Abstract
Aims
To review and compare the outcomes of laparoscopic (LA) versus open appendicectomy (OA) in complicated appendicitis in adult patients, eight years after the last literature review.
Methods
The PRISMA guidelines were adhered to. Pre-defined inclusion and exclusion criteria were used to search the PubMed, Scopus and Cochrane databases and extract relevant data. Methodological and quality assessment was undertaken with outcome meta-analysis and subgroup analyses of methodological quality, type of study and year of study. Assessment of clinical and statistical heterogeneity and publication bias was conducted.
Results
Three randomised control trials (RCTs) (154LA vs 155OA) and 23 case–control trials were included (2034LA vs 2096OA). Methodological quality was low to average but with low statistical heterogeneity. Risk of publication bias was low, and meta-regression indicated shorter length of hospital stay (LOS) in more recent studies, Q = 7.1, P = 0.007. In the combined analysis LA had significantly less surgical site infections [OR = 0.30 (0.22,0.40); p < 0.00001] with reduced time to oral intake [WMD = -0.98 (-1.09,-0.86); P < 0.00001] and LOS [WMD = -3.49(-3.70,-3.29); p < 0.00001]. There was no significant difference in intra-abdominal abscess rates [OR = 1.11(0.85,1.45); p = 0.43]. Operative time was longer during LA [WMD = 10.51 (5.14,15.87); p = 0.0001] but did not reach statistical significance (p = 0.13) in the RCT subgroup analysis.
Conclusions
LA appears to have significant benefits with improved morbidity compared to OA in complicated appendicitis (level of evidence II).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute appendicitis remains one of the most common emergency pathologies, with a cumulative life time incidence of 9% [1]. Its reported incidence has increased over the last few decades, potentially due to the increased use of CT imaging, with the rate of complicated appendicitis representing a stable 25% of all cases [2]. Over the last three decades with the advent of laparoscopic surgery and the more widespread use of laparoscopy, complicated appendicitis (CA) defined as gangrenous or perforated appendicitis with or without peritonitis has been increasingly managed laparoscopically, with up to 67% of cases of CA performed laparoscopically in 2011 in the USA [3]. Laparoscopic practice has been widely adopted by surgeons as they have become more experienced in laparoscopy, in order for patients to benefit from the potential advantages of a minimally invasive procedure, such as reduced wound infection rates and ileus with earlier convalescence and potentially reduced future adhesional complications [4].
Some concerns have been raised in the past though in relation to a potential higher rate of intra-abdominal abscesses (IAA) in the laparoscopic group compared to the open group. A previous systematic review (SR) and meta-analysis (MA) failed to find a difference between the two groups in relation to IAA indicating some benefits in favour of the laparoscopic approach [4]. That evidence though was based on a number of case-controlled (CCTs) studies which were troubled by a number of methodological and external validity problems leading to a low overall level of evidence and recommendation indicating no difference between the two approaches. Since then a number of randomised controlled trials (RCTs), as well as additional CCTs reporting potentially beyond the laparoscopic learning curve, have been published on the subject. Our aim was therefore to perform an update of the previous review and meta-analysis in order to determine whether there is any significant difference between the laparoscopic and open approach in this group of patients in relation to their outcomes and establish the strength and level of existing evidence.
Methods
This study was undertaken according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)[5].
Eligibility criteria
All RCTs and CCTs comparing emergency laparoscopic (LA) versus open appendicectomy (OA) in adult patients (age >16) with CA were included. CA was defined as histologically or intra-operatively diagnosed perforated appendix with or without free or localised pus or gangrenous appendix. Patients with an appendix mass were excluded. Studies were included if reporting on any of the following outcomes: mortality, intra-abdominal abscess (IAA), surgical site infection (SSI), ileus, duration of operation and length of hospital stay (LOS). Additional exclusion criteria included duplicate publications where the most up-to-date and complete publication was included and publications reporting data from large administrative databases without any reporting of baseline characteristic comparison between groups or laparoscopic conversion rates. There were no language restrictions in relation to the database search.
Search and selection strategy
An electronic database search of the Cochrane Library’s Controlled Trials Registry and database of systematic reviews, Medline (1980–30 Apr 2016), PubMed, Scopus and Web of Knowledge databases was performed using pre-defined search terms (Supplementary Table 1) by two of the authors. Review of all titles, relevant abstracts and full-paper publications was performed selecting the studies adhering to the eligibility criteria. Back-referencing was also employed, and differences in relation to the inclusion or exclusion of a study were resolved with discussion.
Data abstraction and validity assessment
Data on methodological quality, baseline characteristics and independent variables, intervention characteristics and outcomes were collected on pre-designed data abstraction forms. Methodological assessment was performed using established methods from the Cochrane reviewer’s Handbook and risk of bias graded as low, intermediate or high.
Data analysis
Meta-analysis of outcomes was undertaken using the RevMan 5.3 statistical package from the Cochrane collaboration. A pre-requisite for inclusion of a dichotomous outcome in the meta-analysis was the report of sufficient data to form 2 × 2 contingency tables. Estimates of mean and standard deviation were calculated in studies reporting continuous variables in the form of median and range.
The Mantel–Haenszel statistical method providing OR with 95% CI and the weighted mean difference (WMD) methods were used to analyse dichotomous and continuous data, respectively. A fixed or random effects model was employed depending on the methodological quality, degree of statistical heterogeneity and size of the studies. Chi-square and I2 statistical tests were employed to assess statistical heterogeneity, and funnel plots graphical representation was performed to assess publication bias. Type of study (RCT vs. CCT), methodological quality (high vs. low) and time period of reported cases in relation to the establishment of laparoscopic surgery subgroup analyses were undertaken. Meta-regression was performed for the outcomes (surgical site infection, intra-abdominal abscess, length of procedure and length of stay) reported individually in more than ten studies. The random effects model was used to explore possible causes of heterogeneity such as year of publication, quality of the study (low, intermediate and high) and country of origin (Europe, Asia, America). Finally, the level of evidence and grade of recommendation reported were based on the Oxford Centre of Evidence-Based Medicine guidelines.
Results
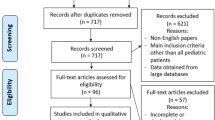
The search and selection results are illustrated in Fig. 1. Three RCTs [6,7,8] (154LA vs 155OA patients) published over the last five years and 23 CCTs (2034LA vs 2096OA patients) published since 1999 were selected (Table 1). All of the RCTs [6,7,8] and 12 of the CCTs [9,10,11,12,13,14,15,16,17,18,19,20] have been published since the last SR MA publication in 2010. One of the excluded studies that had been included in the previous meta-analysis was the study by Guller et al. [21] as this was a report from a large national database without reporting of additional independent variables that may significantly affect the outcomes. The great majority of included studies were undertaken in developed/industrialised countries, with the majority of patients having their surgery within the last 10 years (Table 1).
Definition of CA varied slightly among studies in terms of its precise definition, with seven studies mostly undertaken earlier chronologically including gangrenous CA in addition to perforation and/or purulent peritonitis and/or abscess formation in their diagnosis (Table 2). The diagnosis was performed intra-operatively in most studies, with only 50% of studies confirming the diagnosis histologically. IAA outcome definition was better defined in more recent studies as a radiological or intra-operative diagnosis of a collection and SSI definitions were defined as evidence of wound infection (erythema ± pus) requiring antibiotic or surgical treatment but with no reporting of microbiological wound culture results.
Independent variables such as patients’ age and gender were reported in the great majority of studies and statistically compared between groups, while American Society of Anaesthesiology (ASA) scores were only reported in a minority of cases and body mass index (BMI) is reported in only two of the most recent studies. The mean age among groups appears to vary from 23 to 57 years old with standard deviation values extending to a potential younger age of 12 (Ferranti et al.) [14]. Two studies reported a statistically significant younger age for their laparoscopic groups [10, 11] with Galli et al. [11] also reporting statistically higher ASA grades in the OA group.
The laparoscopic surgical experience was not reported in 8 studies, while the remaining studies reported both types of surgery being performed by experienced open and laparoscopic surgeons, even though the degree of experience is not specifically defined in the majority (Table 2). Laparoscopic conversion rates to open surgery varied from 20 to 45% in studies reporting data on patients operated on before 2000, while studies reporting on patients undergoing surgery in the third millennium report conversion rates of 0 to 18%, with the exception of one study that reported a high conversion rate of 41% [11] with no reported laparoscopic surgical experience (Table 1).
The operative procedures themselves are quite homogeneous between studies (Table 2). Various heat sources are used for mesoappendix division, and endoloops are mainly used for appendicular ligation, with retrieval bags employed in the extraction of the surgical specimen from the abdomen. Most open procedures are performed via a McBurney incision or a lower abdominal laparotomy, with only one study reporting on the use of a wound protector [7]. Fourteen of the studies do not report on their wound closure technique, while four studies selectively allow wounds to heal by secondary intention in OA [8, 20, 22, 23]. Clinically appropriate antibiotic regimes appear to be used peri-operatively and post-operatively and continued on the basis of clinical indication. A standardised post-operative care pathway is not reported in any of the studies.
Methodological quality
The methodological quality and risk of bias assessment of the studies is shown in Table 3. The risk of bias within the studies ranged from intermediate to high among studies. This was mainly because of factors such as absence of observer blinding and statistical power calculations in RCTs, inadequate reporting or statistical testing of significant independent variables that may have influenced the outcomes and insufficient reporting of peri-operative care and its standardisation, all potentially influencing internal and external validity.
Diagnosis of CA and peri-operative management of the patients though appeared to be quite homogeneous among studies in regard to surgical techniques and antibiotic prescribing, with reasonable external validity, and thus, a decision was made to proceed with a meta-analysis of outcomes. Unless specifically reported per outcome, there was no evidence of publication bias on visual inspection of funnel plots. Stratification analysis during the meta-analysis did not reveale any differences between the various groups analysed apart from the analysis comparing the RCT against the CCT groups were on some occasions the RCT subgroup found no difference in some outcomes between LA and OA. This difference can potentially be attributed to the small number of patients included in the RCTs compared to the CCTs. Meta-regression analysis showed that part of the heterogeneity in the length of stay could be explained by the year of publication of each study Q = 7.1, P = 0.007.
Mortality
A great majority of studies [6,7,8,9,10,11,12, 14, 17,18,19, 22,23,24,25,26,27,28,29] report on this outcome. Overall LA was found to have a significantly lower mortality rate compared to OA [OR = 0.14(0.04,0.51); P = 0.003], with no statistical heterogeneity (I2 = 0%). Two studies mainly contributed positive data to the meta-analysis of this outcome reporting high mortality rates in the OA groups, 5% reported by Galli et al.[11] and 11% by Stoltzing et al.[24], versus 0% in the LA group. Both studies had a significantly high laparoscopic conversion rate of over 40% and subsequently failed to use intention to treat analysis; thus, mortality in the LA groups is potentially underreported. Furthermore, one of the studies [11] reported a significantly higher ASA group in the OA group potentially introducing a selection bias in favour of LA. When these two studies are excluded from the MA, there is no difference in mortality between LA and OA.
Intra-abdominal abscess
Twenty-six studies [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20, 22,23,24,25,26,27,28, 30,31,32,33] reported on this outcome (Fig. 2). The mean rate of IAA was 8% in the LA and 6% in the OA group. There was not statistically significant difference between LA and OA in regard to the overall incidence of IAA [OR = 1.11(0.85, 1.45);P = 0.43], with minimal amount of statistical heterogeneity (I2 = 7%).
Surgical site infection
Three RCTs [7, 8, 15] and 21 CCTs [6, 9,10,11,12, 14, 16,17,18,19,20, 22,23,24,25,26,27,28, 31,32,33] reported on this outcome with the smaller number of RCTs finding no significant difference between the two techniques but with a statistically high degree of heterogeneity (I2 = 77%) (Fig. 3). Overall the incidence of SSI was 6.7 and 17.7% in the LA and OA groups, respectively, with a statistically significant lower rate in the LA group compared to the OA group [OR = 0.30 (0.22,0.40); P < 0.00001], with a moderate degree of statistical heterogeneity (I2 = 37%).
Operative duration
The three RCTs [7, 8, 15] reporting on this outcome found a nearly significant (P = 0.13) longer operative time in the LA group of 12 min with a high degree of statistical heterogeneity (I2 = 84%) (Fig. 4). Taking into account all types of studies [6, 9,10,11,12, 16, 17, 19, 22, 30, 32, 33], the LA procedure lasted an average of 10.5 min longer than the OA [WMD = 10.51(5.14,15.87);P = 0.0001] with a similarly high degree of statistical heterogeneity (I2 = 89%).
Ileus and time to oral intake
The rate of ileus was only reported by one RCT [7] and 6 CCTs [6, 9, 10, 16, 24, 28], and there was no difference [OR = 0.98(0.51,1.86); P = 0.94], between the two groups, with no statistical heterogeneity. Time to oral intake was reported by one RCT and 7 CCTs and was statistically faster [WMD = −0.98(−1.09,−0.86);P < 0.00001] in the LA group with no statistical heterogeneity.
Length of stay
All of the RCTs [7, 8, 15] and 12 of the CCTs [6, 9,10,11,12, 16, 17, 19, 22, 30, 32, 33] reported on this outcome (Fig. 5). There was no significant difference found among the RCTs (P = 0.42), but meta-analysis of all types of studies revealed a significantly shorter hospital stay in favour of the LA group [WMD = −2.27(−3.44,−1.09);P = 0.0002]. Both subgroup and overall meta-analyses carried a significant risk of statistical heterogeneity.
Discussion
This systematic review and meta-analysis has been performed 8 years after the last review and meta-analysis on the topic. The number of additional studies performed, including three RCTs, is an indicator of the sustained importance of this topic as well as a positive move towards obtaining higher-quality evidence.
The quality of more recent studies appears to have improved, but findings should still be considered with caution in view of the described methodological deficiencies. These include the lack of use of intention to treat analysis in seven of the included studies, with converted LA cases and their outcomes treated as belonging to the OA group. Current findings reinforce previous results supporting LA as the procedure of choice for CA versus OA, with a reduced rate of SSIs, faster recovery and no difference in the rate of IAA, supported by an increasing number of RCTs and CCTs. The reduction in conversion rates demonstrated in the more recent studies (0–18%) compared to previously published studies (20–45%) is an indirect indicator of the improved laparoscopic skills of surgeons demonstrating an achievement of a laparoscopic learning curve plateau, in agreement with recent literature reports [3, 34, 35].
In terms of individual outcomes, the diagnostic criteria for IAA were fairly well reported in the studies and independent variables that could have affected the incidence of IAA such as the surgical technique and use of antibiotics were well reported. Duration of antibiotic treatment, however, was mainly a clinical decision with no actual parameters provided to guide external validity. Similarly the lack of strict outcome definition for SSI may have influenced the reporting of this outcome explaining some of the degree of statistical heterogeneity observed, even though the reported average difference in the incidence of this complication between the two groups of 6.7% (LA) and 17.7% (OA) is potentially too big to be just attributed to observer bias.
Despite a similar rate of surgical ileus, patients undergoing LA appear to be able to commence oral diet faster, which together with the reduced morbidity observed in this group potentially contributes to the finding of a shorter hospital stay. The latter outcome as in the previous MA was not very clearly defined as total or post-operative length of stay. The risk of clinical heterogeneity is therefore plausible, as it may be directly influenced by the pre-operative time to surgery depending on the diagnostic pathways and availability of theatre resources and expertise. One would expect though that in the current age, these independent variables would not differ between the LA and OA group in the healthcare systems of developed countries where most of the included studies have originated from.
A number of studies reporting on data from national or multicentre administrative databases on the reviewed subject were also identified by this review process. These were not included for this meta-analysis because of the potentially high risk of significant methodological bias such as risk of selection bias, performance bias in the absence of technique description, operator experience and peri-operative care description as well as risk of reporting bias. The huge numbers of patients included in these studies though cannot be completely ignored. Their main findings are described in Table 4[3, 34, 36,37,38,39], with the great majority supporting the findings of this review and meta-analysis.
The outcomes reported in this review were mainly around the short-term post-operative period. Long-term outcomes such as risk of hernias and the risk of adhesional small bowel obstruction (SBO) have not been investigated in this study. Markar et al. [40] recently contacted a systematic review and meta-analysis to investigate the incidence of SBO following LA and OA defined by the need for re-operation to resolve SBO. Their analysis for patients with CA included 42 thousand patients in a mixture of 14 studies, comprising of RCTs, CCTs as well as big database reports and included both adult and paediatric populations. Despite the inherent risk of bias and lack of methodological assessment of the selected studies, the findings overwhelming suggested that LA has a lower risk of SBO when compared to OA both in the short- and long-term post-operative period.
The benefits of LA in CA may be of even greater benefit in high-risk patient groups. Greater than 90% of patients included in this group of studies though had an ASA score of I and II, when this was reported, with BMI values rarely reported. Masoomi et al. [34] using data on 14 thousand patients derived from a large national database demonstrated through a multivariate regression analysis that LA has significant benefits in obese patients (BMI >30) when compared to OA. A similar finding was reported for patients with ASA scores of III and IV [41], even though this study suffered from some methodological weaknesses affecting its results [42]. Additional potential benefits of LA not captured in this meta-analysis directly linked to the faster convalescence seen in LA are the earlier return to normal daily activities and employment. Furthermore, the significant reduction in morbidity and a shorter length of hospital stay can offset the hospital costs of the laparoscopic equipment and slightly longer operative time [34]. Even though a direct cost-effectiveness analysis has not been undertaken in this review, all of these factors can potentially make LA financially more advantageous than OA in this group of patients. Regardless, the relevant cost-effectiveness of the procedure should be considered within the context of the local healthcare system.
Despite the systematic and statistical measures taken to increase its methodological rigour and improve and measure heterogeneity among included studies, this review and meta-analysis comes with a number of inherent limitations. These are directly linked to the methodological quality of the included studies. As such results should be considered per outcome for external validity as well as assessed against the potential risk of a type I or II error.
Overall, this meta-analysis has shown a higher level of evidence (level II) increasingly supporting LA as the procedure of choice in CA versus OA. LA appears to have a similar rate of IAA to OA, but with lower rates of SSI, earlier return to oral diet and reduced length of hospital stay.
References
Anderson JE, Bickler SW, Chang DC et al (2012) Examining a common disease with unknown etiology: trends in epidemiology and surgical management of appendicitis in California, 1995–2009. World J Surg 36:2787–2794
Buckius MT, McGrath B, Monk J et al (2012) Changing epidemiology of acute appendicitis in the United States: study period 1993–2008. J Surg Res 175:185–190
Masoomi H, Nguyen NT, Dolich MO et al (2014) Laparoscopic Appendectomy Trends and Outcomes in the United States: data from the Nationwide Inpatient Sample (NIS), 2004‐2011. Am Surg 80:1074–1077
Markides G, Subar D, Riyad K (2010) Laparoscopic versus open appendectomy in adults with complicated appendicitis: systematic review and meta-analysis. World J Surg 34:2026–2040
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151:264–269
Quezada F, Quezada N, Mejia R et al (2015) Laparoscopic versus open approach in the management of appendicitis complicated exclusively with peritonitis: a single center experience. Int J Surg 13:80–83
Taguchi Y, Komatsu S, Sakamoto E et al (2016) Laparoscopic versus open surgery for complicated appendicitis in adults: a randomized controlled trial. Surg Endosc 30:1705–1712
Thomson J-E, Kruger D, Jann-Kruger C et al (2015) Laparoscopic versus open surgery for complicated appendicitis: a randomized controlled trial to prove safety. Surg Endosc 29:2027–2032
Yeom S, Kim MS, Park S et al (2014) Comparison of the outcomes of laparoscopic and open approaches in the treatment of periappendiceal abscess diagnosed by radiologic investigation. J Laparoendosc Adv Surg Tech 24:762–769
Dimitriou I, Reckmann B, Nephuth O et al (2013) Single institution’s experience in laparoscopic appendectomy as a suitable therapy for complicated appendicitis. Langen Arch Surg 398:147–152
Galli R, Banz V, Fenner H et al (2013) Laparoscopic approach in perforated appendicitis: increased incidence of surgical site infection? Surg Endosc 27:2928–2933
Mohamed AA, Mahran KM (2013) Laparoscopic appendectomy in complicated appendicitis: is it safe? J Minim Access Surg 9:55
Wilson DG, Bond AK, Ladwa N et al (2013) Intra-abdominal collections following laparoscopic versus open appendicectomy: an experience of 516 consecutive cases at a district general hospital. Surg Endosc 27:2351–2356
Ferranti F, Corona F, Siani L et al (2012) Laparoscopic versus open appendectomy for the treatment of complicated appendicitis. G Chir 33:263–267
Schietroma M, Piccione F, Carlei F et al (2012) Peritonitis from perforated appendicitis: stress response after laparoscopic or open treatment. Am Surg 78:582–590
Lim SG, Ahn EJ, Kim SY et al (2011) A clinical comparison of laparoscopic versus open appendectomy for complicated appendicitis. J Korean Soc Coloproctol 27:293–297
Garg CP, Vaidya BB, Chengalath MM (2009) Efficacy of laparoscopy in complicated appendicitis. Int J Surg 7:250–252
Kehagias I, Karamanakos SN, Panagiotopoulos S et al (2008) Laparoscopic versus open appendectomy: which way to go. World J Gastroenterol 14:4909–4914
Park H-C, Yang D-H, Lee B-H (2009) The laparoscopic approach for perforated appendicitis, including cases complicated by abscess formation. J Laparoendosc Adv Surg Tech 19:727–730
Sleem R, Fisher S, Gestring M et al (2009) Perforated appendicitis: is early laparoscopic appendectomy appropriate? Surgery 146:731–738
Guller U, Hervey S, Purves H et al (2004) Laparoscopic versus open appendectomy. Ann Surg 239:43–52
So JB, Chiong E-C, Chiong E et al (2002) Laparoscopic appendectomy for perforated appendicitis. World J Surg 26:1485–1488
Kirshtein B, Bayme M, Domchik S et al (2007) Complicated appendicitis: laparoscopic or conventional surgery? World J Surg 31:744–749
Stöltzing H, Thon K (2001) Perforated appendicitis: is laparoscopic operation advisable? Dig Surg 17:610–616
Piksun G, Kozic D, Rajpal S et al (2001) Comparison of laparoscopic, open and converted appendectomy for perforated appendicitis. Surg Endosc 15:660–662
Fukami Y, Hasegawa H, Sakamoto E et al (2007) Value of laparoscopic appendectomy in perforated appendicitis. World J Surg 31:93–97
Yau KK, Siu WT, Tang CN et al (2007) Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg 205:60–65
Pokala N, Sadhasivam S, Kiran RP et al (2007) Complicated appendicitis—is the laparoscopic approach appropriate? A comparative study with the open approach: outcome in a community hospital setting. Am Surg 73:737–742
Kim H, Lee I, Lee Y et al (2009) A comparative study on the short-term clinicopathologic outcomes of laparoscopic surgery versus conventional open surgery for transverse colon cancer. Surg Endosc 23:1812–1817
Khalili TM, Hiatt JR, Savar A et al (1999) Perforated appendicitis is not a contraindication to laparoscopy. Am Surg 65:965–967
Wullstein C, Barkhausen S, Gross E (2001) Results of laparoscopic vs. conventional appendectomy in complicated appendicitis. Dis Colon Rectum 44:1700–1705
Lin H-F, Wu J-M, Tseng L-M et al (2006) Laparoscopic versus open appendectomy for perforated appendicitis. J Gastrointest Surg 10:906–910
Katsuno G, Nagakari K, Yoshikawa S et al (2009) Laparoscopic appendicectomy for complicated appendicitis: a comparison with open appendicectomy. World J Surg 33:208–214
Masoomi H, Nguyen NT, Dolich MO et al (2011) Comparison of laparoscopic versus open appendectomy for acute nonperforated and perforated appendicitis in the obese population. Am J Surg 202:733–739
Ukai T, Shikata S, Takeda H et al (2016) Evidence of surgical outcomes fluctuates over time: results from a cumulative meta-analysis of laparoscopic versus open appendectomy for acute appendicitis. BMC Gastroenterol 16:1–12
Masoomi H, Mills S, Dolich M et al (2012) Comparison of outcomes of laparoscopic versus open appendectomy in children: data from the Nationwide Inpatient Sample (NIS), 2006–2008. World J Surg 36:573–578
Tiwari MM, Reynoso JF, Tsang AW et al (2011) Comparison of outcomes of laparoscopic and open appendectomy in management of uncomplicated and complicated appendicitis. Ann Surg 254:927–932
Tuggle KR-M, Ortega G, Bolorunduro OB et al (2010) Laparoscopic versus open appendectomy in complicated appendicitis: a review of the NSQIP database. J Surg Res 163:225–228
Yeh C, Wu S, Liao C et al (2011) Laparoscopic appendectomy for acute appendicitis is more favorable for patients with comorbidities, the elderly, and those with complicated appendicitis: a nationwide population-based study. Surg Endosc 25:2932–2942
Markar SR, Penna M AH (2014) Laparoscopic approach to appendectomy reduces the incidence of short- and long-term post-operative bowel obstruction: systematic review and pooled analysis. J Gastrointest Surg 18:1683–1692
Werkgartner G, Cerwenka H, El Shabrawi A et al (2015) Laparoscopic versus open appendectomy for complicated appendicitis in high risk patients. Int J Colorectal Dis 30:397–401
Bulian DR (2015) Invited commentary on” Werkgartner G. et al.: laparoscopic versus open appendectomy for complicated appendicitis in high risk patients”. Int J Colorectal Dis 30:567
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
There are no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Athanasiou, C., Lockwood, S. & Markides, G.A. Systematic Review and Meta-Analysis of Laparoscopic Versus Open Appendicectomy in Adults with Complicated Appendicitis: an Update of the Literature. World J Surg 41, 3083–3099 (2017). https://doi.org/10.1007/s00268-017-4123-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4123-3