Abstract
Background
Critical appraisal of safety, feasibility, and economic impact of thyroidectomy procedures using local (LA) or general anesthesia (GA) is performed.
Methods
Consecutive patients undergoing thyroidectomy procedures were selected from a prospective database from January 1996 to June 2003 of a single-surgeon practice at a tertiary center. Statistical analyses determined differences in patient characteristics, outcomes, operative data, and length of stay (LOS) between groups. A cohort of consecutive patients treated in 2002–2003 by all endocrine surgeons at the institution was selected for cost analysis.
Results
A total of 1,194 patients underwent thyroidectomy, the majority using LA (n = 939) and outpatient surgery (65%). Female gender (76%), body mass index ≥30 kg/m2 (29%), median age (49 years), and cancer diagnosis (45%) were similar between groups. Extent of thyroidectomy (59% total) and concomitant parathyroidectomy (13%) were similarly performed. GA was more commonly utilized for patients with comorbidity [15% vs. 10%, Anesthesia Society of America (ASA) ≥3; P < 0.001], symptomatic goiter (13% vs. 7%; P = 0.004), reoperative cases (10% vs. 6%; P = 0.01), and concomitant lymphadenectomy procedures (15% vs. 3%; P < 0.001). GA was associated with significant increase in LOS ≥24 hours (17 % vs. 4%) or overnight observation (49 % vs. 14%), P < 0.001. Operative room utilization was significantly associated with type of anesthesia (180 min vs. 120 min, GA vs. LA, P < .001) and impacted to a lesser degree by surgeon operative time (89 minutes vs. 76 minutes, GA vs. LA; P = .089). Overall morbidity rates were similar between groups (GA 5.8 % vs. LA 3.2%). The actual total cost (ATC) per case for GA was 48% higher than for LA and 30% higher than the ATC for all procedures (P = 0.006), with the combined weighted average impacted by more LA cases (n = 217 vs. 85).
Conclusion
These data from a large, unselected group of thyroidectomy patients suggest LA results in similar outcomes and morbidity rates to GA. It is likely that associated LA costs are lower.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
We previously reported the safety and feasibility of thyroidectomy using local anesthesia (LA) in 1,025 patients and established its utility in a wide range of patients considered for a vast array of thyroid procedures.1 LA procedures were accomplished in patients with high comorbidity scores (10%) and those requiring more extensive or complex resections with overall low associated morbidity. Same-day discharge was achieved in 80% of patients and in 96% by 23 hours. Intuitively, one might anticipate several advantages to thyroidectomy performed using LA when compared with conventional general anesthesia (GA) with regard to length of hospital stay, operating room utilization, cost containment, patient selection, and voice monitoring. Since thyroidectomy using LA is uncommonly utilized by contemporary endocrine surgeons,2–10 studies directly comparing this method to conventional GA are lacking. Published comparative studies are impacted by small cohort size and stringent patient selection bias with limited or no comparative cost data available.5,9 Cost analyses for thyroidectomy procedures performed in the USA have been limited to studies of outpatient surgery that have addressed results using GA methods only.11–14 Furthermore, since overall operative morbidity, specifically recurrent nerve injury, is low for thyroidectomy procedures, a large cohort of unselected patients is needed to determine potential advantages of thyroidectomy performed with voice monitoring in an awake patient, a unique feature of thyroidectomy using LA, which distinguishes this method from a GA approach.15,16
This study was conducted to compare thyroidectomy performed using LA to standard, conventional GA in a large number of unselected patients with outcome measures including patient characteristics, operative data, morbidity, length of stay (LOS), and cost. Clinically meaningful differences in the types of patients, procedures, and outcomes associated with each thyroidectomy approach are described.
MATERIALS AND METHODS
Patient Selection and Type of Anesthesia
Consecutive patients undergoing thyroidectomy procedures at Columbia University Medical Center by a single surgeon (PL) from January 1996 to June 2003 were selected for study. During this period, LA was routinely offered to all eligible patients undergoing thyroidectomy. Patients with known extensive substernal, retrotracheal/esophageal goiter, locally advanced or regional thyroid cancer, documented recurrent nerve dysfunction, allergy to LA, language barrier, or inability to communicate with the operating team were not eligible for a local procedure. Local thyroidectomy procedures were accomplished using a regional, combined superficial and deep C2–C4 cervical block with lidocaine and bupivicaine LA with the patient under monitored intravenous sedation, as described in previous publications.1,17,18 Patients who did not choose or were not eligible for LA technique underwent conventional thyroidectomy with GA and endotracheal intubation. A similar regional cervical block was performed on GA patients for intra- and perioperative pain control.
Thyroidectomy Procedures
A modified surgical approach with regard to incision placement and cervicotomy closure has been previously published in detail and was employed for all patients in this study, regardless of the anesthetic method.17,18 Modifications include a transverse incision placed high on the neck at the level of the cricoid cartilage, allowing access to the relatively fixed superior pole vessels. Cervicotomy closure involves interrupted approximation of strap muscles overlying the cricoid cartilage and leaving the lower strap muscles open for decompression should perioperative hematoma occur. A clear Collodion adhesive dressing placed on the skin incision facilitates sutureless, cosmetic closure and ability to easily monitor the wound in the postoperative period.16 In addition, vessels were hemostatically controlled with 2.0 and 3.0 silk ties. The recurrent laryngeal nerve (RLN) was identified in each case. Nerve monitoring involved phonation during LA thyroidectomy procedures. No specific nerve monitoring devices were used during thyroidectomy performed under GA.
Perioperative Patient Management
As a routine, all patients were monitored postoperatively in a recovery room setting for 6 hours. Perioperative procedures included nonnarcotic analgesia, calcium prophylaxis (± vitamin D therapy) in patients at risk for hypoparathyroidism, and patient education by specialized staff. Following a 6-hour recovery period, patients eligible for same-day surgery were evaluated by the surgeon for potential discharge. If all criteria were met, patients were discharged following the 6-hour observation period regardless of anesthesia method. Those who did not meet criteria or who required continued monitoring were admitted for a 23-hour observation or a longer hospital stay, as deemed necessary by the surgeon.15,16,19,20
Statistics and Cost Analysis
Data collection and review were conducted with approval from Columbia University Medical Center Institutional Review Board. Patient demographics, operative details, perioperative complications, and LOS data were collected and analyzed using descriptive statistics (SPSS, Version 10.0, Chicago, IL, USA). A comparative analysis was performed for patients grouped according to type of anesthesia (locoregional or general endotracheal) on an intent-to-treat basis. Significance was defined as a P value <0.05 based on Fisher’s exact test for discrete variables and Kruskal–Wallis test for continuous variables. LOS was divided into 3 categories: outpatient (6-hour observation), discharged by <24 hours, and discharged ≥24 hours.
A separate cohort of patients was selected for cost analysis. Patients undergoing consecutive thyroidectomy procedures at the New York Thyroid Center by surgeons with a focus in endocrine surgery during the years 2002–2003 were selected for further review. ATC data associated with each of the 302 consecutive cases were assembled using the hospital’s cost accounting support system. These data included both fixed and variable technical costs for each procedure: operating and recovery room, pharmacy, equipment, nursing, and room and board but not professional fees. Mann–Whitney test was used to compare the mean ATC and variance between patients undergoing thyroidectomy with LA and GA. Adjustments for possible factors such as extent of thyroidectomy procedure, LOS, and operating room time were made by combining P values across different levels of these factors, with significance defined as a P value <0.05.
RESULTS
Patient Characteristics and Operative Procedures
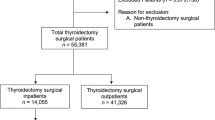
In this 8-year study, 1,194 patients underwent thyroidectomy procedures with the majority (n = 939/1194, 79%) performed using LA. Following initial safety and feasibility trials in a selected cohort of patients from 1987–1993,19,20 LA thyroidectomy eligibility criteria were broadened in 1996 to include nearly all patients presenting for thyroidectomy.1,15,16 This selection bias reflects the significant increase in the proportion of local procedures compared with general cases that occurred throughout the course of the study (Fig. 1).
Comparison of the number of consecutive thyroidectomy procedures performed from 1996–2003 by a single surgeon (PL) at the New York Thyroid Center using local or conventional general anesthesia (P < 0.001). Adapted with permission from Spanknebel et al. 1
Table 1 summarizes clinical features of patients undergoing the 2 operative approaches. Female gender (76%) and age (49.5 years; range 7–89) were similar between LA and GA groups and reflective of other large thyroidectomy series.21–26 In spite of broadened selection criteria, however, GA was more commonly utilized in patients with increased comorbidity, as described by higher Anesthesia Society of America (ASA) scores of 3 and 4 (16% vs. 11%, GA vs. LA, P < 0.001). Available data quantifying patient body habitus showed a similar proportion of obese patients in each of the patient groups (GA 54% and LA 46%, P = 0.10). A trend was noted, however, toward more malignant conditions addressed using LA (47% vs. 46%, P = 0.03). This was likely due to shifts in pathological diagnosis and patient selection rather than clinically meaningful differences related to technique.
Comparative analysis of operative data demonstrated important differences between LA and conventional thyroidectomy groups depicted in Table 2. Since patients with preoperatively identified substernal or retrotracheal/esophageal goiter were typically not offered the LA thyroidectomy, it is not surprising that more patients underwent extensive goiter resections using GA (13% vs. 7%, P = 0.004). Likewise, patients with known regional thyroid cancer requiring cervical lymphadenectomy procedures were more frequently handled using a conventional GA approach (15% vs. 3%, P < 0.001). Prior neck surgery was not a contraindication to LA thyroidectomy; however, more reoperative procedures were performed using GA (10% vs. 6%; P = 0.01). This was also the case for extensive bilateral procedures, including total and subtotal thyroidectomy, which were the types of procedures more commonly performed using GA (63% vs. 61%; P = 0.005). Concomitant parathyroidectomy was similarly performed using either approach in 13% of cases.
Outcomes: Operative Duration and Length of Stay
There were no demonstrable differences in surgeon operative time as measured from skin incision to closure, with a mean of 89 minutes for GA procedures (range 20–280) and 76 minutes for LA procedures (range 25–225), P = 0.09 (Table 2). A more clinically meaningful and accurate comparison of operating room utilization is expressed as overall operating room duration that also includes anesthesia time. These data were available for a smaller subset of cases performed during 2002–2003 and are reported within the context of cost analysis below (Table 3). In fact, GA cases were associated with significantly increased mean operating room times compared with LA cases (180 vs. 120 minutes, GA vs. LA, P < 0.001), most likely as a result of increased anesthesia time required for GA cases.
For the purposes of comparative analysis of discharge data, outpatient status was considered any hospital stay whereby patients were observed for 6 hours postoperatively and then discharged. Inpatient status was defined as any hospital stay more than 6 hours (23-hour overnight observation or hospital admission ≥24 hours). Figure 2A and B depict the trends in outpatient status during the course of the study for LA and GA patients, respectively. Within the context of a mature outpatient thyroidectomy program, both LA and GA patients enjoyed the possibility of shorter hospital stays. LA patients were more likely to receive short-stay procedures (P = 0.001), with 86% of patients discharged following 6-hour observation by the last 2 years of the study. (Figure 2A). In contrast, there were no particular trends noted for the GA group, where patients achieved outpatient status 0%–52% of the time on any given year during the 8 years of the study. (Figure 2B) Overall, significantly more LA patients were able to undergo short-stay procedures compared with the GA group (82% vs. 34%, P < 0.001).
Number of patients undergoing thyroidectomy each year as inpatient (≤24 hours or >24 hours) or outpatient (6-hour observation) procedures using local (LA) (A) or general (GA) (B) anesthesia. A. Outpatient status increased significantly throughout the duration of the study for LA thyroidectomy patients, P = 0.001 (n = 860). B. There were no significant trends in early discharge status noted for patients undergoing conventional GA thyroidectomy procedures (n = 222).
Operative Complications
A critical appraisal of the types of complications seen for each of the operative approaches was performed (Table 4). The crossover rate to a GA approach (attempted local cases that required conversion to GA) was low and did not significantly impact overall morbidity data (3.4%, n = 32). Reasons for conversion to GA are detailed in a previous publication.1 Combined morbidity rates were comparable between the 2 groups: 5.5% for GA patients and 3.2% for LA patients; P = 0.12. There were no deaths.
More specifically, low RLN injury rates were seen (as calculated per patient) and did not appear to be impacted by the thyroidectomy approach used. A diagnosis of RLN injury was secured by performing direct fiberoptic nasolaryngoscopy in patients with noted voice changes or voice complaints. Systematic vocal cord exam was not routinely performed postoperatively but was, rather, prompted by symptomatic patients only. Temporary and permanent RLN injury occurred in 1.6% (n = 4) and 0.8% (n = 2) of patients who underwent conventional thyroidectomy, respectively. Similar rates of temporary (1.7%, n = 16) and permanent (0.7%, n = 7) RLN injury occurred in local thyroidectomy procedures. There were more intentional nerve resections, though not statistically significant, due to locally advanced malignancy in the GA group, which is reflective of the types of cases selected for a conventional approach (1.6% vs. 0.3%; P = 0.20).
Four neck hematomas requiring intervention occurred for each of the 2 groups, resulting in rates of 1.6% for GA and 0.4% for LA patients; P = 0.12. In patients undergoing LA thyroidectomy; postoperative neck swelling became apparent within the 6-hour observation period, with early exploration performed under LA. No patient experienced airway compromise, and bleeding was either superficial or deep to the strap muscles in each of 2 cases. Conventional thyroidectomy patients experienced postoperative hematoma at 5 hours (2 patients), 2 days, and 5 days from the surgical procedure. Of the 2 patients who bled at 5 hours postoperatively, 1 underwent reexploration using LA, with mild, nonspecific oozing noted in the subplatysmal area. The second patient had undergone extensive substernal goiter resection and required transfusion for coagulopathy and significant bleeding from a closed suction drain placed at the time of procedure. Following this therapy bleeding subsided, and no operative intervention was necessary. Both patients with delayed hematoma underwent resection of substernal goiters and had cardiac comorbidity requiring anticoagulation or antiplatelet therapy. The hematoma at 2 days occurred in a patient monitored as an inpatient during reinstitution of heparin therapy. No specific bleeding site was identified at reexploration. The last patient who experienced a large hematoma with a rapid onset at 5 days postoperatively was found to have a bleeding superior pole arterial vessel from a slipped tie, with decompression of hematoma into the subplatysmal and subcutaneous tissue plains and no associated respiratory problems prior to definitive operative exploration. This patient accounted for the one readmission required in this study.
Hypoparathyroidism was a rare event, occurring in only 1 LA patient undergoing resection of malignancy and in no GA patient. Temporary hypoparathyroidism was not reported since postoperative calcium (± vitamin D) therapy was used routinely in at-risk patients, and hypocalcemic symptoms were likely underreported or of no clinical significance. Emergency tracheostomy was necessary in 1 GA patient for tracheal compression and narrowing due to massive goiter and in 1 LA patient as a result of inadvertent nerve injury during goiter resection with respiratory compromise. Unique complications occurred in GA patients associated with locally advanced cancer resection and included tracheal perforation (n = 1) and chylous leak (n = 1).
Cost Analysis
Table 3 shows cost data for 302 consecutive patients undergoing thyroidectomy procedures using LA (72%, n = 217) or GA (18%, n = 85) during years 2002–2003 by surgeons (n = 5) with a focus in endocrine surgery at Columbia University Medical Center. Overall, there was an appreciable difference in mean ATC for local ($2,974) and general procedures ($4,412), P = 0.006, with the combined mean ATC per case heavily impacted by a higher volume of LA thyroidectomy procedures (ratio = 2.6:1). The mean ATC for a GA procedure is 48% higher than for an LA case and 30% higher than the ATC per case for all procedures combined. Conversely, the ATC for an LA procedure is 33% lower than that for a conventional GA thyroidectomy and 12% lower than the ATC per case for LA and GA procedures combined.
A comparison of the 2 approaches adjusted for factors possibly associated with cost demonstrate that extensive procedures and increased operating room times were associated with the highest mean ATC per case; P < 0.001. For thyroidectomy performed with concomitant procedures or bilateral thyroidectomy under GA, costs were 54%–61% higher than for the same types of cases performed using LA. Furthermore, unilateral procedures were associated with a 23% lower mean ATC using LA ($2,862) compared with GA ($3,731). Operating room duration significantly impacted mean ATC for each group. The calculated ATC per minute operating room utilized was $11.35 for GA and $11.42 for LA procedures. ATC was impacted by longer room times for thyroidectomy using GA compared with LA (median 180 vs. 120 minutes; P < 0.001) and the greater predictability of operating room utilization for LA procedures [ATC per minute room utilization standard deviation (SD): $4.08 vs. $1.95, GA vs LA, respectively; P < 0.001]. When outpatient status was achieved, the ATC per case was only 14% higher for conventional GA thyroidectomy compared with LA thyroidectomy and 27% higher when patients were admitted for overnight observation, P = 0.023. (Table 3).
DISCUSSION
Patient Selection
Since LA rapidly became the preferred method for performing thyroidectomy at our institution with its broad application to a majority of patients from 1996,1,15,16 it is not surprising to see further separation and distinction of the types of patients and procedures performed using each method in this comparative cohort study. This study demonstrates that certain thyroid-related pathologies are more commonly and optimally managed using a GA approach, such as extensive substernal and symptomatic goiter, locally advanced or regional thyroid cancer, and complicated reoperative procedures. While substernal goiter may also be treated using LA, in a previous publication, risk for conversion to GA was demonstrated, which was similarly seen in locally or regionally advanced cancer.1 These data are in agreement with recent reports from others evaluating risk factors for airway compromise in goiter resection,27,28 complications of substernal thyroid resection,24,28–30 and thyroid cancer operation,31–33 all challenging clinical scenarios managed using GA.
Since administration of GA has become safer in recent times, this modality has been utilized safely in patients with comorbidity,34–36 which is also demonstrated in this report. Overall, few patient-related factors mandate either approach to thyroidectomy. However, an interesting and unique application of LA involves a subset of patients with amiodarone-induced hyperthyroidism (AIT). In this series, all cases of AIT were treated with LA exclusively and comprised 9 of the 11 cases with ASA scores ≥3. Other series addressing thyroidectomy in AIT patients where GA is used have described incidences of mortality related to anesthesia.36,37 Our opinion is that this subset of patients uniquely benefits from an LA thyroidectomy approach.
Recurrent and Superior Laryngeal Nerve Monitoring
Endocrine surgery literature addresses many methods of nerve identification and monitoring during thyroidectomy that have yet to demonstrate improved nerve injury rates in comparative analyses.38–43 To prove any given method superior would be a hard task since nerve injury incidence is low,23 experience counts,44–48 and many patient- and thyroid-related factors influence outcomes.49–51
A patient who is awake and able to phonate allows for immediate feedback to the surgeon and patient regarding the integrity of the speaking voice and pitch. We feel this is the most accurate means of monitoring the voice during thyroid surgery. In this series, we have shown that the LA method is, at the least, not inferior to standard conventional thyroidectomy performed without specific nerve monitoring. There has been concern to those adverse to LA thyroidectomy procedure that an awake patient who is able to move about, speak, and swallow may actually impose increased risk of unintended nerve injury. However, no nerve injury was attributable directly to anesthetic choice in this or previous publications.1 Thyroid pathology was identified as an important factor in each case of unintended nerve injury, namely, cancer, thyroiditis, and large goiter.
Though difficult to quantify, potential nerve injury may have been reduced in cases performed using LA where feedback of nerve integrity was vital to preserving its function. An identical case performed under GA without specific monitoring may have resulted in nerve damage. Likewise, it is difficult to know if unintended injury might have been avoided in any of the 6 patients in the GA group who experienced temporary or permanent nerve injury if phonation had been possible. More specific proof of the efficacy of nerve monitoring during thyroidectomy using LA would only be possible with a larger number of GA patients.
Outpatient Thyroid Surgery and Management of Potential Delayed Operative Morbidity
Since The Institute of Medicine report on hospital medical errors52,53 and ongoing pressures for cost containment, further interest has been encouraged in performing LA procedures as outpatients wherever possible in order to maximize patient safety and decrease cost across all specialties of medicine and surgery. Patients as consumers continue to place demands on less invasive methods and the importance of cosmetic results.54–59 This has sparked interesting debates in the endocrine surgical community with regard to the safety of early discharge and methods of thyroidectomy.16
It has become clear that prior barriers to early discharge, such as hypocalcemia, pain, nausea, and vomiting are no longer considered by most clinicians to pose significant risk to ambulatory thyroid surgery patients. These concerns have been addressed in the literature and similarly in our unit.1,15,16,19,20,60,61 Protocols of calcium prophylaxis with or without vitamin D therapy for high-risk patients have proven effective and safe.57,62 Likewise, cervical block analgesia15,63,64 and decreased opioid use in the perioperative period65 with improvement of associated nausea and vomiting symptoms all contribute to the successful early discharge of patients and decreased readmission rates observed in contemporary outpatient thyroidectomy reports (Table 5).
Early discharge of patients following thyroidectomy is controversial since potentially life-threatening neck hematoma has been documented to occur beyond a short-stay, 6-hour, observation period.21,66–68 It has been suggested that early discharge of patients may result in increased mortality due to this serious complication occurring outside a hospital setting.16,66 Many endocrine surgeons impose a 23-hour observation period or longer in order to assure safe discharge of patients. (Table 5). Furthermore, some suggest that in observing patients for 23-hours, an additional 38%–50% of serious complications otherwise missed with early discharge would be captured, supporting longer hospital stays for thyroidectomy procedures.16,66 (Table 6). However, emerging data suggest that life-threatening airway compromise or bleeding in fact occurs within the first 6-hours of observation.1,69,70 It therefore becomes vital to observe patients in a recovery room or monitored setting, as described in this report, in order to recognize and address these issues optimally should they arise. This may also explain the fact that hematoma was not observed beyond 6-hour observation in our series since any signs of swelling were treated early, aggressively, and safely, perhaps avoiding the types of intermediate-delayed hematoma reported by others to occur within a 6- to 23-hour time-period postoperatively (Table 6).
Delayed neck hematoma (>24 hours up to 5 days) was observed in our study and likewise has been reported by others.21,65–67,71 In a report by Burkey et al.,66 19% of hematomas requiring therapy occurred beyond 24 hours. It is interesting to note that in the present report, delayed bleeding occurred in GA patients only: an inpatient with coagulopathy and an outpatient due to technical error. Although these occurrences were low, subtle yet important distinctions between the 2 techniques—LA vs. GA—become vastly apparent. These distinctions highlight potential areas of improvement toward the reduction of delayed hematoma and prevention of airway compromise since delayed occurrences of neck hematoma will assuredly take place in an outpatient setting in some cases (Table 6).
First, an awake patient undergoing thyroidectomy using LA is asked to cough and Valsalva, which supplies immediate real-time feedback to the surgeon regarding the integrity and durability of hemostatic control. This is not possible to the same degree with a patient under GA. It is likely that the technical error in the patient with delayed bleed at 5 days may have been noticed using these techniques, which are possible only under LA. Also, particular vigilance on the part of the operating surgeon to secure absolute hemostasis in patients who are likely to be discharged early may occur when an outpatient thyroidectomy program is in place. Furthermore, for both LA and GA patients, we employ a technique whereby the lower strap muscles are left open. This was vital to the prevention of tracheal compression in the case of rapid, delayed bleeding that occurred in an outpatient setting since the patient was able to recognize swelling early and was alleviated of potential airway embarrassment with decompression of blood into the superficial soft tissue planes.
We have shown that outpatient thyroid surgery is feasible and safe in both LA1 and GA patients when implemented within the context of a mature outpatient thyroidectomy program with procedures performed in appropriately selected patients by experienced, high-volume surgeons with expertise in thyroid surgery. Delayed hematoma in GA patients remains an area for further study and particular caution. It is likely that these criteria applied to similar tertiary centers would meet with similar excellent results.
Cost Associated with Thyroidectomy Using Local or General Anesthesia
In this series, and similar to other reports investigating cost associated with outpatient thyroidectomy,11–14 we have shown a reduction in ATC for patients undergoing thyroidectomy using the LA method ($2,974) compared with GA ($4,412); P = 0.006. Early discharge (6-hour observation) was a significant factor impacting both GA and LA procedures, with a 43% and 37% reduction in ATC per case, respectively, compared with procedures performed with longer hospital stays. Thyroidectomy performed as an outpatient using GA was 14% more costly than procedures performed as outpatients under LA ($3,153 vs. $2,760) and 27% more costly for those staying longer than 6 hours ($5,542 vs. $4,362); P = 0.023.
Although outpatient status may contribute to cost containment for thyroidectomy procedures, factors such as operating room utilization and necessary extent of procedures performed are also important areas to explore. ATC per case was significantly impacted by increased overall operating room time associated with GA procedures (180 vs. 120 minutes; GA vs. LA; P < 0.001). Room utilization was also less predicable in GA cases, which translated to significantly varied per-minute costs associated with GA procedures (SD: $4.08 vs. $1.95; GA vs. LA; P < 0.001). Likewise, more extensive procedures, such as bilateral thyroidectomy and concomitant procedures, also resulted in increased ATC per case for thyroidectomy performed using GA compared with LA; P < 0.001.
Interpretation of these data should be tempered with consideration of limitations inherent to the dataset. Surgeon experience has been shown to influence outcomes and associated cost for thyroidectomy procedures44,47,48 and is not controlled for in this study. Also, since our thyroidectomy program is heavily weighted toward performing procedures using LA, there are fewer GA cases represented in this comparison, which introduces a bias into the calculated weighted averages. Nonetheless, cost associated with LA procedures appears to be lower than those for GA. More work is needed to determine specific areas of focus to improve overall associated cost of thyroidectomy.
ReferenceS
Spanknebel K, Chabot JA, DiGiorgi M, et al. Thyroidectomy using local anesthesia: a report of 1,025 cases over 16 years. J Am Coll Surg 2005;201:375–385
Cunningham IG, Lee YK. The management of solitary thyroid nodules under local anaesthesia. Aust N Z J Surg 1975;45:285–289
Fernandez FH. Cervical block anesthesia in thyroidectomy. Int Surg 1984;69:309–311
Saxe AW, Brown E, Hamburger SW. Thyroid and parathyroid surgery performed with patient under regional anesthesia. Surgery 1988;103:415–420
Hochman M, Fee WE Jr. Thyroidectomy under local anesthesia. Arch Otolaryngol Head Neck Surg 1991;117:405–407
Kulkarni RS, Braverman LE, Patwardhan NA. Bilateral cervical plexus block for thyroidectomy and parathyroidectomy in healthy and high risk patients. J Endocrinol Invest 1996;19:714–718
Samson PS, Reyes FR, Saludares WN, et al. Outpatient thyroidectomy. Am J Surg 1997;173:499–503
Prasad KC, Shanmugam VU. Major neck surgeries under regional anesthesia. Am J Otolaryngol 1998;19:163–169
Specht MC, Romero M, Barden CB, et al. Characteristics of patients having thyroid surgery under regional anesthesia. J Am Coll Surg 2001;193:367–372
Hisham AN, Aina EN. A reappraisal of thyroid surgery under local anaesthesia: back to the future? ANZ J Surg 2002;72:287–289
Steckler RM. Outpatient thyroidectomy: a feasibility study. Am J Surg 1986;152:417–419
Marohn MR, LaCivita KA. Evaluation of total/near-total thyroidectomy in a short-stay hospitalization: safe and cost-effective. Surgery 1995;118:943–947
Mowschenson PM, Hodin RA. Outpatient thyroid and parathyroid surgery: a prospective study of feasibility, safety, and costs. Surgery 1995;118:1051–1053
McHenry CR. “Same-day” thyroid surgery: an analysis of safety, cost savings, and outcome. Am Surg 1997;63:586–589
LoGerfo P. Local/regional anesthesia for thyroidectomy: evaluation as an outpatient procedure. Surgery 1998;124:975–978
Schwartz AE, Clark OH, Ituarte P, et al. Therapeutic controversy: thyroid surgery–the choice. J Clin Endocrinol Metab 1998;83:1097–1105
LoGerfo P, Kim LJ. Technique for regional anesthesia: thyroidectomy and parathyroidectomy. Oper Tech Gen Surg 1999;1:95–102
Williams M, LoGerfo P. Thyroidectomy using local anesthesia in critically ill patients with amiodarone-induced thyrotoxicosis: a review and description of the technique. Thyroid 2002;12:523–525
LoGerfo P, Gates R, Gazetas P. Outpatient and short-stay thyroid surgery. Head Neck 1991;13:97–101
LoGerfo P, Ditkoff BA, Chabot J, et al. Thyroid surgery using monitored anesthesia care: an alternative to general anesthesia. Thyroid 1994;4:437–439
Foster RS Jr. Morbidity and mortality after thyroidectomy. Surg Gynecol Obstet 1978;146:423–429
Hundahl SA, Fleming ID, Fremgen AM, et al. A national cancer data base report on 53,856 cases of thyroid carcinoma treated in the U.S., 1985–1995 [see comments]. Cancer 1998;83:2638–2648
Hundahl SA, Cady B, Cunningham MP, et al. Initial results from a prospective cohort study of 5583 cases of thyroid carcinoma treated in the united states during 1996. U.S. and German Thyroid Cancer Study Group. An American College of Surgeons Commission on Cancer Patient Care Evaluation study. Cancer 2000;89:202–217
Thomusch O, Machens A, Sekulla C, et al. Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: prospective multicenter study in Germany. World J Surg 2000;24:1335–1341
Rosato L, Avenia N, Bernante P, et al. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg 2004;28:271–276
Goncalves FJ, Kowalski LP. Surgical complications after thyroid surgery performed in a cancer hospital. Otolaryngol Head Neck Surg 2005;132:490–494
Shen WT, Kebebew E, Duh QY, et al. Predictors of airway complications after thyroidectomy for substernal goiter. Arch Surg 2004;139:656–659
Rios A, Rodriguez JM, Canteras M, et al. Surgical management of multinodular goiter with compression symptoms. Arch Surg 2005;140:49–53
Zambudio AR, Rodriguez J, Riquelme J, et al. Prospective study of postoperative complications after total thyroidectomy for multinodular goiters by surgeons with experience in endocrine surgery. Ann Surg 2004;240:18–25
Erbil Y, Bozbora A, Barbaros U, et al. Surgical management of substernal goiters: clinical experience of 170 cases. Surg Today 2004;34:732–736
Patel KN, Shaha AR. Locally advanced thyroid cancer. Curr Opin Otolaryngol Head Neck Surg 2005;13:112–116
Kikuchi S, Perrier ND, Cheah WK, et al. Complication of thyroidectomy in patients with radiation-induced thyroid neoplasms. Arch Surg 2004;139:1185-1188
Nakao K, Kurozumi K, Nakahara M, et al. Resection and reconstruction of the airway in patients with advanced thyroid cancer. World J Surg 2004;28:1204–1206
Ferrier MB, Spuesens EB, Le Cessie S, et al. Comorbidity as a major risk factor for mortality and complications in head and neck surgery. Arch Otolaryngol Head Neck Surg 2005;131:27–32
Franzese CB, Fan CY, Stack BC Jr. Surgical management of amiodarone-induced thyrotoxicosis. Otolaryngol Head Neck Surg 2003;129:565–570
Houghton SG, Farley DR, Brennan MD, et al. Surgical management of amiodarone-associated thyrotoxicosis: Mayo Clinic experience. World J Surg 2004;28:1083–1087
Mittendorf EA, McHenry CR. Thyroidectomy for selected patients with thyrotoxicosis. Arch Otolaryngol Head Neck Surg 2001;127:61–65
Otto RA, Cochran CS. Sensitivity and specificity of intraoperative recurrent laryngeal nerve stimulation in predicting postoperative nerve paralysis. Ann Otol Rhinol Laryngol 2002;111:1005–1007
Marcus B, Edwards B, Yoo S, et al. Recurrent laryngeal nerve monitoring in thyroid and parathyroid surgery: the University of Michigan experience. Laryngoscope 2003;113:356–361
Scheuller MC, Ellison D. Laryngeal mask anesthesia with intraoperative laryngoscopy for identification of the recurrent laryngeal nerve during thyroidectomy. Laryngoscope 2002;112:1594–1597
Hermann M, Hellebart C, Freissmuth M. Neuromonitoring in thyroid surgery: prospective evaluation of intraoperative electrophysiological responses for the prediction of recurrent laryngeal nerve injury. Ann Surg 2004;240:9–17
Witt RL. Electrophysiologic monitoring of the recurrent laryngeal nerves may not predict bilateral vocal fold immobility after thyroid surgery. J Voice 2004;18:256–260
Beldi G, Kinsbergen T, Schlumpf R. Evaluation of intraoperative recurrent nerve monitoring in thyroid surgery. World J Surg 2004;28:589–591
Sosa JA, Bowman HM, Tielsch JM, et al. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg 1998;228:320–330
Mishra A, Agarwal G, Agarwal A, et al. Safety and efficacy of total thyroidectomy in hands of endocrine surgery trainees. Am J Surg 1999;178:377–380
Bliss RD, Gauger PG, Delbridge LW. Surgeon’s approach to the thyroid gland: surgical anatomy and the importance of technique. World J Surg 2000;24:891–897
Acun Z, Cihan A, Ulukent SC, et al. A randomized prospective study of complications between general surgery residents and attending surgeons in near-total thyroidectomies. Surg Today 2004;34:997–1001
Udelsman R. Experience counts. Ann Surg 2004;26–27
Yarbrough DE, Thompson GB, Kasperbauer JL, et al. Intraoperative electromyographic monitoring of the recurrent laryngeal nerve in reoperative thyroid and parathyroid surgery. Surgery 2004;136:1107–1115
Chan WF, Lo CY, Lam KY, et al. Recurrent laryngeal nerve palsy in well-differentiated thyroid carcinoma: clinicopathologic features and outcome study. World J Surg 2004;28:1093–1098
Sinagra DL, Montesinos MR, Tacchi VA, et al. Voice changes after thyroidectomy without recurrent laryngeal nerve injury. J Am Coll Surg 2004;199:556–560
Kohn KT, Corrigan JM, Donaldson MS. To err is human: Building a safer health system. Washington, DC, National Academy Press, 1999
Leape LL, Berwick DM. Five years after To err is human: what have we learned? JAMA 2005;293:2384–2390
Miccoli P, Berti P, Raffaelli M, et al. Comparison between minimally invasive video-assisted thyroidectomy and conventional thyroidectomy: a prospective randomized study. Surgery 2001;130:1039–1043
Ikeda Y, Takami H, Sasaki Y, et al. Are there significant benefits of minimally invasive endoscopic thyroidectomy? World J Surg 2004;28:1075–1078
Sackett WR, Barraclough BH, Sidhu S, et al. Minimal access thyroid surgery: is it feasible, is it appropriate? ANZ J Surg 2002;72:777–780
Bellantone R, Lombardi CP, Raffaelli M, et al. Is routine supplementation therapy (calcium and vitamin D) useful after total thyroidectomy? Surgery 2002;132:1109–1112
Ikeda Y, Takami H, Sasaki Y, et al. Comparative study of thyroidectomies. Endoscopic surgery versus conventional open surgery. Surg Endosc 2002;16:1741–1745
Seven H, Calis AB, Vural C, et al. Microscopic thyroidectomy: a prospective controlled trial. Eur Arch Otorhinolaryngol 2005;262:41–44
Testini M, Nacchiero M, Miniello S, et al. One-day vs standard thyroidectomy. A perspective study of feasibility. Minerva Endocrinol 2002;29:225–229
Sahai A, Symes A, Jeddy T. Short-stay thyroid surgery. Br J Surg 2005;92:58–59
Moore FD Jr. Oral calcium supplements to enhance early hospital discharge after bilateral surgical treatment of the thyroid gland or exploration of the parathyroid glands. J Am Coll Surg 1994;178:11–16
Park GR, Drummond GB, Sinclair IS, et al. Bupivacaine infiltration for thyroid surgery. J R Coll Surg Edinb 1983;28:295–296
Aunac S, Carlier M, Singelyn F, et al. The analgesic efficacy of bilateral combined superficial and deep cervical plexus block administered before thyroid surgery under general anesthesia. Anesth Analg 2002;95:746–750
Sonner JM, Hynson JM, Clark O, et al. Nausea and vomiting following thyroid and parathyroid surgery. J Clin Anesth 1997;9:398–402
Burkey SH, Van Heerden JA, Thompson GB, et al. Reexploration for symptomatic hematomas after cervical exploration. Surgery 2001;130:914–920
Lacoste L, Gineste D, Karayan J, et al. Airway complications in thyroid surgery. Ann Otol Rhinol Laryngol 1993;102:441–446
Abbas G, Dubner S, Heller KS. Re-operation for bleeding after thyroidectomy and parathyroidectomy. Head Neck 2001;23:544–546
Shaha AR, Jaffe BM. Practical management of post-thyroidectomy hematoma. J Surg Oncol 1994;57:235–238
Hurtado-Lopez LM, Zaldivar-Ramirez FR, Basurto KE, et al. Causes for early reintervention after thyroidectomy. Med Sci Monit 2002;8:CR247–CR250
Bergamaschi R, Becouarn G, Ronceray J, et al. Morbidity of thyroid surgery. Am J Surg 1998;176:71–75
Acknowledgements
With gratitude and appreciation, we wish to acknowledge colleagues and staff at the New York Thyroid Center, especially Bonnie Badenchini, Mary DiGiorgi, Diana Hernandez, and Dianna Walsh who, with dedication and devotion, supported the patients, professional practice, and research endeavors of Paul LoGerfo and to whom we owe much to the completion of his work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spanknebel, K., Chabot, J.A., DiGiorgi, M. et al. Thyroidectomy Using Monitored Local or Conventional General Anesthesia: An Analysis of Outpatient Surgery, Outcome and Cost in 1,194 Consecutive Cases. World J. Surg. 30, 813–824 (2006). https://doi.org/10.1007/s00268-005-0384-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0384-3