Abstract
Background
Laparoscopic distal pancreatectomy (LDP) has been shown to have short-term benefits over open distal pancreatectomy (ODP). Its application for pancreatic ductal adenocarcinoma (PDAC) remains controversial.
Methods
From 1995 to 2014, 72 patients underwent distal pancreatectomy for PDAC at a single institution and were included in the study. Postoperative and long-term outcomes of patients undergoing LDP (n = 44) or ODP (n = 28) were compared.
Results
LDP was associated with less blood loss (332 vs. 874 mL, p = 0.0012) and lower transfusion rates than ODP (18.2 vs. 50 %, p = 0.0495). Operative time was similar (254 vs. 266 min) for LDP and ODP; five patients (11.4 %) required conversion to ODP. Pancreatic fistulas (13.6 vs. 7.1 %) and major complications (13.6 vs. 25 %), were similar between LDP and ODP, respectively. Length of hospital stay (5.1 vs. 9.4 days, p = 0.0001) and time to initiate adjuvant therapy (69.4 vs. 95.6 days, p = 0.0441) was shorter for LDP than ODP. Tumor characteristics were similar but LDP was associated with more resected lymph nodes than ODP (25.9 vs. 12.7, p = 0.0001). One-, three-, and five-year survival rates were similar between LDP (69, 41, and 41 %, respectively) and ODP (78, 44, and 32 %, respectively).
Conclusion
LDP is associated with less blood loss and need for blood transfusion, shorter hospital stay, and faster time to initiate adjuvant therapy than ODP for patients with PDAC. Postoperative outcomes and long-term survival are similar between the two groups. LDP appears to be safe in the treatment of patients with PDAC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic distal pancreatectomy (LDP) has been shown [1–8] to have significant advantages over open distal pancreatectomy (ODP). Many large, single institutional or multi-institutional studies have demonstrated the safety and feasibility of this approach for malignant indications [9–13]. However, some still question its appropriateness for pancreatic adenocarcinoma (PDAC) [14]. A recent meta-analysis of LDP for PDAC showed less blood loss, shorter hospital stay, longer operative times, and smaller tumor size than for ODP for PDAC [15]. Oncologic outcomes, such as margin status and lymph node harvest, as well as pancreatic fistula rate, morbidity, mortality, and administration of adjuvant therapy were similar. However, the overall number of patients analyzed in this study was small and only surrogate markers of oncologic equivalence were analyzed. Similarly, a study using the National Cancer Data Base to examine the outcomes of LDP for PDAC over a two-year time period demonstrated similar advantages over ODP without compromising perioperative oncologic outcomes [16].
Prognosis from PDAC is notoriously poor, even after complete surgical resection. Therefore, surgeons must closely evaluate each intervention to ensure that both quality and quantity of each patient’s survival is not deleteriously affected. Additionally, in studies of adjuvant therapy for pancreatic adenocarcinoma, up to 38 % of patients are not able to complete full adjuvant therapy regiments, at least in part due to the effects of surgical morbidities [17]. Surgical techniques that help reduce morbidity may help increase the proportion of patients completing therapy and thus may have some beneficial effect on survival. It is clear that LDP has short-term advantages over ODP. However, reports regarding long-term survival outcomes that compare LDP to ODP for PDAC are scarce and underpowered. This study was performed to compare short- and long-term outcomes of LDP and ODP for PDAC at a single institution over a 20-year time period.
Materials and methods
Information was collected on all patients undergoing pancreatic resection from January 1995 to December 2014. This study used an institutional review board (IRB)-approved prospective database. The data points that were collected from the database included demographics, operative variables, postoperative outcomes, pathologic findings, and extended follow-up. Preoperative characteristics included age, sex, comorbidities, body mass index (BMI), American Society of Anesthesiologists (ASA) score, and the use of neoadjuvant treatments. Operative details included operative time (incision to close of the wound), estimated blood loss (EBL), and blood product transfusion obtained from the anesthesia record. Use of laparoscopy, type of distal pancreatectomy, vascular resection, and concomitant resections were also recorded.
Postoperative outcomes were tracked for 3 months (90 days) after surgery and were graded according to the Clavien system [18]. A final overall patient complication grade was given to the highest-rated complication grade experienced by patients in the group. Clinically significant complications (morbidity) were defined as grade III-V complications. Pancreatic fistula (PF) [19] and post-pancreatectomy hemorrhage (PPH) [20] were scored and graded according to standard international consensus definitions. Length of stay (LOS) was recorded and was defined as postoperative day 1 through day of discharge. Readmission to any hospital was defined as any unplanned admission and was tracked for all patients through 90 days after surgery. Reoperation was defined as any unplanned operation within 90 days of the primary pancreatic resection. Final pathologic details were recorded and included margin status and lymph node harvest. Positive margins were considered positive if microscopic (R1) or macroscopic (R2) disease was noted at the surface of any surgical margin. There was no use of separate diagnostic laparoscopy with peritoneal cytology or intraoperative peritoneal cytology in this study. Adjuvant therapy (chemotherapy and/or radiation) is administered as indicated to all eligible patients at a time frame of 4–8 weeks postoperatively. Adjuvant therapy data were collected retrospectively from our institution as well as outside facilities in which the therapy was administered for patients who received treatment elsewhere.
Patients included in the study were those patients with PDAC undergoing consecutive distal pancreatectomy for curative intent during the study time period. Those patients with the finding of unresectable metastatic peritoneal disease at the time of the index operation were excluded from analysis. This finding is rare as the routine use of high quality magnetic resonance imaging and endoscopic ultrasound by a dedicated HPB team is performed for all patients. NCCN guidelines were used to determine resectability based on these studies. Distal pancreatectomy for PDAC was approached by open technique for the first 15 years of the study with only one exception and approached by laparoscopic technique during the last five years of the study with only two exceptions due to the arrival of a minimally invasive HPB surgeon at the end of 2008 (H.A.) and the addition of another in 2011 (J.S.) who was trained at our institution and therefore, LDP was performed in the same manner by both surgeons as previously described [21]. Parenchymal transection was performed by stapled transection in the large majority of ODP and LDP. However, since 2008, LDP parenchymal transection has been performed using a slow compression technique with staple line reinforcement.
Categorical data are reported as number with percentage of the whole with significance tested by 2-tailed Fisher’s exact test. Continuous data are reported as a mean with range with significance tested by a t test. Survival analysis was performed using Kaplan–Meier estimated survival. Analyses were completed in an intention-to-treat manner.
Results
All patients
During the study time period, 351 patients underwent distal pancreatectomy. Of these, 72 patients underwent distal pancreatectomy for curative intent for the diagnosis of pancreatic ductal adenocarcinoma. Open distal pancreatectomy (ODP) was performed in 28 patients, while laparoscopic distal pancreatectomy (LDP) was performed in 44 patients.
The demographics of the patients are shown in Table 1, and the majority of patients in both groups had at least one major comorbidity. The patients undergoing LDP were older, but the patients were otherwise well matched between the two groups.
The hand-assisted method was used in four patients (9.1 %) from the LDP group, while the conversion to open surgery was necessary in five (11.4 %) patients from this group (Table 2). Conversion to open surgery was performed when multivisceral resection could not be completed laparoscopically (n = 2), when there was extensive tumor involvement near the celiac trunk (n = 1), when there was recurrent positive pancreatic margins (n = 1), and for control of hemorrhage (n = 1).
Regarding operative variables (Table 2), LDP compared with ODP was associated with significantly less blood loss [332 vs. 884 mL (p = 0.0012)] and intraoperative blood transfusion [18.2 vs. 50 % (p = 0.0495)]. A multivisceral resection was required in 32.1 and 38.6 % (p = 0.6229) of patients undergoing ODP and LDP, respectively, and most commonly included partial gastrectomy, colectomy, or left adrenalectomy. Vascular resections included portal vein or hepatic arterial resections, and their incidences were very similar between groups, occurring in approximately 7 % of patients in each group.
Ninety-day postoperative complication rates (Table 2) were largely similar between the two groups. Postoperative monitoring in the intensive care setting was needed much less frequently in the LDP patient group (16 %) compared with those undergoing ODP (44 %) (p = 0.0150). Morbidity and readmission rates were also lower for LDP but did not reach statistical significance. Length of stay was significantly shorter for the LDP group (5.1 days) versus the ODP group (9.4 days) (p = 0.0001). One patient experienced both the single postoperative hemorrhage and mortality in the LDP group. This patient had variant hepatic artery anatomy with subsequent injury eventually resulting in hepatic infarction, pancreatic fistula, and hemorrhage eventually resulting in multiorgan dysfunction and death. The one patient that required reoperation experienced an abdominal fascial dehiscence at the specimen extraction site resulting in the need for wound exploration and fascial closure.
Pathological examination (Table 3) revealed that tumor size, T-stage, and N-stage were well matched between the two groups. LDP was associated with a significantly higher number of harvested lymph nodes compared with ODP [25.9 vs. 12.7, respectively (p = 0.0001)]. LDP was also associated with a smaller tumor size, higher rate of negative margins, and lower lymph node ratio (LNR), but these differences did not reach statistical significance. Neoadjuvant therapy was used prior to ODP and LDP in one and two patients, respectively. Three-fourths of patients in both groups underwent treatment with adjuvant chemotherapy, but the LDP group was able to initiate treatment within a significantly shorter time period after surgery 69.4 vs. 95.6 days, respectively (p = 0.0441).
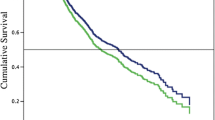
Survival
Kaplan–Meier estimated survival analysis (Table 4) revealed similar overall and stage matched survival for the two groups at all points through 5 years. There was no statistical difference in overall survival between LDP and ODP for all stages (p = 0.851) or when matched by stage (Fig. 1). The estimated median overall survival is 26.4 and 26.6 months for ODP and LDP, respectively. Only 1 patient in the ODP group was lost to follow-up.
Discussion
Over the past decade, the safety and feasibility of laparoscopic pancreatic surgery has been proven by many surgeons and institutions around the world. Furthermore, advantages of the laparoscopic approach have been clearly reported for distal pancreatectomy [1–8, 15]. Gagner et al. reported the first LDP for malignancy in 1996 [22], and since then, multiple series have been published that included small subsets of patients undergoing LDP for PDAC, with data on short-term oncologic outcomes [23]. In a series of distal pancreatectomies for PDAC reported in 2013, the authors compared 28 robotic and LDP to 34 ODP and found less blood loss and shorter length of stay but similar oncologic outcomes for the minimally invasive group [12]. Just recently, a group from Korea reported a propensity score-matched comparative analysis of two groups of 51 patients each undergoing LDP or ODP for PDAC and found a shorter hospital stay for LDP but similar postoperative outcomes and overall survival between the two groups [13].
LDP has become an accepted method for dealing with all pathologies of the neck, body, and tail of the pancreas. In the past, the adoption of LDP in the United States had been relatively low, but the rate appears to be increasing [24, 25]. Despite mounting evidence and increasing popularity, some authors still question the appropriateness of LDP for the treatment of malignancy and call for randomized studies to evaluate its effectiveness [14]. This series represents one of the largest experiences regarding LDP for PDAC published to date and demonstrates that there is no oncologic rationale for withholding the possible benefits of LDP from patients who require operative resection for PDAC in the distal pancreas.
Our experience is unique in that there was a clear and definitive change in the approach to PDAC of the distal pancreas from an open fashion to a minimally invasive fashion with the arrival of the senior author in August 2008. Prior to this, all but one patient underwent ODP. After 2008, all distal pancreatectomies were preferentially approached by a minimally invasive fashion, and only 2 patients underwent ODP after 2008. The first patient underwent ODP due to the need for portal vein resection, and the second patient underwent ODP by a low volume non-pancreatic surgeon. This provided a relatively non-biased comparison between the ODP and LDP groups, which were free of selection bias. The patients were very well matched with regard to demographics, comorbidities, and pathologic staging; similar to the group who utilized a propensity score-matching method [13].
Patients undergoing LDP experienced the expected advantages over ODP and had decreased blood loss and less need for intraoperative blood transfusions, and these results were similar to those that we and others have previously published regarding LDP versus ODP [9, 12, 26]. A review of recent literature clearly indicates that perioperative blood transfusions have been repeatedly associated with a poor long-term prognosis after resection of pancreatic cancer [27]. Unfortunately despite this improvement with LDP, long-term survival was not significantly impacted in this study. Perhaps future studies with sufficient patients will allow for this attribute to positively impact survival after LDP for PDAC, but there are numerous other factors that also affect survival.
We were also able to demonstrate significantly increased lymph node retrieval with the use of LDP compared with ODP in our series. Previously, we reported a non-significant increase in lymph node retrieval for patients undergoing LDP for PDAC and pancreatic neuroendocrine tumors [9]. While this translated into a lower LNR for the patients undergoing LDP in this current study, this did not reach statistical significance. A decreased LNR has been shown to have prognostic significance for patients undergoing pancreatic resection for PDAC in a single institutional series of 905 patients [28], and it was seen in a Surveillance, Epidemiology, and End Results (SEER) database study [29]. It is unlikely that resection of additional peripancreatic lymph nodes will truly impact the prognosis of a patient undergoing pancreatic resection for PDAC. However, we believe this data demonstrates the ability to ensure a wide en bloc resection of the body and tail of the pancreas afforded and even facilitated by the laparoscopic approach.
Correspondingly, a negative margin (RO) was obtained in a higher percentage of patients undergoing LDP than ODP (95.5 vs. 82.1 %, p = 0.1012). While this did not reach statistical significance, similar findings were identified by a recent National Cancer Data Base (NCDB) study that found that patients undergoing LDP had an increased rate of margin negative resections over ODP (87 vs. 78 %, p = 0.042) [16]. The lack of selection bias in our data seems to indicate that a “cleaner” and wider en bloc resection can be performed using a minimally invasive method. RO resection is known to have a significant impact on survival, and although it was not born out in our survival results possibly due to the small numbers of patients in our study, this higher rate of RO resection with LDP could certainly contribute to improved overall and disease-free survival in patients undergoing PDAC resection.
Our findings are similar to those reported in 2014 by Lee et al. This group described twelve patients undergoing minimally invasive, radical antegrade modular pancreatosplenectomy (RAMPS) for distal PDAC. Operative time, blood loss, transfusion rate, and overall complications reported were well within acceptable margins, and they were able to obtain a margin negative resection in all patients with an impressive 5-year disease-specific survival of 55.6 % [30]. While their series did not include patients undergoing en bloc gastric or colon resection, other groups have also demonstrated the ability of experienced surgeons to modify dissection planes to accomplish an oncologically appropriate resection even with contiguous organ involvement [13, 31].
The minimally invasive approach can also be advantageous for patients in whom a need for conversion to open resection will be very likely. In this “hybrid” approach, a laparoscopic mobilization of the tail of the pancreas and spleen allows for a smaller open incision, oftentimes by a midline incision which spares a large left subcostal incision for the patient. This is particularly true for larger and more central lesions or those that require a multivisceral or vascular resection.
Overall survival was very similar between those patients undergoing LDP and ODP and comparable to results previously published for LDP for PDAC [23]. Estimated three-year overall survival for LDP and ODP was 41 and 44 %, respectively. Currently, there are eight 5-year survivors from the ODP group and two 5-year survivors from the LDP group. The majority of patients in the LDP group have not reached this post-surgical time point yet because of the date of their initial surgery.
The limitations of this study included a relatively small sample size, but our study can be considered large in comparison to what is currently available in literature. Additionally, data regarding the use of adjuvant therapy (chemotherapy and radiotherapy) including the time periods, regiments, completion rate, tolerance, and reason for withholding adjuvant treatment was often absent due to the nature of referrals to our institution. A large majority of patients are from afar and do not receive adjuvant treatments within our institution since they are treated closer to their home, which makes long-term follow-up of these parameters more challenging. As these data were collected over the course of a 20-year time period, there were clearly changes and developments in technique and perioperative care that can account for some of the short-term and postoperative outcome improvements seen in this study. Surgical technique, perioperative anesthesia management, pathologic analysis, postoperative protocols, and comprehensive cancer management systems have undergone continuous progressive evolution in this time period. The overall treatment of PDAC is multifactorial and minimally invasive surgery is just one of the many tools that surgeons may utilize to lessen the impact of this disease on our patients.
Conclusion
This study is currently one of the largest single institutional series to report LDP for PDAC and shows that this approach does not compromise survival. In fact, LDP improves RO resection rate and LNR and leads to a more immediate initiation of adjuvant chemotherapy after surgery, which may impact survival if analyzed in a larger number of patients. One of the advantages of this study is the lack of selection bias, a clear change in practice from open to laparoscopic at a particular time period, and a standardized laparoscopic technique by two experienced MIS pancreas surgeons.
Ultimately, overall survival was not affected by the laparoscopic approach in this study despite the improvement in surrogate oncologic markers and may need larger studies to detect any differences. Nevertheless, LDP has been shown to have clear perioperative and short-term advantages over OPD and does not appear to pose any oncologic disadvantages. The outcomes of patients treated at our institution in the study time period provides evidence that the laparoscopic approach is safe and may be responsible for improved short-term outcomes. However, a multi-institutional study comparing the MIS and open approaches in a contemporaneous group of patients may be of benefit to validate these outcomes.
Abbreviations
- DP:
-
Distal pancreatectomy
- ODP:
-
Open distal pancreatectomy
- LDP:
-
Laparoscopic distal pancreatectomy
- BMI:
-
Body mass index
- ASA:
-
American Society of Anesthesiologists
- EBL:
-
Estimated blood loss
- PF:
-
Pancreatic fistula
- PPH:
-
Post-pancreatectomy hemorrhage
- LOS:
-
Length of stay
References
Venkat R, Edil BH, Schulick RD, Lidor AO, Makary MA, Wolfgang CL (2012) Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique: a systematic review and meta-analysis. Ann Surg 255(6):1048–1059
Nakamura M, Nakashima H (2013) Laparoscopic distal pancreatectomy and pancreatoduodenectomy: is it worthwhile? A meta-analysis of laparoscopic pancreatectomy. J Hepatobiliary Pancreat Sci 20(4):421–428
Sui CJ, Li B, Yang JM, Wang SJ, Zhou YM (2012) Laparoscopic versus open distal pancreatectomy: a meta-analysis. Asian J Surg 35(1):1–8
Jin T, Altaf K, Xiong JJ et al (2012) A systematic review and meta-analysis of studies comparing laparoscopic and open distal pancreatectomy. HPB 14(11):711–724
Jusoh AC, Ammori BJ (2012) Laparoscopic versus open distal pancreatectomy: a systematic review of comparative studies. Surg Endosc 26(4):904–913
Xie K, Zhu YP, Xu XW, Chen K, Yan JF, Mou YP (2012) Laparoscopic distal pancreatectomy is as safe and feasible as open procedure: a meta-analysis. World J Gastroenterol 18(16):1959–1967
Pericleous S, Middleton N, McKay SC, Bowers KA, Hutchins RR (2012) Systematic review and meta-analysis of case-matched studies comparing open and laparoscopic distal pancreatectomy: is it a safe procedure? Pancreas 41(7):993–1000
Nigri GR, Rosman AS, Petrucciani N et al (2011) Metaanalysis of trials comparing minimally invasive and open distal pancreatectomies. Surg Endosc 25(5):1642–1651
Stauffer JA, Rosales-Velderrain A, Goldberg RF, Bowers SP, Asbun HJ (2013) Comparison of open with laparoscopic distal pancreatectomy: a single institution’s transition over a 7-year period. HPB 15(2):149–155
Lee SY, Allen PJ, Sadot E et al (2015) Distal pancreatectomy: a single institution’s experience in open, laparoscopic, and robotic approaches. J Am Coll Surg 220(1):18–27
Kooby DA, Hawkins WG, Schmidt CM et al (2010) A multicenter analysis of distal pancreatectomy for adenocarcinoma: is laparoscopic resection appropriate? J Am Coll Surg. 210(5):779–787
Magge D, Gooding W, Choudry H et al (2013) Comparative effectiveness of minimally invasive and open distal pancreatectomy for ductal adenocarcinoma. JAMA Surg 148(6):525–531
Shin SH, Kim SC, Song KB et al (2015) A comparative study of laparoscopic vs. open distal pancreatectomy for left-sided ductal adenocarcinoma: a propensity score-matched analysis. J Am Coll Surg 220(2):177–185
Mehrabi A, Hafezi M, Arvin J et al (2015) A systematic review and meta-analysis of laparoscopic versus open distal pancreatectomy for benign and malignant lesions of the pancreas: it’s time to randomize. Surgery 157(1):45–55
Ricci C, Casadei R, Taffurelli G et al (2015) Laparoscopic versus open distal pancreatectomy for ductal adenocarcinoma: a systematic review and meta-analysis. J Gastrointest Surg 19(4):770–781
Sharpe SM, Talamonti MS, Wang E et al (2015) The laparoscopic approach to distal pancreatectomy for ductal adenocarcinoma results in shorter lengths of stay without compromising oncologic outcomes. Am J Surg 209(3):557–563
Oettle H, Neuhaus P, Hochhaus A et al (2013) Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA 310(14):1473–1481
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Bassi C, Dervenis C, Butturini G et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138(1):8–13
Wente MN, Veit JA, Bassi C et al (2007) Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 142(1):20–25
Asbun HJ, Stauffer JA (2011) Laparoscopic approach to distal and subtotal pancreatectomy: a clockwise technique. Surg Endosc 25(8):2643–2649
Gagner M, Pomp A, Herrera MF (1996) Early experience with laparoscopic resections of islet cell tumors. Surgery 120(6):1051–1054
Bjornsson B, Sandstrom P (2014) Laparoscopic distal pancreatectomy for adenocarcinoma of the pancreas. World J Gastroenterol 20(37):13402–13411
Rosales-Velderrain A, Bowers SP, Goldberg RF et al (2012) National trends in resection of the distal pancreas. World J Gastroenterol 18(32):4342–4349
Tran Cao HS, Lopez N, Chang DC et al (2014) Improved perioperative outcomes with minimally invasive distal pancreatectomy: results from a population-based analysis. JAMA Surg 149(3):237–243
Jayaraman S, Gonen M, Brennan MF et al (2010) Laparoscopic distal pancreatectomy: evolution of a technique at a single institution. J Am Coll Surg 211(4):503–509
Benson D, Barnett CC Jr (2011) Perioperative blood transfusions promote pancreas cancer progression. J Surg Res 166(2):275–279
Pawlik TM, Gleisner AL, Cameron JL et al (2007) Prognostic relevance of lymph node ratio following pancreaticoduodenectomy for pancreatic cancer. Surgery 141(5):610–618
Slidell MB, Chang DC, Cameron JL et al (2008) Impact of total lymph node count and lymph node ratio on staging and survival after pancreatectomy for pancreatic adenocarcinoma: a large, population-based analysis. Ann Surg Oncol 15(1):165–174
Lee SH, Kang CM, Hwang HK, Choi SH, Lee WJ, Chi HS (2014) Minimally invasive RAMPS in well-selected left-sided pancreatic cancer within Yonsei criteria: long-term (>median 3 years) oncologic outcomes. Surg Endosc 28(10):2848–2855
Kang CM, Lee SH, Lee WJ (2014) Minimally invasive radical pancreatectomy for left-sided pancreatic cancer: current status and future perspectives. World J Gastroenterol 20(9):2343–2351
Acknowledgments
The authors would like to acknowledge Mauricia Buchanan for her assistance in collecting data for the purpose of this study and Zhou Li with the statistical analysis with support from the Mayo Clinic in Florida Focused Research Team Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Stauffer, Dr. Coppola, Dr. Mody, and Dr. Asbun report no biomedical financial interests or potential conflict of interest.
Rights and permissions
About this article
Cite this article
Stauffer, J.A., Coppola, A., Mody, K. et al. Laparoscopic Versus Open Distal Pancreatectomy for Pancreatic Adenocarcinoma. World J Surg 40, 1477–1484 (2016). https://doi.org/10.1007/s00268-016-3412-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3412-6