Abstract
We have previously demonstrated that, although most papillary thyroid microcarcinomas (PMC) do not grow or grow only slowly, cases showing lateral node metastasis diagnosed by ultrasonography (US) show an aggressive characteristic associated with poor disease-free survival. In this study, we focused on two prominent US features: tumor, edge definition and strong echoes. We investigated whether these findings reflect aggressive characteristics of PMC in a series of 155 cases. Poor edge definition was observed in 21.5% of patients, all of who showed worse disease-free survival (p = 0.0477) than those with a well-defined edge. Furthermore, this finding was directly linked to US-diagnosed lateral node metastasis (p = 0.0001). Strong echoes were observed in 63.9% of the cases, and fine strong echoes were seen in 25.2%. Cases demonstrating fine strong echoes tended to frequently show recurrence (p = 0.0902), and this finding was also significantly linked to US-diagnosed lateral node metastasis (p = 0.0494). These findings suggest that an ill-defined tumor edge is an important US feature of biologically aggressive PMC. We should carefully follow such patients, regardless of the therapeutic strategy, observation, or surgical treatment chosen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Papillary carcinoma is the most common histological type of malignancy originating in the thyroid. This tumor generally displays slow growth and shows a good prognosis if competently resected. Recent establishment of the technique of ultrasonography (US)-guided fine-needle aspiration biopsy (FNAB) has facilitated detection and diagnosis, even of small papillary carcinoma measuring 10 mm or less in maximal diameter. Such tumor are defined as papillary microcarcinoma (PMC), according to the World Health Organization (WHO) [1]. To date, there have been two therapeutic options for PMC. One is thyroidectomy with lymph node dissection; similar to larger papillary carcinoma lesions, PMC has been associated with lymph node metastasis as well as multiple tumor formation (intrathyroidal metastasis) in high incidences [2–5]. Another therapeutic option is observation without immediate surgical treatment [6]. Observation has been proposed based on autopsy findings that PMC is frequently found to be a harmless occult carcinoma [7–9]. To date, we have applied this therapy option to cases without any of the following unfavorable features: (1) tumors located adjacent to the trachea, (2) tumors possibly invading the recurrent laryngeal nerve, (3) FNAB findings suggesting high-grade malignancy, (4) lymph nodes highly suggestive of metastasis (or confirmed as metastatic by FNAB). Uncomplicated PMC detected by US generally have been found to grows slowly or not at all. [6]. For both diagnosis and evaluation of the-biological characteristics of PMC, US is the most useful tool.
We recently demonstrated that patients with PMC demonstrating lymph node metastasis in the lateral compartment on preoperative US examination have significantly worse disease-free survival (DFS), even if therapeutic modified radical neck dissection (MRND) is performed [10]. These results suggest that US-diagnosed (but not pathologically confirmed) lateral metastasis predicts a poor prognosis in PMC patients and that preoperative US evaluation of lateral node metastasis is one of the most important factors in selecting the appropriate surgical treatment [10, 11].
We then studied the relationships between US findings of the primary tumors and US-diagnosed lateral node metastasis. Tumors with multiple intrathyroidal metastasis and/or that occupy the upper region of the thyroid on US examination more frequently demonstrated US-diagnosed lateral node metastasis [11]. These findings suggest that, for such cases, evaluation of lateral node metastasis on US should be carefully performed. In addition, when observation is the treatment chosen for patients without US-diagnosed lateral metastasis, such observation should proceed with particular care because lateral metastasis may be more likely to develop.
Since around 2000, the accuracy of US has increased, making it possible to obtain more information about the tumors, as revealed by the status of the border and charactoristic of the internal echoes. However, little is known about whether and how the US features of PMC reflect biologically aggressive phenotypes. In this study, we therefore focused on two representative US features of the tumor, edge definition and strong echoes. As the first step in the study, we investigated the relationships between these findings and DFS of patients, as well as US-diagnosed lateral node metastasis, a known characteristic that definitely indicates the biological aggressiveness of PMC [10, 11].
Patients and Methods
Patients
When we find micronodules suggestive of malignancy by such US findings as low echoic signals and a jagged border, we perform FNAB to diagnose the micronodules as benign or malignant. We do not routinely perform FNAB for micronodules without such features. The positive predictive value of FNAB is around 99% for papillary carcinoma, as previously described [6].
This study enrolled 155 patients, who were diagnosed as having PMC by FNAB and who underwent surgery in our hospital between October 1999 and August 2001. Before surgical treatment, all patients underwent US to evaluate the form, location, and number of tumors and the presence of lymph node metastasis. On the basis of these findings, the surgeon determined the range of thyroidectomy and lymph node dissection. For US examination in our hospital, an ultrasonic real-time electronic scanner (Aloka SSD-5500, Tokyo, Japan) and a search unit of the mechanical sector model of 10 MHz and 13 MHz have been used since 1999. All patients in the present series were examined using this equipment. In addition all cases were pathologically confirmed as papillary carcinoma after surgery.
Based on the records of US findings and photographs, two examiners (Y. I. and K. K.) reviewed whether the tumor edge was ill-defined or well-defined and whether strong echoes, if present, were fine or coarse in each case. The term “fine strong echoes” indicates multiple dot-like high echoic spots (microcalcification), whereas “coarse strong echoes” indicates apparently detectable calcification in nodules with acoustic shadow. In the cases of multiple lesions, we judged the lesions as ill-defined and/or having fine strong echoes, when at least one of the tumors demonstrated these findings.
We considered nodes metastatic when the US findings met the criteria proposed by Antonelli et al. [12]: (1) diameter of 1 cm or greater;(2) clear hypoechoic pattern or dyshomogeneous pattern, with alternating hypoechoic and hyperechoic areas; (3) irregular cystic appearance; (4) presence of internal calcification; (5) rounded or bulging shape with increased antero-posterior diameter; and (6) shorter/longer diameter ratio greater than 0.7. Twenty patients, who were diagnosed as having lateral node metastasis on preoperative US examination, underwent therapeutic modified radial neck dissection (MRND). Of the remaining 135 patients without US-diagnosed lateral metastasis, 43 underwent prophylactic MRND, and the remaining 92 underwent central node dissection only.
Postoperative Follow-up
After surgical treatment, we followed the patients by US and chest roentogenogram to determine whether local recurrence or distant metastasis had developed. Follow-up periods averaged 37.3 ± 11.1 months (range: 2–58 months). To date, three patients have shown recurrence in the remnant thyroid or lymph node. One patient with ill-defined edge and coarse strong echoes demonstrated lung metastasis at surgery, and was omitted from the analysis of DFS. This patient remains alive after 131I ablation following total thyroidectomy with MRND. To date, distant metastases have not been detected postoperatively in any patient, and none of the patients have died of papillary carcinoma.
Statistical Analyses
Fisher’s exact test was used to compare the clinicopathological variables. The Kaplan-Meier method was adopted to evaluate DFS of the patients. A p value < 0.05 was regarded as significant, and p values between 0.05 and 0.1 was regarded as indicating borderline significance.
Results
US-diagnosed Lateral Node Metatasis
Of the 155 PMCs, lateral node metastasis was detected by preoperative US examination in 20 cases (Fig. 1-a). Table 1 demonstrates the accuracy of US-diagnosed lateral metastasis by comparing pathological findings for 63 patients undergoing therapeutic or prophylactic MRND. Of the 20 cases showing US-diagnosed lateral metastasis, all but two were confirmed as having metastasis by postoperative pathological examination, and the positive predictive value reached 90%. However, US could not detect metastasis in 14 of 32 cases with pathologically confirmed lateral node metastasis, indicating that the sensitivity was only 56.3%. Furthermore, of 43 cases without US-diagnosed lateral node metastasis, 14 (32.6%) had pathologically confirmed metastasis. These incidences are similar to those reported in our previous study, which reported a larger series [11].
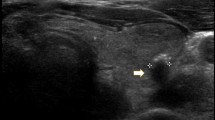
1-a. Ultrasound (US) photograph of a metastatic node in the lateral compartment. 1-b. US photograph of a papillary thyroid microcarcinoma (PMC) with an ill-defined edge and fine strong echoes. 1-c. US photograph of a PMC with a well-defined edge. 1-d. US photograph of a PMC with coarse strong echoes. We could not determine edge definition in this case.
Edge Definition
Of the 155 PMC cases the present in series, we could not determine edge definition in 11 cases because of the wide range of acoustic shadows from large and coarse high echoes. These 11 cases were therefore omitted from this analysis. Of the 144 informative cases, edges in 31 (21.5%) were classified as ill-defined and those in the remaining 113 (78.5%) as well-defined (Fig. 1-b, 1-c; Table 1). Figure 2 indicates the DFS of patients with ill-defined and well-defined edges, Patients with an ill-defined edge had a higher incidence of recurrence than those with a well-defined edge (p = 0.0477).
Of the 31 US studies showing an ill-defined edge, lateral node metastasis was detected by preoperative US examination in 13 (41.9%), while such metastasis was found only in 4 of 113 cases showing a well-defined edge (3.7%) (Table 2). There was a significant difference between the two diagnoses (p < 0.0001).
Strong Echoes
Of the 155 cases in this series, fine strong echoes were detected in 39 (25.2%), while 60 (38.7%) demonstrated coarse strong echoes (Fig. 1-c, 1-d). There were no strong echoes found in the remaining 56 cases (36.1%). We compared the DFS of patients showing fine strong echoes with that of those showing coarse or no strong echoes (Fig. 3). Patients with fine strong echoes tended to show recurrence more frequently than those with coarse or no strong echoes (p = 0.0902).
Table 3 shows the relationship between the presence of strong echoes and US-diagnosed lateral metastasis. Cases showing fine strong echoes more frequently showed US-diagnosed lateral metastasis (p = 0.0494). There was no significant difference in the rate of US-diagnosed lateral metastasis between cases showing coarse strong echoes and those without strong echoes.
Discussion
To date, several groups have studied the US findings of thyroid carcinoma. Chang et al. reported that papillary carcinoma lesions manifested as well-limited, heterogeneous, and hypoechoic nodules, and that cystic degenerations and/or discrete particles could be present [13]. Thereafter, Khoo et al. reported that the risk of malignancy is high when calcification is noted within a solitary nodule [14]. Koike et al. analyzed US findings for a large number of thyroid nodules and showed that the malignancy of nonfollicular neoplasms can be predicted on US by analyzing five US features: margin, shape, US structure, echogenecity, and calcification [15]. According to Chan et al., US findings in papillary carcinoma demonstrate a broad spectrum, and US features atypical of papillary carcinoma can be seen in half of all lesions [16]. To date, however, there have not been any studies focusing on the US features of PMC.
To our knowledge, this is the first study investing the US features of PMC tumors. This is because, before 1999, the lack of accuracy in US findings precluded investigation of the US features of tumors in detail. We found an ill-defined edge in 21.5% of PMC, and such cases showed a worse DPS rate than those with a well-defined edge, although the follow-up period remains rather short, 37.3 months on average. This finding indicates that ill-defined edge reflects the aggressive character of PMC. Furthermore, tumors with an ill-defined edge more frequently demonstrated US-diagnosed lateral node metastasis. This finding does not provide direct evidence that an ill-defined edge is a marker of the aggressiveness of PMC, but, because US-diagnosed lateral metastasis is a strong indicator of worse DFS, an ill-defined edge may indirectly indicate that such tumors tend to be biologically aggressive. Furthermore, for cases managed by observation without immediate surgical treatment, careful US evaluation to screen for metastasis is required at every follow-up to determine whether to proceed to surgery. It is important to consider that US-diagnosed lateral metastasis may be more likely to occur in patients with PMC with an ill-defined edge.
Koike et al. demonstrated that ill-defined margin could be observed in 56.1% of nonfollicular malignant nodules [15]. Chan et al. also reported a similar incidence of this feature, 53%, in papillary carcinoma [16]. The incidences were greater than that presented in this study, perhaps because their series included all sizes of tumors. Because tumor size is one of the prognostic factors of papillary carcinoma [17], it seems reasonable that the incidence of ill-defined edge in PMC would be lower than that reported in larger tumors.
Fine strong echoes were observed in 25.2% of our US studies, which is similar to the incidence reported in a previous study of nonfollicular malignant nodules but less frequent than that in another study of papillary carcinoma [15, 16]. This phenomenon is thought to historically represent psammoma bodies, small crystalline calcific deposits in the epithelium [18, 19]. This type of strong echo signal can be observed not only in primary tumors but also in metastatic nodes [20] Although the significance of fine strong echoes has not been confirmed, this pattern of strong echoes is accepted as a radiological sign of papillary carcinoma. By comparison coarse strong echoes mostly correlate with amorphous and dense calcifications and have less diagnostic value [13]. The clinical, as well as physiological significance of fine strong echoes remains to be clarified.
Previous studies demonstrated that the prognosis of the diffuse sclerosing variant of papillary carcinoma with abundant psammoma bodies does not significantly differ from that of the more common type [21, 22]. In PMC, the DFS rates of patients with tumors showing fine strong echoes tended to be worse, but the difference did not reach significance. Therefore, we can not accurately assess whether fine strong echoes can be considered a marker of aggressive character of PMC. Neverthless, because we have found that tumors with fine strong echoes are more likely to be associated with US-diagnosed lateral metastasis, careful US evaluation for node metastasis is an essential aspect of patient management when observation has been chosen as the treatment plan.
In summary, we have demonstrated that, in PMC, the presence of an ill-defined tumor edge may be a marker of aggressive characteristics. Also, fine strong echoes, may potentially reflect the biological aggressiveness of a lesion. Further studies over a longer follow-up are necessary to determine with greater certainty the clinical significance of this finding in PMC.
References
Hedinger C, Williams ED, Sobin LH. Histological Typing of Thyroid Tumors, volume 11, Berlin, Springer-Verlag, 1988
Iida F, Sugenoya A, Muramatsu A. Clinical and pathologic properties of small differentiated carcinomas of the thyroid gland. World J. Surg. 1991;15:511–515
Hay ID, Grant CS, van Heerden JA, et al. Papillary thyroid microcarcinoma: a study of 535 cases observed in a 50-year period. Surgery 1992;112:1139–1147
Rodriguez JM, Moreno A, Parrila P, et al. Papillary thyroid microcarcinoma: clinical study and prognosis. Eur. J. Surg. 1997;163:255–259
Rassael H, Thompson LDR, Heffess CS. A rationale for conservative management of microscopic papillary carcinoma of the thyroid gland: a clinicopathological correlation of 90 cases. Eur. Arch. Otorhinolaryngol. 1998;255:462–467
Ito Y, Uruno R, Nakano K, et al. An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid Thyroid 2003;13:381–388
Harach HR, Franssila KO, Wasenius VM. Occult papillary carcinoma of the thyroid: a “normal” finding in Finland. A systematic autopsy study. Cancer 1985;56:531–538
Fukunaga FH, Yatani R. Geographic pathology of occult thyroid carcinomas. Cancer 1975;36:1095–1099
Lang W, Borrusch G, Bauer L. Occult carcinomas of the thyroid. Am. J. Clin. Pathol. 1988;90:72–76
Ito Y, Tomoda C, Uruno T, et al. Preoperative ultrasonographic examination for lymph node metastasis is useful when designing lymph node dissection for papillary microcarcinoma. World J. Surg. 2004;28:498–501
Ito Y, Tomoda C, Uruno T, et al. Papillary microcarcinoma of the thyroid: how should it be treated? World J. Surg. 2004; 28: 1115–1121
Antonelli A, Miccoli P, Ferdeghini M, et al. Role of neck ultrasonography in follow-up of patients operated on for differentiated thyroid cancer. Thyroid 1995;5: 25–29
Chang TC, Hong CT, Chang SL, et al. Correlation between sonography and pathology in thyroid diseases. J. Formosan Med. Assoc. 1990;89:777–783
Khoo MLC, Asa SL, Witterick IJ, et al. Thyroid calcification and its association with thyroid carcinoma. Head Neck 2002;24:651–655
Koike E, Noguchi S, Yamashita H, et al. Ultrasonographic characteristics of thyroid nodules. Arch. Surg. 2001;136:334–337
Chan BK, Desser TS, McDougall IR, et al. Common and uncommon sonographic features of papillary thyroid carcinoma. J. Ultrasound Med. 2003;22:1083–1090
Schindler AM, van Melle G, Evequoz B, et al. Prognostic factors in papillary carcinoma of the thyroid. Cancer 1991;68:324–330
Takashima S, Fukuda H, Nomura N, et al. Thyroid nodules: re-evaluation with ultrasound. J. Clin. Ultrasound 1995;23:179–185
Klinck GH, Winship T. Psammoma bodies and thyroid cancer. Cancer 1959;12:656–662
Ahuja AT, Chow L, Chick W, et al. Metastatic cervical nodes in papillary carcinoma of the thyroid: ultrasound and histological correlation. Clin. Radiol. 1995;43:121–124
Fujimoto Y, Obara T, Ito Y, et al. Diffuse sclerosing variant of papillary carcinoma of the thyroid. Clinical importance, surgical treatment, and follow-up study. Cancer 1990;66:2306–2312
Schoroder S, Bay V, Dumke K, et al. Diffuse sclerosing variant of papillary thyroid carcinoma. S-100 protein immunocytochemistry and prognosis. Virchows Arch. A. Pathol. Anat. Histopathol. 1990;416:367–371
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ito, Y., Kobayashi, K., Tomoda, C. et al. Ill-defined Edge on Ultrasonographic Examination Can Be a Marker of Aggressive Characteristic of Papillary Thyroid Microcarcinoma. World J. Surg. 29, 1007–1011 (2005). https://doi.org/10.1007/s00268-005-7834-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-7834-9