouqeer F, Morrow C, Jordan P (1987) Duodenal varices as a cause of massive upper gastrointestinal bleeding. Surgery 102:548–552
Kakizaki S, Ishikawa T, Koyama Y, et al. (2003) Primary biliary cirrhosis complicated with sigmoid colonic varices: The usefulness of computed tomographic angiography. Abdom Imaging 28:831–834
Handschin AE, Weber M, Weishaupt D, et al. (2002) Contrast-enhanced three-dimensional magnetic resonance angiography for visualization of ectopic varices. Dis Col Rectum 45:1541–1544
Kishimoto K, Hara A, Arita T, et al. (1999) Stomal varices: Treatment by percutaneous transhepatic coil embolization. Cardiovasc Intervent Radiol 22:523–525
Jonnalagadda SS, Quiason S, Smith OJ (1998) Successful therapy of bleeding duodenal varices by TIPS after failure of sclerotherapy. Am J Gastroenterol 93:272–274
Sarfeh IJ, Rypins EB (1986) The emergency portacaval H graft in alcoholic cirrhotic patients: Influence of shunt diameter on clinical outcome. Am J Surg 152:290–293
Bureau C, Garcia-Pagan JC, Otal P, et al. (2004) Improved clinical outcome using polytetrafluoroethylene coated stents for TIPS: Results of a randomized study. Gastroenterology 126:469–475
Hidajat N, Stobb H, Hosten N, et al. (2002) Transjugular intrahepatic shunt and transjugular embolization of bleeding rectal varices in portal hypertension. AJR Am J Roentgenol 178:362–363
Fantin AC, Zala G, Risti B, et al. (1996) Bleeding anorectal varices : Successful treatment with transjugular intrahepatic portosystemic shunting (TIPS). Gut 38:932–935
Morris CS, Najarian KE (2000) Transjugular intrahepatic portosystemic shunt for bleeding stomal varices associated with chronic portal vein occlusion: Long-term angiographic, hemodynamic, and clinical follow-up. Am J Gastroenterol 95:2966–2968
Bernstein D, Yrizarry J, Reddy KR, et al. (1996) Transjugular intrahepatic portosystemic shunt in the treatment of intermittently bleeding stomal varices. Am J Gastroenterol 91:2237–2238
Katz JA, Rubin RA, Cope C, et al. (1993) Recurrent bleeding from anorectal varices: Successful treatment with a transjugular intrahepatic portosystemic shunt. Am J Gastroenterol 88:1104–1107
Johnson PA, Laurin J (1997) Transjugular portosytemic shunt for treatment of bleeding stomal varices. Dig Dis Sci 42:440–442
Ory G, Spahr L, Megevand JM, et al. (2001) The long-term efficacy of the intrahepatic portosystemic shunt (for the treatment of bleeding anorectal varices in cirrhosis. A case report and review of the literature. Digestion 64:261–264
Haskal ZJ, Scott M, Rubin RA, et al. (1994) Intestinal varices: Treatment with the transjugular intrahepatic portosystemic shunt. Radiology 191:183–187
Shibata D, Brophy DP, Gordon FD, et al. (1999) Transjugular intrahepatic portosystemic shunt for treatment of bleeding ectopic varices with portal hypertension. Dis Col Rectum 42:1581–1585
Vangeli M, Patch D, Terreni N, et al. (2004) Bleeding ectopic varices treatment with transjugular intrahepatic portosystemic shunt (TIPS) and embolisation. J Hepatol 41:560–566
Acknowledgments
The authors thank Mrs. Manon Bourcier for editing the manuscript and Dr. Daphna Fenyves for reviewing the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vidal, V., Joly, L., Perreault, P. et al. Usefulness of Transjugular Intrahepatic Portosystemic Shunt in the Management of Bleeding Ectopic Varices in Cirrhotic Patients. Cardiovasc Intervent Radiol 29, 216–219 (2006). https://doi.org/10.1007/s00270-004-0346-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-004-0346-4