Abstract
Background
Seizure following traumatic brain injury (TBI) constitutes a common complication that requires effective prevention to improve the outcome of TBI. Phenytoin has been the only recommended antiepileptic drug (AED) for seizure prophylaxis; however, several shortcomings have affected its use. Intravenous levetiracetam has been available since 2006 and has been increasingly accepted as a seizure prophylaxis for brain injury, mainly due to its favorable pharmacokinetic features and minimal adverse events profile. However, the efficacy and safety of levetiracetam versus phenytoin for seizure prophylaxis following TBI are not well clarified.
Objective
The aim of this study was to assess the efficacy and safety of levetiracetam versus phenytoin for seizure prophylaxis following TBI.
Methods
We conducted a search of the MEDLINE, EMBASE, and Cochrane library databases to March 2016, and screened original research that included patients with TBI who received levetiracetam. We included randomized controlled trials (RCTs) or controlled observational cohort studies that compared levetiracetam and phenytoin, as well as uncontrolled case series regarding prophylactic levetiracetam following TBI. The outcomes included early or late seizure prophylaxis and safety. The estimates of seizure prophylaxis were pooled using a meta-analysis, and the estimates for the case series were pooled using descriptive statistics.
Results
A total of 1614 patients from 11 studies were included in this review, of whom 1285 patients from eight controlled studies (one RCT and seven cohort studies) were included in the meta-analysis. Levetiracetam was not superior to phenytoin with regard to early seizure prophylaxis (risk ratio [RR] 1.10, 95 % confidence interval [CI] 0.64–1.88); the estimate of early seizure incidence was 0.05 (95 % CI 0.02–0.08). Three studies that assessed late seizure did not indicate the superiority of levetiracetam to phenytoin. There were no differences in mortality during hospitalization or after 6 months, or in the number of patients with adverse reactions between levetiracetam and phenytoin.
Conclusions
Levetiracetam does not appear to be superior to phenytoin in efficacy or safety with regard to early or late seizure prophylaxis following TBI; however, no class I evidence was identified. Additional evidence from high-quality studies is required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
There is no evidence indicating that levetiracetam was superior to phenytoin for early or late seizure prophylaxis following traumatic brain injury. |
The limited information regarding safety did not indicate a superiority of levetiracetam compared with phenytoin. |
More well-designed comparative studies with a large sample size are warranted. |
1 Introduction
Traumatic brain injury (TBI) is a common condition with an annual incidence of 1.7 million individuals in the US [1]. Post-traumatic seizure (PTS) is a frequent complication following TBI. Based on the occurrence time of the seizure following TBI, PTS has been divided into early seizure, which occurs within the first 7 days, and late seizure, which occurs after the first 7 days following TBI. The incidence of early seizure ranged from 2.6 to 16.3 % [2, 3], whereas the incidence of late seizure reached 0.7–7.1 % at 1 year and 1.6–11.5 % at 5 years following a moderate to severe TBI [4]. Early seizure should be intensively monitored and adequately treated to avoid secondary insults, such as hypoxia, hypotension, and hyperthermia [5]. Late seizure was difficult to control with antiepileptic drugs (AEDs) and frequently led to poor clinical outcomes, including reduced quality of life, education, and employment [6]. In addition, evidence from epidemiologic studies has indicated that early seizure may be a predictor for late seizure [7]; therefore, it may be a reasonable strategy to prevent the development of late seizure following acute TBI [8].
In 2003, the American Academy of Neurology recommended phenytoin as a seizure prophylaxis following severe TBI, based on the pooled results from two class I studies, which demonstrated a significantly lower risk of early PTS in patients receiving phenytoin compared with control (relative risk 0.37, 95 % confidence interval [CI] 0.18–0.74) [9]. In 2007, the Brain Trauma Foundation made a similar recommendation [10]. However, phenytoin has several shortcomings that have affected its use, including non-linear pharmacokinetics, drug interactions and numerous side effects [11]. In addition, concerns have been raised that phenytoin may worsen cognitive deficits and the outcomes assessed by the Glasgow Coma Scale (GCS) and modified Ranking Scale [12]. Furthermore, studies have demonstrated that phenytoin has not been effective for late seizure prophylaxis [9]; therefore, other AEDs for seizure prophylaxis are urgently needed.
Intravenous levetiracetam was approved by the US FDA in 2006. Taking advantage of its favorable pharmacokinetic features and minimal adverse events profile, levetiracetam has been widely used in seizure prophylaxis following brain injuries, including TBI [6, 11, 13, 14, 15]. A recent meta-analysis demonstrated its superiority compared with phenytoin in brain tumor patients who underwent surgery [14]. To the best of our knowledge, no class I studies have demonstrated its efficacy and safety regarding seizure prophylaxis following TBI [16]; however, several small-scale controlled studies and case series have utilized levetiracetam for seizure prophylaxis following TBI. In addition, we conducted a search of ClinicalTrials.gov and did not identify any ongoing trials regarding prophylactic levetiracetam following TBI. We therefore performed this systematic review and meta-analysis to summarize the current evidence regarding the efficacy and safety of levetiracetam in seizure prophylaxis following TBI.
2 Methods
2.1 Search Strategy
This systematic review and meta-analysis was performed in March 2016 according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRIMSA) guidelines. Inclusion criteria and methods of the review were specified in advance in a protocol that has not been published. The electronic MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials (CENTRAL) databases were searched to March 2016. Referring to the search strategy of a Cochrane review regarding epilepsy prevention after traumatic head injury [17], we had a comprehensive strategy that incorporated Medical Subject Headings (MeSH) and text words relating to TBI and levetiracetam (see electronic supplementary material). The references of relevant reviews and included articles were manually checked for potential studies. According to the search strategy, two authors (YY and ZFS) performed the literature search independently and merged all the searched articles.
2.2 Inclusion Criteria
Eligible research met the following criteria.
-
1.
Types of study: The eligible studies were randomized controlled trials (RCTs; including the first phase of crossover trials) or controlled cohort studies that compared levetiracetam with phenytoin for seizure prophylaxis following TBI. Uncontrolled case series that contained ≥10 patients receiving levetiracetam for seizure prophylaxis were also included.
-
2.
Types of participants: Patients with TBI were included in the study without restriction of age, and type and severity of TBI.
-
3.
Intervention: Intravenous levetiracetam and other AEDs in the control group were administered following TBI. No concomitant AED was used in any intervention group and no language restrictions were applied.
According to the inclusion criteria, two authors (YY and ZFS) performed the study selection independently. Article titles and abstracts were first screened, and potential studies were further reviewed in full-text articles. If multiple articles reported the same study, all articles were examined in order to extract comprehensive data. Discrepancies were resolved through discussion with the other authors (XX and WXF).
2.3 Data Extraction
Two authors (YY and ZFS) independently extracted data using a standardized data extraction form, which had been piloted with a sample of three studies and further modified prior to the initiation of full data extraction. Discrepancies were resolved through discussion with other authors (XX and WXF). The extracted data included the following: (1) basic information about the study, including study name, publication year, authors, country where the study was conducted, and the time of patients’ enrollment; (2) information about patients, including the number of patients in each intervention group, age, sex, and type and severity of TBI; (3) study design, including RCT, controlled observational cohort study or uncontrolled case series, duration of follow-up, and duration of AEDs used; and (4) data on outcomes, including incidence of early seizure, late seizure, adverse effects, and all-cause mortality during hospitalization or a specified follow-up period.
2.4 Quality Evaluation
Two authors (YY and ZFS) independently evaluated the quality of the study. Two tools for quality assessment, the Cochrane Collaboration’s tool and the Newcastle–Ottawa Scale, were implemented based on the type of included studies. If two or more RCTs were included, we assessed the quality of these RCTs using the Cochrane Collaboration’s tool, which is typically used to evaluate RCTs. If less than two RCTs and controlled cohort studies were included, we assessed the quality of all controlled studies using the Newcastle–Ottawa Scale, a ‘star system’ tool typically used to assess cohort and case–control studies [18]. Generally, studies with no less than six stars were considered of high quality. Discrepancies were resolved through discussion with the other authors (XX and WXF).
2.5 Statistical Analysis
For the controlled studies that compared levetiracetam with phenytoin, we performed a meta-analysis if data were available for more than one study, and the risk ratio (RR) and 95 % CI were calculated. In cases in which a zero value was present, a 0.5 continuity correction was applied to all four cells. Initially, a fixed effects model with the Mantel–Haenszel method was used to obtain a pooled effect estimate and the between-study heterogeneity (the Cochran’s Q statistic and the I 2 statistic). A p value ≤0.05 or an I 2 value ≥75 % was considered significant heterogeneity. A sensitivity analysis was subsequently performed by removing studies of low quality to identify the source of the heterogeneity, with a subgroup analysis being conducted if necessary. Finally, if the heterogeneity was not controlled, the random-effects model using the DerSimonian and Laird method was used to pool the effect estimate. In the meta-analysis that compared levetiracetam and phenytoin, statistical significance was present when the 95 % CI did not span one (p < 0.05 in the forest plot). The estimate of the seizure incidence was calculated using the DerSimonian and Laird method within the random-effects setting. If heterogeneity was noted (a p value ≤0.05 or an I 2 value ≥75 %), a sensitivity analysis was conducted by removing the case series. The publication bias was assessed using the Egger test and visual inspection of the funnel plot.
3 Results
3.1 Study Selection and Study Characteristics
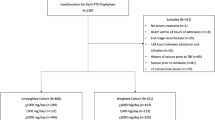
We identified 983 unique articles (Fig. 1). Thirty-eight studies were selected for full-text review, of which 11 studies containing 1614 patients were included in the final dataset [19–29]. Of the 11 studies, eight (one RCT and seven controlled cohort studies) compared levetiracetam with phenytoin, two were case series that reported the seizure incidence after prophylactic levetiracetam, and one study that comprised an observation intervention as the control group was considered a case series for extracting data regarding levetiracetam for seizure prophylaxis (Table 1). Therefore, the Newcastle–Ottawa Scale was used to assess the quality of the eight controlled studies that compared levetiracetam with phenytoin. Six studies were scored no less than six stars, indicating high quality, and two studies were scored five stars (Table 2). In general, the studies were of good quality. For early seizure, most studies included a follow-up of at least 7 days, with the exception of the study by Szaflarski et al., which followed up for 3 days after TBI using electroencephalogram [29]. In the meta-analysis of early seizure prophylaxis, no evidence of publication bias was noted (Egger test, p = 0.302; funnel plot is shown in Fig. 2).
3.2 Early Seizure Prophylaxis
For the meta-analysis of early seizure prophylaxis comparing levetiracetam with phenytoin, a total of 1285 patients (levetiracetam, n = 573; phenytoin, n = 712) from one RCT and seven controlled cohort studies were included. No statistically significant difference in the incidence of early seizure was identified between the two treatments (RR 1.10, 95 % CI 0.64–1.88), and no evidence of statistical heterogeneity between individual trials was noted using both the I 2 statistic (I 2 = 0 %) and Cochran Q statistic (p = 0.87) [Fig. 3].
For the estimate of early seizure incidence under levetiracetam prophylaxis, after excluding the study by Gabriel and Rowe [23], which contained only five patients in the levetiracetam group, a total of 32/771 patients from nine studies (seven controlled studies and two case series) had an early seizure under prophylactic levetiracetam. The estimate of early seizure incidence was 0.05 (95 % CI 0.02–0.08), and moderate heterogeneity between the individual trials was identified (p = 0.016, I 2 = 57.4 %) [Fig. 4]. A sensitivity analysis was performed by removing two case series [22, 28], and indicated a slight increase in the risk of early seizure with a pooled RR of 0.06 (95 % CI 0.02–0.10).
3.3 Late Seizure Prophylaxis
As a result of identification of only three studies with different study designs that evaluated late seizure, we performed a qualitative appraisal. A small RCT investigated late seizure at 6 months following TBI, and indicated that late seizure occurred in 1 of 20 patients who received levetiracetam and none of the 14 patients who received phenytoin (p < 0.05) [29]. A prospective cohort study with a small sample size investigated late seizure during the 6 months or more following TBI, and indicated there was no difference in late seizure prevention (levetiracetam 0/5 vs. phenytoin 2/14; p = 0.53) [23]. A retrospective cohort study that utilized observation treatment as the control group evaluated late seizure during the 2 years following TBI. This study indicated there was no difference between the two groups in adult patients (levetiracetam 5/46 vs. observation 8/40; p = 0.96) or patients in all age ranges (levetiracetam 6/66 vs. observation 8/60; p = 0.95) [26].
3.4 Safety Evaluation
As a result of the inconsistent reports regarding safety outcomes, we performed a qualitative appraisal. For the side effects, a large, multicenter study that included 406 individuals in the levetiracetam group and 407 individuals in the phenytoin group indicated there was no difference between the groups in adverse drug reactions (levetiracetam 7.9 % vs. phenytoin 10.3 %; p = 0.227) [24]. The study from Gabriel and Rowe indicated there were no differences in side effects between the groups (levetiracetam 1/5 vs. phenytoin 3/14; p = 0.73) [23]. The study from Carter et al. also demonstrated there were no differences in side effects between the groups (levetiracetam 3/36 vs. phenytoin 4/65; p = not significant) [21]. For all-cause mortality, no differences were identified in the study from Szaflarski et al. [29] during the 6 months following TBI (levetiracetam 12/34 vs. phenytoin 4/18; p = 0.227), in the study from Kruer et al. [27] during hospitalization (levetiracetam 6/20 vs. phenytoin 35/89; p = not significant), or in the study by Inaba et al. [24] during hospitalization (levetiracetam 5.4 % vs. phenytoin 3.7 %; p = 0.236). In a study with 2 years of follow-up, levetiracetam treatment for 30 days did not improve all-cause mortality throughout the 2 years (levetiracetam 5/46 vs. observation 3/40; p = 0.96) [26].
4 Discussion
In the present systematic review and meta-analysis, 1614 patients from 11 studies were included. For the meta-analysis of early seizure prophylaxis comparing levetiracetam with phenytoin, 1285 patients from one RCT and seven controlled cohort studies were analyzed. Prophylactic levetiracetam does not appear to be superior to phenytoin (RR 1.10, 95 % CI 0.64–1.88). For the estimate of the early seizure incidence under levetiracetam prophylaxis, 771 patients from nine studies were analyzed, and the estimate of the early seizure incidence was 0.05 (95 % CI 0.02–0.08). Late seizure was evaluated in three individual studies, and no superiority was identified in the levetiracetam group compared with phenytoin. No evidence of safety assessment was identified that favoured levetiracetam.
Several meta-analyses had addressed that AEDs were needed for seizure prophylaxis following brain injuries. In 1998, Schierhout and Roberts analyzed 10 RCTs that included 2036 patients with acute traumatic head injury. The authors determined that prophylactic AEDs (including carbamazepine, phenobarbitone and phenytoin) were effective in reducing the occurrence of early seizure but not late seizure [30]. A recent Cochrane meta-analysis of RCTs in 2015 indicated that early treatment with an AED (phenytoin or carbamazepine) compared with placebo or standard care may reduce the risk of early PTS; however, it did not reduce the risk of late seizure or mortality [17].
Among carbamazepine [31], valproate [32], and phenytoin [33–37], which were indicated by RCTs to be effective for seizure prophylaxis following TBI, phenytoin was the most investigated drug. A large-scale, placebo-controlled RCT assessed 208 patients who received phenytoin and 196 patients who received placebo for 1 year. Compared with the placebo, phenytoin significantly decreased the risk of early seizure (3.6 vs. 14.2 %; p < 0.001) but not late seizure [34]. Primarily because of this study, phenytoin was recommended for early but not late seizure prophylaxis by the American Academy of Neurology in 2003 and the Brain Trauma Foundation in 2007 [9, 10]; however, phenytoin use was not without drawbacks, especially the need for serum drug monitoring [38].
Since approved by the FDA in 2006, intravenous levetiracetam has been widely used for seizure prophylaxis following various brain injuries. In 2012, Zafar et al. performed a meta-analysis that assessed seizure prophylaxis following various brain injuries, with the authors determining that levetiracetam was not superior to phenytoin for early or late seizure prevention [39]. Most recently, a systematic review and meta-analysis was performed to assess levetiracetam for supratentorial brain tumor surgery. The authors concluded that prophylactic levetiracetam appeared to be superior to phenytoin and valproate in reducing postoperative seizure and led to fewer side effects [14]. Furthermore, Kruer et al. assessed the prescription for seizure prophylaxis at Johns Hopkins Hospital and determined that there was a significant shift in prescriptions away from phenytoin and toward levetiracetam between 2008 and 2010 [27].
Levetiracetam has become an appealing alternative; however, a high quality, head-to-head RCT between phenytoin and levetiracetam was lacking. In this systematic review and meta-analysis, using a systematic search, one RCT and seven controlled cohort studies were included for the comparisons of the two AEDs.
Based on the analysis of this review, effectiveness or safety did not contribute towards making a better choice from the two AEDs. The superiority of levetiracetam to phenytoin in early seizure prophylaxis was not demonstrated in all eight individual controlled studies or the pooled data obtained from these studies (RR 1.10, 95 % CI 0.64–1.88). The estimate of early seizure incidence in levetiracetam treatment was 0.05 (95 % CI 0.02–0.08), which was similar to 3.6 % with phenytoin treatment reported in a high-quality study [34]. However, as a result of low incidence, a study with large sample size is required to confirm the efficacy of levetiracetam compared with phenytoin.
Severe TBI may lead to an extreme emergency condition, which may be susceptible to adverse events, such as thrombocytopenia and unexplained fever in phenytoin treatment [40]. The remarkable effect of phenytoin in drug–drug reactions, as well as the elevation of hepatic enzymes, may affect the treatment of TBI [41]. The wide use of levetiracetam has largely benefited from its minimal adverse events profile [42]; however, somewhat surprisingly, no superiority regarding adverse effects that favored levetiracetam was indentified in three individual studies [21, 23, 24]. Death during hospitalization or the 6 months following TBI also did not favor levetiracetam [24, 27, 29]; this may be limited by small sample size and poor study design.
In addition to the efficacy and safety evaluation, pharmacoeconomic evaluation comprises a useful approach for choosing a better drug. In 2010, a cost-effectiveness analysis was conducted from the perspective of a university Level I urban trauma center in Houston. The cost-effectiveness ratios for early seizure prophylaxis were US$1.58/quality-adjusted life-years (QALYs) for phenytoin and US$20.72/QALY for levetiracetam, which was significantly favorable for phenytoin [43]. In 2011, a cost-minimization analysis for early seizure prophylaxis following TBI was performed based on two studies that were conducted in the US [25, 29]. As a result, the phenytoin strategy was superior to the levetiracetam strategy from the perspectives of both the institution (mean cost per patient US$151.24 vs. US$411.85, respectively) and patient (mean charge per patient US$2302.58 vs. US$3498.40, respectively) [44].
This meta-analysis may be subject to several limitations. First, it mainly included observational cohort studies, which may induce a selective bias from various potential confounding factors. Most studies recruited patients with a median or mean age of more than 45 years, and male patients outnumbered female patients, which was not consistent with previous studies that indicated the incidence of TBI was approximately the same in men and women over the age of 45 years [45–47]. Several important baseline conditions were also difficult to balance in cohort studies, such as systolic blood pressure at admission and severity of TBI [23, 24]. The only RCT that contained a small sample size had several limitations, such as the inclusion of a small proportion of patients with subarachnoid hemorrhage, seizure diagnosed by EEG, and an insufficient follow-up of 3 days after admission [29]. Second, this meta-analysis may be affected by clinical heterogeneity, although statistical heterogeneity between the individual studies was not noted (p = 0.87, I 2 = 0 %). TBI severity (usually assessed by GCS) affects seizure occurrence [2, 4, 48]; however, it was difficult to exclude the influence from TBI severity by subgroup analysis because most studies had an overlapping GCS score. Third, the incidence of seizure under prophylactic AEDs was low, and a small sample size of 1285 patients was included for the meta-analysis of early seizure prophylaxis. Thus, it is not surprising that the point estimate may be imprecise, with a 95 % CI that covers the entire spectrum from benefit to harm.
5 Conclusions
Based on current evidence, this systematic review and meta-analysis indicated that levetiracetam and phenytoin had similar efficacy and safety for seizure prevention following TBI. A pharmacoeconomic evaluation conducted by other scholars favored phenytoin, while levetiracetam may be more convenient because drug monitoring is not required [43, 44]. Therefore, to date it is difficult to propose a more preferable recommendation between levetiracetam and phenytoin, and both AEDs are a good choice for seizure prophylaxis following TBI [49]; however, class I evidence is lacking. Thus, in future, well-designed RCTs or large-scale, prospective cohort studies are needed to compare the efficacy and safety of levetiracetam on seizure prophylaxis following TBI. Some important factors that may affect the occurrence of seizure should be considered when a study is designed, such as age, TBI severity, etc. Furthermore, studies regarding the prevention of late seizure and children should be performed.
References
Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths. Atlanta: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010.
Annegers JF, Hauser WA, Coan SP, Rocca WA. A population-based study of seizures after traumatic brain injuries. N Engl J Med. 1998;338(1):20–4.
Asikainen I, Kaste M, Sarna S. Early and late posttraumatic seizures in traumatic brain injury rehabilitation patients: brain injury factors causing late seizures and influence of seizures on long-term outcome. Epilepsia. 1999;40(5):584–9.
Annegers JF, Grabow JD, Groover RV, Laws ER Jr, Elveback LR, Kurland LT. Seizures after head trauma: a population study. Neurology. 1980;30(7):683–9.
Guilliams K, Wainwright MS. Pathophysiology and management of moderate and severe traumatic brain injury in children. J Child Neurol. 2016;31(1):35–45.
Szaflarski JP, Nazzal Y, Dreer LE. Post-traumatic epilepsy: current and emerging treatment options. Neuropsychiatr Dis Treat. 2014;10:1469–77.
Loscher W, Brandt C. Prevention or modification of epileptogenesis after brain insults: experimental approaches and translational research. Pharmacol Rev. 2010;62(4):668–700.
Wyllie E. Wyllie’s treatment of epilepsy. 5th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2010.
Chang BS, Lowenstein DH. Practice parameter: antiepileptic drug prophylaxis in severe traumatic brain injury: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2003;60(1):10–6.
Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, et al. Guidelines for the management of severe traumatic brain injury. XIII. Antiseizure prophylaxis. J Neurotrauma. 2007;24(Suppl 1):S83–6.
Fuller KL, Wang YY, Cook MJ, Murphy MA, D’Souza WJ. Tolerability, safety, and side effects of levetiracetam versus phenytoin in intravenous and total prophylactic regimen among craniotomy patients: a prospective randomized study. Epilepsia. 2013;54(1):45–57.
Bhullar IS, Johnson D, Paul JP, Kerwin AJ, Tepas JJ 3rd, Frykberg ER. More harm than good: antiseizure prophylaxis after traumatic brain injury does not decrease seizure rates but may inhibit functional recovery. J Trauma Acute Care Surg. 2014;76(1):54–60 (discussion 60–51).
Virant-Young D, Alexander R, Umstead G, Savoy-Moore R, Himes D, Nikolavsky M, et al. Retrospective analysis of phenytoin and levetiracetam for seizure prophylaxis after traumatic brain injury. Crit Care Med. 2009;37(12):A443.
Pourzitaki C, Tsaousi G, Apostolidou E, Karakoulas K, Kouvelas D, Amaniti E. Efficacy and safety of prophylactic levetiracetam in supratentorial brain tumour surgery: a systematic review and meta-analysis. Br J Clin Pharmacol. 2016. doi:10.1111/bcp.12926 (Epub 5 Mar 2016).
Iuchi T, Kuwabara K, Matsumoto M, Kawasaki K, Hasegawa Y, Sakaida T. Levetiracetam versus phenytoin for seizure prophylaxis during and early after craniotomy for brain tumours: a phase II prospective, randomised study. J Neurol Neurosurg Psychiatry. 2015;86(10):1158–62.
Rowe AS, Goodwin H, Brophy GM, Bushwitz J, Castle A, Deen D, et al. Seizure prophylaxis in neurocritical care: a review of evidence-based support. Pharmacotherapy. 2014;34(4):396–409.
Thompson K, Pohlmann-Eden B, Campbell LA, Abel H. Pharmacological treatments for preventing epilepsy following traumatic head injury. Cochrane Database Syst Rev. 2015;8:CD009900.
Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2013. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed Nov 2013.
Anderson R, Montero J. Utilization of seizure prophylaxis in traumatic brain injury (TBI) patients. Crit Care Med. 2014;42(12):A1626.
Caballero GC, Hughes DW, Maxwell PR, Green K, Gamboa CD, Barthol CA. Retrospective analysis of levetiracetam compared to phenytoin for seizure prophylaxis in adults with traumatic brain injury. Hosp Pharm. 2013;48(9):757–61.
Carter D, Askari R, Frawley B, Rogers S. Evaluation of the use of phenytoin and levetiracetam for seizure prophylaxis in patients with traumatic brain injury. Crit Care Med. 2009;37(12):A77.
Chung MG, O’Brien NF. Prevalence of early posttraumatic seizures in children with moderate to severe traumatic brain injury despite levetiracetam prophylaxis. Pediatr Crit Care Med. 2016;17(2):150–6.
Gabriel WM, Rowe AS. Long-term comparison of GOS-E scores in patients treated with phenytoin or levetiracetam for posttraumatic seizure prophylaxis after traumatic brain injury. Ann Pharmacother. 2014;48(11):1440–4.
Inaba K, Menaker J, Branco BC, Gooch J, Okoye OT, Herrold J, et al. A prospective multicenter comparison of levetiracetam versus phenytoin for early posttraumatic seizure prophylaxis. J Trauma Acute Care Surg. 2013;74(3):766–71 (discussion 771–763).
Jones KE, Puccio AM, Harshman KJ, Falcione B, Benedict N, Jankowitz BT, et al. Levetiracetam versus phenytoin for seizure prophylaxis in severe traumatic brain injury. Neurosurg Focus. 2008;25(4):E3.
Klein P, Herr D, Pearl PL, Natale J, Levine Z, Nogay C, et al. Results of phase 2 safety and feasibility study of treatment with levetiracetam for prevention of posttraumatic epilepsy. Arch Neurol. 2012;69(10):1290–5.
Kruer RM, Harris LH, Goodwin H, Kornbluth J, Thomas KP, Slater LA, et al. Changing trends in the use of seizure prophylaxis after traumatic brain injury: a shift from phenytoin to levetiracetam. J Crit Care. 2013;28(5):883.
Patanwala AE, Kurita A, Truong E. Low-dose levetiracetam for seizure prophylaxis after traumatic brain injury. Brain Inj. 2016;30(2):156–8.
Szaflarski JP, Sangha KS, Lindsell CJ, Shutter LA. Prospective, randomized, single-blinded comparative trial of intravenous levetiracetam versus phenytoin for seizure prophylaxis. Neurocrit Care. 2010;12(2):165–72.
Schierhout G, Roberts I. Prophylactic antiepileptic agents after head injury. A systematic review. J Neurol Neurosurg Psychiatry. 1998;64(1):108–12.
Glotzner FL, Haubitz I, Miltner F, Kapp G, Pflughaupt KW. Seizure prevention using carbamazepine following severe brain injuries [in German]. Neurochirurgia (Stuttg). 1983;26(3):66–79.
Temkin NR, Dikmen SS, Anderson GD, Wilensky AJ, Holmes MD, Cohen W, et al. Valproate therapy for prevention of posttraumatic seizures: a randomized trial. J Neurosurg. 1999;91(4):593–600.
Pechadre JC, Lauxerois M, Colnet G, Commun C, Dimicoli C, Bonnard M, et al. Prevention of late post-traumatic epilepsy by phenytoin in severe brain injuries. 2 years’ follow-up [in French]. Presse Med. 1991;20(18):841–5.
Temkin NR, Dikmen SS, Wilensky AJ, Keihm J, Chabal S, Winn HR. A randomized, double-blind study of phenytoin for the prevention of post-traumatic seizures. N Engl J Med. 1990;323(8):497–502.
Young B, Rapp RP, Norton JA, Haack D, Tibbs PA, Bean JR. Failure of prophylactically administered phenytoin to prevent early posttraumatic seizures. J Neurosurg. 1983;58(2):231–5.
Young KD, Okada PJ, Sokolove PE, Palchak MJ, Panacek EA, Baren JM, et al. A randomized, double-blinded, placebo-controlled trial of phenytoin for the prevention of early posttraumatic seizures in children with moderate to severe blunt head injury. Ann Emerg Med. 2004;43(4):435–46.
McQueen JK, Blackwood DH, Harris P, Kalbag RM, Johnson AL. Low risk of late post-traumatic seizures following severe head injury: implications for clinical trials of prophylaxis. J Neurol Neurosurg Psychiatry. 1983;46(10):899–904.
Winter ME. Phenytoin and fosphenytoin. In: Murphy JE, editor. Clinical pharmacokinetics. Bethesda: American Society of Health-System Pharmacists; 2008. p. 247–64.
Zafar SN, Khan AA, Ghauri AA, Shamim MS. Phenytoin versus leviteracetam for seizure prophylaxis after brain injury: a meta analysis. BMC Neurol. 2012;12:30.
Shah D, Husain AM. Utility of levetiracetam in patients with subarachnoid hemorrhage. Seizure. 2009;18(10):676–9.
Jones GL, Wimbish GH, McIntosh WE. Phenytoin: basic and clinical pharmacology. Med Res Rev. 1983;3(4):383–434.
De Smedt T, Raedt R, Vonck K, Boon P. Levetiracetam. part II, the clinical profile of a novel anticonvulsant drug. CNS Drug Rev. 2007;13(1):57–78.
Cotton BA, Kao LS, Kozar R, Holcomb JB. Cost-utility analysis of levetiracetam and phenytoin for posttraumatic seizure prophylaxis. J Trauma. 2011;71(2):375–9.
Pieracci FM, Moore EE, Beauchamp K, Tebockhorst S, Barnett CC, Bensard DD, et al. A cost-minimization analysis of phenytoin versus levetiracetam for early seizure pharmacoprophylaxis after traumatic brain injury. J Trauma Acute Care Surg. 2012;72(1):276–81.
Hahn YS, Fuchs S, Flannery AM, Barthel MJ, McLone DG. Factors influencing posttraumatic seizures in children. Neurosurgery. 1988;22(5):864–7.
Henry PC, Hauber RP, Rice M. Factors associated with closed head injury in a pediatric population. J Neurosci Nurs. 1992;24(6):311–6.
Pentland B, Jones PA, Roy CW, Miller JD. Head injury in the elderly. Age Ageing. 1986;15(4):193–202.
Haltiner AM, Temkin NR, Dikmen SS. Risk of seizure recurrence after the first late posttraumatic seizure. Arch Phys Med Rehabil. 1997;78(8):835–40.
Szaflarski JP. Is there equipoise between phenytoin and levetiracetam for seizure prevention in traumatic brain injury? Epilepsy Curr. 2015;15(2):94–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the National Natural Science Foundation of China (Grant Numbers 81271445 and 81501122) and the National Clinical Key Specialty Construction Foundation of China.
Conflicts of interest
Yong Yang, Fangshuo Zheng, Xin Xu and Xuefeng Wang declare that they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yang, Y., Zheng, F., Xu, X. et al. Levetiracetam Versus Phenytoin for Seizure Prophylaxis Following Traumatic Brain Injury: A Systematic Review and Meta-Analysis. CNS Drugs 30, 677–688 (2016). https://doi.org/10.1007/s40263-016-0365-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-016-0365-0