Abstract
Introduction
Early seizures after severe traumatic brain injury (TBI) have a reported incidence of up to 15 %. Prophylaxis for early seizures using 1 week of phenytoin is considered standard of care for seizure prevention. However, many centers have substituted the anticonvulsant levetiracetam without good data on the efficacy of this approach. Our hypothesis was that the treatment with levetiracetam is not effective in preventing early post-traumatic seizures.
Methods
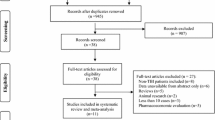
All trauma patients sustaining a TBI from January 2007 to December 2009 at an urban level-one trauma center were retrospectively analyzed. Seizures were identified from a prospectively gathered morbidity database and anticonvulsant use from the pharmacy database. Statistical comparisons were made by Chi square, t tests, and logistic regression modeling. Patients who received levetiracetam prophylaxis were matched 1:1 using propensity score matching with those who did not receive the drug.
Results
5551 trauma patients suffered a TBI during the study period, with an overall seizure rate of 0.7 % (39/5551). Of the total population, 1795 were diagnosed with severe TBI (Head AIS score 3–5). Seizures were 25 times more likely in the severe TBI group than in the non-severe group [2.0 % (36/1795) vs. 0.08 % (3/3756); OR 25.6; 95 % CI 7.8–83.2; p < 0.0001]. Of the patients who had seizures after severe TBI, 25 % (9/36) received pharmacologic prophylaxis with levetiracetam, phenytoin, or fosphenytoin. In a matched cohort by propensity scores, no difference was seen in seizure rates between the levetiracetam group and no-prophylaxis group (1.9 vs. 3.4 %, p = 0.50).
Conclusions
In this propensity score-matched cohort analysis, levetiracetam prophylaxis was ineffective in preventing seizures as the rate of seizures was similar whether patients did or did not receive the drug. The incidence of post-traumatic seizures in severe TBI patients was only 2.0 % in this study; therefore we question the benefit of routine prophylactic anticonvulsant therapy in patients with TBI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the US Center for Disease Control and Prevention, an estimated 2.5 million Americans sustain a traumatic brain injury (TBI) annually, of whom 15 % develop post-traumatic early seizures [1, 2]. Pharmacological prophylaxis has been suggested in the literature to prevent development of a permanent seizure foci [3, 4]. Classically post-traumatic seizure prophylaxis is performed using a 1-week course of phenytoin to reduce early seizures, with acceptable results. Temkin et al. [5] published data in 1990 showing a 75 % reduction in early seizures following TBI using this approach. The Traumatic Brain Injury Guidelines of the Brain Trauma Foundation currently recommend anticonvulsant administration as a prophylaxis to prevent early post-traumatic seizure [6]. However, there have been some subsequent studies showing that in some patient groups the rate of early post-traumatic seizures is much lower and phenytoin administration did not substantially reduce this rate [7].
Although standard prophylaxis in post-traumatic seizure prophylaxis is phenytoin for 1 week, there are disadvantages such as the requirement for drug level monitoring and potential for adverse side effects [8, 9]. Many centers have now substituted levetiracetam as an alternative due the ease of dosing and no requirement of blood level monitoring. However, the cost of levetiracetam is significantly greater than standard therapy using phenytoin. Recent cost analysis studies have confirmed the significant increase in cost, despite the lack of necessity for drug monitoring with levetiracetam [10, 11]. Aside from concerns over the price of the therapy, there are limited data demonstrating the efficacy of levetiracetam in TBI patients. Only a few small studies have suggested levetiracetam as a feasible alternative [3, 12] and none of these studies have compared levetiracetam therapy to a patient group who did not receive any prophylaxis.
The aim of our study was to assess the efficacy of a 1-week course of levetiracetam in the prophylaxis of early post-traumatic seizures. We hypothesized that the treatment with levetiracetam is not effective in preventing early post-traumatic seizures.
Methods
Study settings and patients
After obtaining approval from the Institutional Review Board (IRB) at the University of Arizona, College of Medicine, we performed a 3-year (from January 2007 to December 2009) retrospective cohort analysis of all trauma patients sustaining TBI at an urban level-one trauma center. Seizures were identified from a prospectively gathered morbidity database, and anticonvulsant use (levetiracetam, phenytoin, fosphenytoin) was extracted from the pharmacy database. During the study period, we did not have a specific protocol for levetiracetam administration for seizure prophylaxis, and this was at the discretion of our Neurosurgeons. Thus, we had a significant population of patients who did not receive any seizure prophylaxis.
Data points and definitions
Patient’s medical records were reviewed and the following data points were recorded: patient demographics (age, gender), mechanism of injury, vitals on presentation (systolic blood pressure, heart rate, temperature), Glasgow coma scale (GCS) Score, hospital and Intensive Care Unit (ICU) length of stay, and in-hospital mortality. Injury Severity Score (ISS) and head Abbreviated Injury Scale (AIS) were extracted from trauma registry. Patients were stratified based on head AIS. We defined mild TBI as head AIS 1 and 2, and severe TBI as head AIS 3–5. Patients with a head AIS of 6 were excluded.
Data presentation
For our statistical analysis, we used IBM Statistical Package for Social Sciences (SPSS, Version 21.0; IBM, Inc., Armonk, New York). Continuous data are presented as the mean and standard deviation. Continuous variables were compared using independent samples t test. For the matched pairs, continuous variables were compared using Wilcoxon Signed Ranks test. Ordinal data are presented as the median and interquartile range (IQR). Test of median was used to compare the ordinal variables. Categorical data are presented as proportions and percentages. Chi square test was used to compare categorical variables. For the matched pairs McNemar test was used for comparison.
Statistical analysis: propensity score matching
We matched the patients who received levetiracetam prophylaxis in a 1:1 ratio (levetiracetam:no levetiracetam) to patients who did not receive any pharmacologic prophylaxis, using propensity score matching process to eliminate possible treatment bias. Patients who received either phenytoin or fosphenytoin were not included in the matching. We adjusted our match for age, gender, ISS, head AIS, emergency department GCS, heart rate, systolic blood pressure, and mechanism of injury. Propensity score matching is an analog to the process of randomization of a clinical trial that is commonly used in observational studies. The propensity score denotes the conditional probability of an individual to receive a certain treatment. A propensity score is generated for each patient based on all the confounding factors using a logistic regression model. We used logistic regression estimation algorithm and nearest neighbor matching algorithm without replacement. Our outcome measure was incidence of seizure.
Statistical analysis: univariate and multivariate analysis
Univariate analysis was performed to assess factors predicting seizures in patients with severe TBI. Factors with p < 0.2 on univariate analysis were used in a multivariate regression analysis. Logistic regression was performed for the development of seizures adjusting for age, gender, ISS, head AIS, emergency department GCS, heart rate, systolic blood pressure, mechanism of injury, and levetiracetam prophylaxis. For multivariate analysis we considered p value <0.05 as statistically significant.
Results
During the study period, 5551 trauma patients who suffered TBI were identified. Mean age was 35.7 ± 21.6 years, 66.6 % were male, and 96.9 % had blunt mechanism of injury. The overall seizure rate was 0.7 % (39/5551) and mortality was 5.3 % (294/5551). Table 1 shows the demographics, admission vital signs, and injury characteristics of our study population.
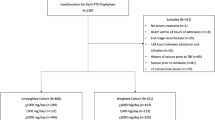
Of the total population, 32.3 % (n = 1795) patients sustained severe TBI. Severe TBI patients were 25 times more likely than the mild TBI patients to have seizures [2.0 % (36/1795) vs. 0.08 % (3/3756); OR 25.6; 95 % CI 7.8–83.2; p < 0.0001]. 18.0 % (n = 324) of the severe TBI patients received seizure prophylaxis of which 64.2 % (n = 208) of the patients received levetiracetam, while 34.3 % (n = 111) of the patients received phenytoin and 1.6 % (n = 5) of the patients received fosphenytoin for prophylaxis (Fig. 1). There was no difference in seizure rates in patients with severe TBI who received seizure prophylaxis with levetiracetam (1.9 % [4/208], p = 0.93), phenytoin (4.5 % [5/111], p = 0.06), and fosphenytoin (0 % [0/5], p = 0.76]) compared to patients who did not receive any prophylaxis (1.8 % [27/1471]). Stratification of TBI into terciles of mild, moderate, or severe TBI based on admission GCS (<9, 9–12, >12) did not show any statistical differences in seizure rate. In patients with severe TBI, there was no difference in the seizure rate based on the type of injury, e.g., skull fracture, and subarachnoid versus subdural versus epidural hemorrhage.
A total of 416 patients were included in the analysis after propensity score matching. We matched 208 patients who received levetiracetam (levetiracetam group) to 208 patients who did not receive any prophylaxis (no-levetiracetam group) controlling for confounding factors. After matching there was no difference in patient characteristics and confounding factors (Table 2). No difference was seen in seizure rates between the two groups (1.9 vs. 3.4 %, p = 0.50).
In univariate analysis, age (p = 0.19), head AIS (p = 0.001), and phenytoin prophylaxis (p = 0.06) were associated with the development of seizures (Table 3). After adjusting for factors associated with the development of seizure, only head AIS (p = 0.002) was independently associated with development of seizures in patients with severe TBI. levetiracetam and phenytoin prophylaxis were not associated with the development of seizures (Table 4).
Discussion
With the increasing use of levetiracetam as an alternative to phenytoin in the early post-traumatic seizure prophylaxis, its beneficial role has been questioned [13, 14]. Our study reports no benefit of levetiracetam prophylaxis in seizure prevention compared to no prophylaxis. Our study also raises questions on the benefit of any kind of seizure prophylaxis post TBI, as an extremely low rate of post-TBI seizures was observed. This is consistent with another recent study that also showed a very low rate of post-traumatic seizures [15]. Considering its higher cost without any additive benefits, the role of levetiracetam prophylaxis for early post-TBI seizures needs to be reconsidered.
Post-traumatic seizures remain a significant concern for many physicians after traumatic brain injury, especially in the early phase [16]. Seizures during the early phase of traumatic brain injury can aggravate the brain edema and inflammatory insult to neurons. This potentially lethal adverse effects cause physicians to take extra preventive measures. Phenytoin prophylaxis for 1 week after traumatic brain injury became standard of care in this background. Later, Temkin et al. [5] provided evidence of protective effects of phenytoin prophylaxis. Phenytoin-related adverse drug events and need of drug level monitoring require probing into alternatives [9]. However, we found that there was no statistically significant difference using phenytoin prophylaxis compared to no prophylaxis.
Over the past few years, post-traumatic seizure prophylaxis has shifted toward levetiracetam due to its relative ease of use and safety profile [13]. However, literature remain divided on its clinical utility. Szaflarski et al. [3] in a prospective randomized study, reported equal efficacy of phenytoin compared to levetiracetam with the latter showing better results on disability rating scale and Glasgow outcome scale. However, this study was underpowered to detect any sizeable difference in early seizure incidence between the groups. Contrary to that, there are other studies that question the safety of levetiracetam compared to phenytoin; Jones et al. [12] reported similar rates of early post-traumatic seizures with levetiracetam therapy associated with increased seizure tendency . However, no study to our knowledge has reported the comparison between levetiracetam prophylaxis and no prophylaxis. Our study adds a unique piece of evidence to the existing literature reporting relative efficacy of levetiracetam in post-traumatic seizure prevention. The results of our study suggest that in a well-matched cohort of patients, seizure prophylaxis with levetiracetam made no difference in seizure incidence.
Most of the studies reporting the potential benefits of seizure prophylaxis include all patients with traumatic brain injury. It has been previously established in literature that injury severity is a significant determinant of post-traumatic seizure incidence. The skew induced by mild and moderate TBI in patient population may be responsible for this protective association. To overcome this potential bias, in our final analysis we only included patients with severe traumatic brain injury. Furthermore, our patient cohorts were matched using propensity score matching to add clarity to the association. The results from the matched cohort of patients in our study raise thoughtful questions on utility of levetiracetam in post-traumatic seizures. We observed no difference in seizure rate in levetiracetam patients compared to no prophylaxis. Although relatively safer than phenytoin, the cost of prophylaxis with levetiracetam compared to phenytoin is controversial. While Cotton et al. [10] and Pieracci et al. [11] found levetiracetam prophylaxis to have a significant cost burden, Caballero et al. [17] in a recent retrospective study showed the overall cost benefit to be in favor of levetiracetam prophylaxis as compared to phenytoin.
Several studies have tried to identify factors associated with the development of early post-traumatic seizures [18–20]. Most of the studies looking at the predictors of post-traumatic seizure development identified type and severity of injury along with age, penetrating mechanism, and loss of consciousness at the time of injury to be associated with seizure development in early phase of TBI [18]. However, in our study we observed no such association for age, mechanism, and type of injury, and only injury severity predicted seizure development.
An interesting finding in our study was the lack of association between seizure prophylaxis and the development of seizures. Congruent with our data from propensity-matched sample, results of our multivariate regression analysis also showed no association between prophylaxis and prevention of seizures. Considering the published literature on utility of prophylaxis, these results are unusual. However, there are growing studies that question the role of post-traumatic prophylaxis [21, 22]. Bhullar et al. [15] in a recent study highlighted the suppression of functional recovery after seizure prophylaxis. Our findings underline the need for reconsideration of the role of seizure prophylaxis in general and specifically re-explorations of the role of levetiracetam prophylaxis.
Findings of our study should be interpreted in light of its limitations. Due to retrospective nature of the study, all potential confounders cannot be accounted for by propensity score matching. Seizures were identified mostly by clinical observation with EEGs performed as indicated. Routine EEGs were not performed during the study period, which may have led to systematic underreporting of seizure. We did not differentiate between type of seizure, and EEG confirmation was generally not employed, therefore our seizure rate may underestimate the true incidence of early post-traumatic seizures. There were no prophylaxis guidelines in place during the study period, and all three drugs were used for seizure prophylaxis, with the preference to a particular agent being based on the treating physician’s discretion. It is therefore possible that selection bias on the part of the treating clinicians was introduced based on the severity and/or type of their injuries, which may not have been accounted for by our propensity scoring. This remains a possible unmeasured confounder, but this was constant during the study period. In our center, from 2010 onward, we have implemented the prophylaxis guidelines. However, our seizure rate continues to be low, similar to the rate prior to the implementation of these guidelines. Despite these limitations, our study provides an important piece of evidence in the management of post-traumatic seizures.
Conclusion
In this propensity score-matched cohort analysis, levetiracetam prophylaxis did not show a significant difference in preventing seizures, as the rate of seizures was the same whether patients did or did not receive the drug. The overall incidence of post-traumatic seizures in patients with severe TBI was only 2 % in this study; therefore, we question the benefit of routine prophylactic anticonvulsant therapy in preventing early seizures in severe TBI patients. Since prophylaxis for post-TBI seizures remains the standard of care, an appropriately randomized controlled trial is warranted to clarify whether levetiracetam therapy is effective.
References
Centers for Disease Control and Prevention, National Center for Injury Prevention and Control: “Traumatic Brain Injury”. http://www.cdc.gov/TraumaticBrainInjury/index.html
Temkin NR (2009) Preventing and treating posttraumatic seizures: the human experience. Epilepsia 50(Suppl 2):10–13
Szaflarski JP, Sangha KS, Lindsell CJ, Shutter LA (2010) Prospective, randomized, single-blinded comparative trial of intravenous levetiracetam versus phenytoin for seizure prophylaxis. Neurocrit Care 12:165–172
Stratton SC, Large CH, Cox B, Davies G, Hagan RM (2003) Effects of lamotrigine and levetiracetam on seizure development in a rat amygdala kindling model. Epilepsy Res 53:95–106
Temkin NR, Dikmen SS, Wilensky AJ, Keihm J, Chabal S, Winn HR (1990) A randomized, double-blind study of phenytoin for the prevention of post-traumatic seizures. The New England Journal of Medicine 323:497–502
Brain Trauma F (2007) American Association of Neurological S, Congress of Neurological S. Guidelines for the management of severe traumatic brain injury. J Neurotrauma 24(Suppl 1):S1–S106
McQueen JK, Blackwood DH, Harris P, Kalbag RM, Johnson AL (1983) Low risk of late post-traumatic seizures following severe head injury: implications for clinical trials of prophylaxis. J Neurol Neurosurg Psychiatry 46:899–904
Frend V, Chetty M (2007) Dosing and therapeutic monitoring of phenytoin in young adults after neurotrauma: are current practices relevant? Clin Neuropharmacol 30:362–369
Haltiner AM, Newell DW, Temkin NR, Dikmen SS, Winn HR (1999) Side effects and mortality associated with use of phenytoin for early posttraumatic seizure prophylaxis. J Neurosurg 91:588–592
Cotton BA, Kao LS, Kozar R, Holcomb JB (2011) Cost-utility analysis of levetiracetam and phenytoin for posttraumatic seizure prophylaxis. J Trauma 71:375–379
Pieracci FM, Moore EE, Beauchamp K et al (2012) A cost-minimization analysis of phenytoin versus levetiracetam for early seizure pharmacoprophylaxis after traumatic brain injury. J Trauma Acute Care Surg 72:276–281
Jones KE, Puccio AM, Harshman KJ et al (2008) Levetiracetam versus phenytoin for seizure prophylaxis in severe traumatic brain injury. Neurosurg Focus 25:E3
Kruer RM, Harris LH, Goodwin H et al (2013) Changing trends in the use of seizure prophylaxis after traumatic brain injury: a shift from phenytoin to levetiracetam. J Crit Care 28(883):e9–e13
Inaba K, Menaker J, Branco BC et al (2013) A prospective multicenter comparison of levetiracetam versus phenytoin for early posttraumatic seizure prophylaxis. J Trauma Acute Care Surg 74:766–771 discussion 71-3
Bhullar IS, Johnson D, Paul JP, Kerwin AJ, Tepas JJ 3rd, Frykberg ER (2014) More harm than good: antiseizure prophylaxis after traumatic brain injury does not decrease seizure rates but may inhibit functional recovery. J Trauma Acute Care Surg 76:54–60
Annegers JF, Coan SP (2000) The risks of epilepsy after traumatic brain injury. Seizure J Br Epilepsy Assoc 9:453–457
Caballero GC, Hughes DW, Maxwell PR, Green K, Gamboa CD, Barthol CA (2013) Retrospective analysis of levetiracetam compared to phenytoin for seizure prophylaxis in adults with traumatic brain injury. Hosp Pharm 48:757–761
Temkin NR (2003) Risk factors for posttraumatic seizures in adults. Epilepsia 44(Suppl 10):18–20
Oluwole OS (2011) Incidence and risk factors of early post-traumatic seizures in Nigerians. Brain Inj 25:980–988
Liesemer K, Bratton SL, Zebrack CM, Brockmeyer D, Statler KD (2011) Early post-traumatic seizures in moderate to severe pediatric traumatic brain injury: rates, risk factors, and clinical features. J Neurotrauma 28:755–762
Young B, Rapp RP, Norton JA, Haack D, Tibbs PA, Bean JR (1983) Failure of prophylactically administered phenytoin to prevent late posttraumatic seizures. J Neurosurg 58:236–241
Young KD, Okada PJ, Sokolove PE et al (2004) A randomized, double-blinded, placebo-controlled trial of phenytoin for the prevention of early posttraumatic seizures in children with moderate to severe blunt head injury. Ann Emerg Med 43:435–446
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zangbar, B., Khalil, M., Gruessner, A. et al. Levetiracetam Prophylaxis for Post-traumatic Brain Injury Seizures is Ineffective: A Propensity Score Analysis. World J Surg 40, 2667–2672 (2016). https://doi.org/10.1007/s00268-016-3606-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3606-y