Abstract
Introduction
Pharmacological prophylaxis for early seizures following traumatic brain injury (TBI) is a recommendation in the Brain Trauma Foundation Guidelines. However, several studies have challenged the efficacy and safety of this practice, resulting in varied practice across centers around the world. The purpose of the present study was to compare the incidence of early clinical seizures following TBI, between two large centers, a US Center that practises routine seizure prophylaxis and a Chinese Center that does not use seizure prophylaxis following TBI.
Patients and methods
This was a prospective observational study including an urban level I trauma center in the USA and a large hospital in Shenzhen, China. At the US Center, all patients received seizure prophylaxis with levetiracetam. At the Chinese Center, no seizure prophylaxis was given. All patients with blunt TBI and positive computed tomography findings for epidural hematoma, subdural hematoma, subarachnoid hemorrhage, intracerebral hemorrhage or diffuse axonal injury were included. Patients who died within 24 h of admission were excluded. The study population was monitored daily for clinical seizures for the first 7 post-injury days. Data collected included demographics, mechanism of injury, vital signs upon arrival, injury severity and emergency interventions. Primary outcome was the incidence of early seizures, defined as those occurring within 7 days of injury.
Results
A total of 522 patients were included in the analysis: 272 patients at the US Center who received seizure prophylaxis and 250 patients at the Chinese Center who did not receive prophylaxis. Overall, 3.7% of patients who received seizure prophylaxis developed early seizures, compared to 2.8% of patients who did not receive any prophylaxis (p = 0.573). Decompressive craniectomy was associated with the highest incidence of early seizure (9.2%). In this subgroup, the seizure rate was 10.4% in the prophylaxis group and 7.1% in the no-prophylaxis group (p = 0.738). Patients with admission GCS < 9 had an overall early seizure incidence of 7.0%: 4.3% in the prophylaxis group and 14.3% in the no-prophylaxis group (p = 0.062). Analysis of the subgroup with isolated blunt TBI showed an incidence of early seizures of 3.4% in the prophylaxis group versus 2.4% in the no-prophylaxis group (p = 0.593). Further analyses of outcomes according to head AIS 3, 4 and 5 showed no significant difference in the seizure rate between the two groups: head AIS 3: 6.1% in the prophylaxis group versus 2.6% in the no-prophylaxis group, p = 0.329; head AIS 4: 0 versus 2.7%, p = 0.302; head AIS 5: 8.7 versus 4.0%, p = 0.601.
Conclusions
The present study failed to show any benefit of routine early seizure prophylaxis following blunt TBI. This practice should be reexamined in a large randomized clinical study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Early pharmacological seizure prophylaxis for traumatic brain injuries (TBI) is a common practice in most centers in the USA and is a recommendation in the Brain Trauma Foundation Guidelines [1]. This recommendation, however, is based largely on historic level II evidence [2] and has not been adopted worldwide. A randomized control study in 1990 reported that phenytoin prophylaxis reduced the incidence of early post-traumatic seizures; however, it had no benefit on late-seizure rates [2]. The utility of early seizure prophylaxis has been challenged with concern for no clinical benefit and a potential negative cognitive effect and worsened functional outcome in patients treated with prophylaxis [3,4,5,6].
The purpose of the present study was to compare the incidence of early clinical seizures following TBI, between an American trauma center, which practises routine seizure prophylaxis, and a large urban Chinese hospital, which does not use seizure prophylaxis after TBI.
Patients and methods
This was a prospective observational study at two large hospitals: the LAC + USC Medical Center, in Los Angeles, and the Nanshan Hospital, a large, urban hospital in Shenzhen, China. At LAC + USC Medical Center, all patients received seizure prophylaxis with levetiracetam (Keppra) at a dose of 500 mg every 12 h for 7 days per hospital protocol. At the Nanshan Hospital, no seizure prophylaxis was given. Institutional Review Board approval was obtained at both hospitals. The study was performed over a 19-month period (Sept 2015–April 2017). The two hospitals use different protocols in the management of traumatic brain injuries. In addition to differences in seizure prophylaxis, at the Nanshan Hospital, patients with GCS < 9 and normal SaO2 do not undergo routine endotracheal intubation in the emergency room, and ICP monitoring and decompressive craniectomies for intracranial hypertension are very rarely performed.
All patients with blunt TBI and computed tomography (CT) findings of epidural hematoma, subdural hematoma, subarachnoid hemorrhage, intracerebral hemorrhage or diffuse axonal injury were included in the study. Patients who died within 24 h of admission were excluded, because they died due to other major associated injuries or were non-survivable TBI. The study population was monitored daily for clinical seizures for the first seven post-admission days. If there was suspicion of subclinical seizures (nystagmus, facial twitching, changing anisocoria or any other suspected seizure activity), an EEG was performed.
Data collected included demographics, mechanism of injury (motor vehicle collision, auto versus pedestrian, motorcycle collision, auto versus bicycle, fall, assault and other), vital signs upon arrival to the emergency department (ED), ED intubation, craniectomy, intracranial pressure (ICP) monitor placement, injury severity score (ISS) and Abbreviated Injury Scale (AIS) of each body region (head, chest, abdomen, extremities). The Abbreviated Injury Severity (AIS) 2005 grading system was used [7]. Primary outcome was the incidence of early seizures, defined as those occurring within the first 7 days of admission. Seizures that were reported before hospital arrival or in the emergency department or occurred after post-injury day 7 were not included.
Statistical analysis
Data from both hospitals were recorded into a password-protected Microsoft Office 2013 Excel spreadsheet. Data analyses were done by the LAC + USC Medical Center using SPSS for windows version 20 (Chicago Inc, IL). Categorical variables were expressed as percentages and were compared using Pearson Chi-square test/Fisher exact test, while continuous variables were expressed as median with interquartile range (IQR) and compared using Mann–Whitney U test.
Findings
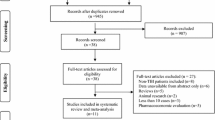
During the study period, a total 522 patients met inclusion criteria and were included in the analysis. A total of 272 patients (52.1%) were admitted to LAC + USC Medical Center and received seizure prophylaxis, and 250 patients (47.9%) were admitted to the Nanshan Hospital and did not receive any prophylaxis. The epidemiologic and clinical characteristics including interventions of the two study groups are shown in Table 1. Patients admitted to the LAC + USC Medical Center were significantly more likely to undergo endotracheal intubation in the emergency room than patients admitted to Nanshan Hospital (41.8 vs 4.8%, p < 0.001), more likely to have an ICP monitor placed (37.7 vs 3.2%, p < 0.001) and more likely to undergo craniectomy (24.9 vs 16.7% p = 0.022).
There was no difference in the incidence of early seizures between the patients treated with seizure prophylaxis at LAC + USC Medical Center and those treated without prophylaxis at the Nanshan Hospital. Overall, 10 of the 272 (3.7%) patients treated at LAC + USC Medical Center developed early seizures, while early seizures developed in 7 of the 250 (2.8%) patients at Nanshan Hospital (p = 0.573). After excluding those patients who died or transferred to other facility within 7 days of admission, the incidence of early seizures remained similar between the two groups [LAC + USC 10/250 (4.0%) vs Nanshan 7/237 (3.0%), p = 0.529].
In the 23 pediatric TBI patients treated at the two hospitals, there were no clinical seizures recorded. Decompressive craniectomy was associated with the highest incidence of early seizures, 13/109 (11.9%). After decompressive craniectomy, the seizure rate was 10.4% in the patients who received prophylaxis and 7.1% in the patients without prophylaxis (p = 0.738). Patients with admission GCS < 9 had an overall seizure incidence of 7.0% (9/128): 4.3% in patients with prophylaxis and 14.3% in patients without prophylaxis (p = 0.062). In further analyses of only patients with isolated blunt TBI (exclusion of patients with extracranial AIS > 3) the incidence of early seizures remained similar in the two groups [LAC + USC 6/179 (3.4%) vs Nanshan 5/205 (2.4%), p = 0.593] (Table 2).
Subgroup analysis stratified by head AIS 3, 4 and 5 showed no significant difference in the seizure rate between the two groups: head AIS 3: 6.1% in the prophylaxis group versus 2.6% in the no-prophylaxis group, p = 0.329; head AIS 4: 0 versus 2.7%, p = 0.302; head AIS 5: 8.7 versus 4.0%, p = 0.601 (Table 3).
Discussion
Post-traumatic seizures may occur early or late after TBI. Seizures occurring within 7 days of the injury are classified as early and are not considered to be epilepsy. On the other hand, seizures occurring after 7 days of admission are classified as late and are considered epilepsy [8, 9]. The prognosis and treatment of the two types of seizures are different. Any TBI, including minor injuries, may be complicated by early seizures. Pediatric patients, severe TBI, acute intracerebral hematomas, acute subdural hematomas and penetrating injuries are all associated with a higher risk of early post-traumatic seizures [10,11,12,13].
The reported incidence of early post-traumatic seizures without prophylaxis varies across the literature, largely due to the heterogeneity of the study populations and associated risk factors. In a collective review of the literature, the incidence of early seizures ranged from 2.1 to 16.9% [2, 12, 14]. In the present study, the incidence of early seizures with no prophylaxis was 2.8%, which is similar to other reports [14, 15].
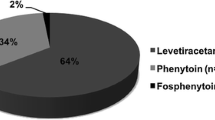
Early post-traumatic seizures may precipitate secondary brain injury by increasing cerebral metabolic demands, increasing intracranial pressure and aggravating brain edema [15]. In addition, patients with early seizures have been shown to be at higher risk for the development of epilepsy compared with those without early seizures [16]. For these reasons, pharmacological prophylaxis has been used to reduce the risk of early seizures. The most commonly used medications for prophylaxis are phenytoin and levetiracetam, administered for 7 days post-injury. Both medications show similar rates of early seizures. In a prospective multicenter study of 813 patients who received seizure prophylaxis, the incidence of early seizures was 1.5% with phenytoin and 1.5% with levetiracetam [17]. Similar results were reported by other smaller studies [18] or collective reviews [19].
The Brain Trauma Foundation Guidelines include a level II recommendation for early pharmacologic seizure prophylaxis [1]. Although this recommendation is endorsed by many professional organizations, the role of early pharmacological seizure prophylaxis on outcome is unclear. The recommendation is largely based on a randomized study performed in 1990 by Temkin et al. [2]. In this study, 404 trauma patients with blunt or penetrating TBI were randomized to receive phenytoin (n = 208) or placebo (n = 196) for 1 year. Phenytoin was associated with a significantly lower incidence of early seizures than placebo (3.6 vs 14.2%, p < 0.001), but there was no effect on late-seizure rates. These results, however, could not be replicated in subsequent analyses, which report conflicting outcomes. Young et al. conducted a randomized study of 244 patients with TBI, assigned to receive phenytoin or placebo within 24 h of injury [6]. The study reported no significant difference in the incidence of early seizures between groups (3.7% in placebo and 3.7% in prophylaxis groups). Dikmen et al. in a randomized study of 244 of TBI, who received prophylactic phenytoin or placebo, reported that, in the severely injured, phenytoin significantly impaired the performance at 1 month, and suggested that phenytoin had negative cognitive effects [5]. Bhullar et al. in a retrospective study of 93 adults with TBI found no difference in the incidence of early seizures between patients receiving phenytoin prophylaxis and patients not receiving prophylaxis (4 vs. 2.3%], p = 1) [3]. The prophylaxis group had a significantly longer hospital stay and a significantly worse functional outcome at discharge than the no-prophylaxis group, further supporting the potential negative effects of pharmacologic prophylaxis.
Despite the Brain Trauma Foundation Guidelines recommendation for early seizure prophylaxis, and perhaps in part due to concerns regarding efficacy, compliance with this recommendation varies from country to country and from center to center. A 1996 survey of 127 neurosurgical departments in Europe reported that TBI seizure prophylaxis was practised always in 12%, never in 36% and sometimes in 52% of centers [20]. In a 2007 Canadian survey of 99 neurosurgeons and 148 critical care physicians, the use of seizure prophylaxis for traumatic epidural hematoma was graded as “uncertain appropriateness” [21].
The current study showed that the incidence of early post blunt TBI clinical seizures is low, confirming the results of recent prospective studies [17]. It also demonstrated that routine early seizure prophylaxis may not be effective. This finding was consistent overall and across different injury severities with similar seizure rates regardless of prophylaxis in moderate or severe TBI with head AIS 3,4 or 5 or admission GCS < 9. Additionally, craniectomy has been reported as a significant risk factor for early seizures [22]. Despite this, seizure prophylaxis in this subgroup of TBI patients did not have any effect on the seizure rate.
Although no statistical difference was found, in the group of patients with GCS < 9, the use of seizure prophylaxis had a trend toward lower incidence of early seizures. There could be two explanations for this trend. First, at LAC + USC Medical Center, patients with a GCS < 9 are routinely intubated on arrival. These patients are not only more likely to receive benzodiazepines, but the ongoing sedation medications during mechanical ventilation may mask clinical seizures. Second, it is possible that seizure prophylaxis may have a protective effect in this subpopulation.
The present study has the strength of its large number of patients, its prospective nature and meticulous data collection. However, it is not randomized and this poses some questions. The two participating centers follow different practices in the management of TBI, such as emergency department endotracheal intubation in patients for GCS < 9, differing thresholds for use of ICP monitoring devices and the variable role of decompressive craniectomy. The role of these interventions has not been proven, and recent studies challenged the value of ICP placement and decompressive craniectomies [8, 23]. Another possible limitation is the lack of specific description of CT scan findings partially addressed by the head AIS, which is based on the CT scan findings. The AIS classification takes into account compression of the ventricles or brain stem compression/herniation. These findings are classified as AIS 5 or 6 (non-survivable). Subanalysis according to head AIS 3, 4 and 5 showed no difference in the incidence of early seizures.
Another unanswered question is the incidence of subclinical seizures in comatose patients, as no routine EEG monitoring was performed in the obtunded patients. However, almost all published studies on early seizure prophylaxis, including the seminal randomized study by Temkin et al. [2] which formed the basis of the Brain Trauma Foundation Guidelines, used only clinical seizures as the outcome of seizure prophylaxis. Finally, the study included only blunt TBI. Penetrating TBI has a much worse prognosis and higher incidence of early seizures. It is also possible that other select subgroups of TBI may benefit from prophylaxis.
These findings, in addition to the concerns about the reported negative neurobehavioral effects of phenytoin prophylaxis [5], should call into question the current practices and Brain Trauma Foundation Guidelines regarding routine early seizure prophylaxis in blunt TBIs. Having in mind the importance and implications of TBI, it is imperative that this issue is revisited and a well-designed randomized study is performed.
References
Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GW, Bell MJ et al (2017) Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery 80:6–15
Temkin NR, Dikmen SS, Wilensky AJ, Keihm J, Chabal S, Winn HR (1990) A randomized, double-blind study of phenytoin for the prevention of post-traumatic seizures. N Engl J Med 323:497–502
Bhullar IS, Johnson D, Paul JP, Kerwin AJ, Tepas JJ 3rd, Frykberg ER (2014) More harm than good: antiseizure prophylaxis after traumatic brain injury does not decrease seizure rates but may inhibit functional recovery. J Trauma Acute Care Surg 76:54–60 discussion 60-51
Dikmen SS, Machamer JE, Winn HR, Anderson GD, Temkin NR (2000) Neuropsychological effects of valproate in traumatic brain injury: a randomized trial. Neurology 54:895–902
Dikmen SS, Temkin NR, Miller B, Machamer J, Winn HR (1991) Neurobehavioral effects of phenytoin prophylaxis of posttraumatic seizures. JAMA 265:1271–1277
Young B, Rapp RP, Norton JA, Haack D, Tibbs PA, Bean JR (1983) Failure of prophylactically administered phenytoin to prevent early posttraumatic seizures. J Neurosurg 58:231–235
Gennarelli TA, Wodzin E (eds) (2005) AIS 2005. Association for the Advancement of Automotive Medicine, Barrington
Hung C, Chen JW (2012) Treatment of post-traumatic epilepsy. Curr Treat Options Neurol 14(4):293–306
Szaflarski JP, Nazzal Y, Dreer LE (2014) Post-traumatic epilepsy: current and emerging treatment options. Neuropsychiatr Dis Treat. 11(10):1469–1477
Chung MG, O’Brien NF (2016) Prevalence of early posttraumatic seizures in children with moderate to severe traumatic brain injury despite levetiracetam prophylaxis. Pediatr Crit Care Med 17:150–156
Cranley MR, Craner M, McGilloway E (2016) Antiepileptic prophylaxis following severe traumatic brain injury within a military cohort. J R Army Med Corps 162:109–114
Frey LC (2003) Epidemiology of posttraumatic epilepsy: a critical review. Epilepsia 44(Suppl 10):11–17
Won SY, Konczalla J, Dubinski D, Cattani A, Cuca C, Seifert V et al (2017) A systematic review of epileptic seizures in adults with subdural haematomas. Seizure 45:28–35
Zangbar B, Khalil M, Gruessner A, Joseph B, Friese R, Kulvatunyou N et al (2016) Levetiracetam prophylaxis for post-traumatic brain injury seizures is ineffective: a propensity score analysis. World J Surg 40:2667–2672. https://doi.org/10.1007/s00268-016-3606-y
Debenham S, Sabit B, Saluja RS, Lamoureux J, Bajsarowicz P, Maleki M et al (2011) A critical look at phenytoin use for early post-traumatic seizure prophylaxis. Can J Neurol Sci 38:896–901
Ritter AC, Wagner AK, Fabio A, Pugh MJ, Walker WC, Szaflarski JP et al (2016) Incidence and risk factors of posttraumatic seizures following traumatic brain injury: a traumatic brain injury model systems study. Epilepsia 57:1968–1977
Inaba K, Menaker J, Branco BC, Gooch J, Okoye OT, Herrold J et al (2013) A prospective multicenter comparison of levetiracetam versus phenytoin for early posttraumatic seizure prophylaxis. J Trauma Acute Care Surg 74:766–771 discussion 771-763
Szaflarski JP, Sangha KS, Lindsell CJ, Shutter LA (2010) Prospective, randomized, single-blinded comparative trial of intravenous levetiracetam versus phenytoin for seizure prophylaxis. Neurocrit Care 12:165–172
Yang Y, Zheng F, Xu X, Wang X (2016) Levetiracetam versus phenytoin for seizure prophylaxis following traumatic brain injury: a systematic review and meta-analysis. CNS Drugs 30:677–688
Dauch WA, Schutze M, Guttinger M, Bauer BL (1996) Post-traumatic seizure prevention–results of a survey of 127 neurosurgery clinics. Zentralbl Neurochir 57:190–195
Jacka MJ, Zygun D (2007) Survey of management of severe head injury in Canada. Can J Neurol Sci 34:307–312
Ritter AC, Wagner AK, Szaflarski JP, Brooks MM, Zafonte RD, Pugh MJ et al (2016) Prognostic models for predicting posttraumatic seizures during acute hospitalization, and at 1 and 2 years following traumatic brain injury. Epilepsia 57(9):1503–1514
Aiolfi A, Benjamin E, Khor D, Inaba K, Lam L, Demetriades D (2017) Brain trauma foundation guidelines for intracranial pressure monitoring: compliance and effect on outcome. World J Surg 41:1543–1549. https://doi.org/10.1007/s00268-017-3898-6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors deny any potential conflicts of interest.
Rights and permissions
About this article
Cite this article
Khor, D., Wu, J., Hong, Q. et al. Early Seizure Prophylaxis in Traumatic Brain Injuries Revisited: A Prospective Observational Study. World J Surg 42, 1727–1732 (2018). https://doi.org/10.1007/s00268-017-4373-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4373-0