Abstract
Background
Concern for postoperative complications causing airway compromise has limited widespread acceptance of ambulatory thyroid surgery. We evaluated differences in outcomes and hospital costs in those monitored for a short stay of 6 h (SS), inpatient observation of 6–23 h (IO), or inpatient admission of >23 h (IA).
Methods
We retrospectively reviewed all patients undergoing thyroidectomy from 2006 to 2012. The incidence of postoperative hemorrhage, nerve dysfunction, and hypocalcemia were evaluated, as well as cost data comparing the SS and IO groups.
Results
Of 1447 thyroidectomies, 880 (60.8 %) were performed as SS, 401 (27.7 %) as IO, and 166 (11.5 %) as IA. Fewer patients in the SS group (59 %) underwent total thyroidectomy than IO (73 %) and IA (71 %; p < 0.01), and SS patients had smaller thyroid weights (27.9 g) compared with IO and IA (47.2 and 98.9 g, respectively; p < 0.01). Ten (0.69 %) patients developed hematomas requiring reoperation, five of the ten patients received antiplatelet or anticoagulant therapy perioperatively. Only one patient in the IA group bled within the 6- to 23-h period, and no patients with bleeding who were discharged at 6 h would have benefitted from 23-h observation. Twenty-four (1.66 %) recurrent laryngeal nerve injuries were identified, 16 with temporary neuropraxias. In addition, 24 (1.66 %) patients had symptomatic hypocalcemia, which was transient in 17 individuals. Financial data showed higher payments and lower costs associated with SS compared with IO.
Conclusions
Selective SS thyroidectomy can be safe and cost effective, with few overall complications in patients undergoing more complex operations involving larger thyroids who were admitted to hospital.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Short-stay (SS) thyroidectomy has been extensively debated in the surgical literature and has been found by a number of groups to be safe and cost effective. Some of the first proponents of this practice, Lo Gerfo et al.1 selectively performed ambulatory thyroid surgery without significant morbidity, thereby making a case for the safety of this practice. However, surgeons still have concerns about the potential for significant, life-threatening complications, including airway compromise from expanding hematomas and recurrent laryngeal nerve injury. A few large patient series have determined that most bleeding complications requiring reoperation occurred within the first 6 h post-thyroidectomy.1–4 We thus examined patients who underwent thyroid operations to evaluate rates of, and risk factors for, postoperative bleeding, as well as other significant complications such as nerve injury and symptomatic hypocalcemia. We hypothesized that the majority of severe complications requiring reoperation would occur within the first 6 h after thyroid surgery and that patients could be safely discharged home after close monitoring during this time period. Avoiding the need for inpatient observation (IO) periods or admission may increase patient satisfaction and diminish hospital costs.
Methods
All thyroidectomies performed by a single, high-volume surgeon at Rutgers Robert Wood Johnson University Hospital between January 2006 and December 2012 were retrospectively reviewed. The study was approved by the Rutgers Institutional Review Board. Study parameters included patient demographics such as age, sex, and American Society of Anesthesiology (ASA) classification, and operative data included estimated blood loss (EBL; in milliliters [mL]) and the operation performed. Pathologic data included thyroid weight (in grams [g]) and malignant or benign diagnosis. Specific postoperative complications examined were emergency room visits or inpatient hospitalization within 30 postoperative days, hematoma requiring reoperation, recurrent laryngeal nerve injury, symptomatic hypocalcemia, and 30-day mortality. Financial data, including total payment per case (TPC), direct cost per case (DCC), and contribution to margin per case (CMC) were obtained and analyzed for the year 2012.
Patients were retrospectively divided into three groups: SS patients were monitored for 6 h postoperatively and discharged, IO patients were monitored for 6–23 h and then discharged, and inpatient admission (IA) patients were admitted for more than 23 h.
Education and Evaluation
Prior to initial evaluation in the office, all patients attended an educational session outlining the surgery and postoperative expectations, including signs of hematoma development, nerve injury, and hypocalcemia. They were encouraged to bring family members to this session and given detailed written instructions. After surgery, all patients were monitored in the postoperative care unit for at least 6 h and were evaluated by the attending surgeon or a senior house staff member who decided whether the patient was safe for discharge. Elderly patients with significant comorbidities and those who underwent modified radical neck dissections (MRND) were admitted for IO. All patients undergoing total thyroidectomy were discharged on calcium and vitamin D.
Patients taking aspirin alone were commonly discharged in the 6 h SS group and were allowed to restart their aspirin the day after surgery. Patients taking Plavix®, Coumadin®, or other anticoagulants were admitted for IO. Coumadin® was restarted on the first postoperative day, with frequent international normalized ratio (INR) checks upon discharge. The resumption of Plavix® was based on the individual’s need for antiplatelet therapy balanced with their risk of postoperative bleeding.
Statistical Analysis
Statistical analysis using GraphPad Prism statistical software comparing all three groups was performed using one-way analysis of variance (ANOVA), and comparisons made between groups using Tukey’s multiple comparisons test and unpaired t-tests for comparison of means. A p value <0.05 indicated statistical significance.
Results
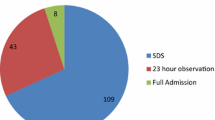
Of the 1447 thyroid operations performed between 2006 and 2012, 880 (60.8 %) were performed as SS, 401 (27.7 %) as IO, and 166 (11.5 %) as IA. Eighty-one percent of patients were female, with more females in the SS group (83.8 %) than the IO (78.8 %) or IA (74.1 %; p < 0.01) groups. SS patients were younger and had a lower mean ASA (with data available for 81 % of patients) than IO or IA patients (Table 1). Patients had larger mean thyroid weights in the IO (47.2 g) and IA (98.9 g) groups compared with the SS group (27.9 g; p < 0.01), as well as a significantly higher EBL in the IO (39.6 mL) and IA (123.5 mL) groups than the SS group (approximately 7.0 ml; p < 0.01). Thyroid malignancies were more frequent in the IA group (43.4 %) compared with the SS (28.4 %) and IO (29.7 %) groups (p < 0.01), demonstrating that patients who underwent operations with larger thyroids, higher EBL, and with more malignancies were admitted for longer than the 6-h period. Subsequently, 92.7 % of patients in the IA group had a drain placed compared with 11.9 % in the IO group and none in the SS group (p < 0.01).
The operations performed also differed for each group (Table 1). Total thyroidectomy was the most common procedure overall (64.4 % of the total), including 520 patients (59 %) from the SS group, 294 (73 %) from the IO group, and 118 patients (71 %) from the IA group. The remaining patients underwent lobectomies. One hundred central neck dissections were performed—49 (5.5 %) in the SS group, 25 (6.2 %) in the IO group, and 26 (15.7 %) in the IA group. MRNDs were only performed as IO (0.49 %) and IA (24.7 %) procedures.
Complications
Overall, few complications were observed. Forty-one (2.8 %) patients visited the emergency department (ED) within 30 days post-thyroidectomy, without significant difference between the three groups (SS 22, IO 13, and IA 6 patients; p = 0.45). Seventeen patients (1.17 %) were readmitted within the 30-day time period—five (0.56 %) in the SS group, seven (1.74 %) in the IO group, and five (3.0 %) in the IA group, with a significant difference between SS and IA (p < 0.01).
Postoperative Hematoma Development
Ten (0.69 %) patients developed hematomas requiring reoperation (Table 2). Of these, the mean age was 75 years, with an equal distribution of males and females. Six patients had hypertension, three patients had coronary artery disease (CAD), and one patient had atrial fibrillation, asthma, and chronic kidney disease. Six patients underwent thyroid lobectomy (two completion thyroidectomies), and four patients underwent total thyroidectomy, with one MRND. Eight patients had multinodular goiters and two patients had metastatic papillary thyroid cancer. Of the ten patients who underwent hematoma evacuation, thyroid weight data were available for nine patients, with a mean of 36.8 g and a mean EBL of 62.5 mL. Five patients who developed hematomas were determined to be using antiplatelet and/or anticoagulant agents. No patients discharged at 6 h had bleeding that would have benefitted from a 23-h stay for observation, and none were seen at an outside ED within 24 h of surgery. There were no emergency bedside hematoma evacuations, emergent tracheostomies, or mortalities related to compressive hematomas.
In the SS group, three patients required hematoma evacuation: two individuals taking aspirin had late hemorrhage on postoperative days five (after straining) and nine. Another bled just prior to extubation after coughing.
Of the IO patients, four developed hematomas—two on the day of surgery, one (with papillary thyroid cancer with strap muscle invasion) was evacuated prior to extubation, and another (with an adherent multinodular goiter) had hematoma evacuation within 4 h postoperatively. One patient presented with bleeding 26 h after lobectomy for superior mediastinal goiter, and another, using aspirin, Plavix® and Coumadin® for coronary stents and deep vein thrombosis, presented on postoperative day 10.
Three patients in the IA group developed hematomas requiring reoperation. One patient underwent total thyroidectomy for multinodular goiter and was explored immediately after extubation for excessive blood in the Jackson Pratt drain. Her aspirin and Plavix® (for CAD) were held preoperatively and restarted during the hospital admission. Another patient bled on postoperative day 5 after resection of mediastinal multinodular goiter. The last patient underwent total thyroidectomy and MRND for metastatic papillary thyroid cancer. He bled 24 h after initial surgery secondary to a small artery under the left flap. His aspirin and Coumadin® were also held preoperatively.
Recurrent Laryngeal Nerve Dysfunction
Twenty-four patients (1.66 %) had recurrent laryngeal nerve dysfunction, significantly higher in the IA group than the SS group (p < 0.01) [Table 3]. Sixteen patients had temporary neuropraxias and eight had permanent injuries (five with preoperative nerve dysfunction). Five patients underwent temporary tracheostomy placement for airway protection; three with temporary injuries required vocal cord injection and two underwent vocal training. No incidences of permanent nerve dysfunction were observed in the SS group. Of these 24 patients, 19 (79 %) underwent total thyroidectomy, 4 (16.7 %) underwent lobectomies, and 1 underwent removal of recurrent cancer. Eleven patients had multinodular goiters (five were massive or compressive), one had Hashimoto’s thyroiditis, and the remaining 12 patients had various malignant pathologies (three with metastatic disease). A total of 1220 (84.3 %) patients had intraoperative nerve monitoring.
Hypocalcemia
Twenty-four patients (1.66 %) presented with symptomatic postoperative hypocalcemia (Table 3). Seventeen presented with transient hypocalcemia which resolved. A significant difference was found between the SS (10 patients) and IA groups (9 patients; p = 0.02) but not compared with the IO group, likely due to the higher proportion of total thyroidectomies and neck dissections in the IA group. Of patients with hypocalcemia, 22 (91.7 %) underwent total thyroidectomy, four with concurrent MRNDs, and five needed reimplantation of at least one parathyroid gland.
Cost Analysis
Cost data (Table 4), including TPC, DCC, and CMC, were obtained for the year 2012 to determine whether a financial advantage existed with earlier discharge (6-h observation compared with 23-h observation). When comparing the SS and IO groups, the TPC was significantly higher—$4023 compared with $3347 (p < 0.01). The DCC was also lower—$3058 versus $3596 (p < 0.08). The SS group made a $965 profit per case compared with a $249 loss in the IO group (p < 0.01).
Discussion
The ability for surgeons to safely discharge patients after an SS observation period following thyroidectomy has been much debated, with increasing evidence for the safety of this practice. Postoperative hematoma is a rare but potentially lethal complication, with a reported incidence ranging from 0.1 to 4.7 %.5,6 In this study, 0.69 % of patients developed postoperative cervical hematomas requiring evacuation, well within the expected range. Significant post-thyroidectomy hematomas often occur within the first 6 h postoperatively. This was the case in 40 % of our patients. However, the major concern for opponents of SS thyroidectomy is the development of late postoperative hemorrhage with subsequent airway compromise. Forty percent of patients in this study developed neck hematomas 5 days or more after initial surgery; thus, accurate temporal prediction of late postoperative hematomas is difficult, with a predilection for late bleeding in patients using anticoagulant or antiplatelet agents.7,8
Campbell et al.9 found that patients who returned to the operating room for cervical hematoma evacuation were likely to be older males, taking anticoagulant/antiplatelet medications, with larger thyroids and higher EBL, and undergoing total thyroidectomies for benign disease. Other factors noted in various studies to be risk factors for cervical hematoma development include postoperative hypertension, alcohol abuse, chronic kidney disease, Graves’ disease, and reoperative thyroidectomy.3,5,6,10–12
In this study, patients who developed hematomas were older (mean age of 75 years), mostly undergoing lobectomies for multinodular goiter. Mean thyroid weight of 36.8 g and EBL of 62.5 mL were much higher than the averages for the SS group (27.9 g and 7.0 mL, respectively). We also found an association between post-thyroidectomy hematomas and resumption of anticoagulant and antiplatelet agents, especially in those who developed hematomas 5 or more days postoperatively. An association was also found between patients with hypertension and postoperative bleeding (60 % of this group); however, none of our study patients had Graves’ disease or known bleeding disorders.
Operative considerations such as minimizing exposure of the anterior jugular veins, looser closure of the strap muscles, and the Valsalva maneuver may be effective in identifying bleeding vessels and preventing airway compression if hematoma develops.10,13 However, no difference in post-thyroidectomy complications is seen between the use of the clamp tie technique and energy devices.14 Routine placement of cervical drains has been shown to be ineffective in preventing the development of compressive hematomas.15
Recurrent laryngeal nerve injury occurred with very low incidence (1.66 % of patients) in this study compared with up to 30 % in the literature.7,16 Of these, two-thirds had temporary dysfunction and the majority occurred after total thyroidectomies for multinodular goiters or invasive cancers. While intraoperative nerve monitoring does not decrease the rate of injury, it can be useful in postoperative prognostication of vocal cord function.7 Most patients with nerve dysfunction in this study presented with hoarseness and recovered vocal cord function, typically in the 2–3 months following surgery.3
Temporary hypocalcemia was identified in only 1.66 % of patients in this study but can occur in up to 25 % of patients.17 The incidence was found to be significantly higher in IA patients who underwent total thyroidectomies with larger thyroid glands and MRNDs. It is our practice to discharge all patients, after total thyroidectomy, on calcium and vitamin D15, with the addition of calcitriol in those at higher risk of symptomatic hypocalcemia.
Over the 6-year study period, our institution has deemed many patients safe for discharge after 6 h of close observation following thyroid surgery. Factors preventing discharge within this time period included patients with significant comorbidities, larger thyroid glands, and larger intraoperative blood loss. Patients who underwent MRND were always admitted to the hospital, usually for greater than 24 h. Other criteria for patients to be eligible for SS thyroidectomy include good preoperative education, social support, and close proximity to a hospital in order to be able to manage complications expeditiously.17–19 Relative contraindications to SS thyroid operations included significant cardiac and pulmonary comorbidities, the use of anticoagulant and antiplatelet therapy, as well as large thyroid goiters and invasive cancers.17
Reducing hospital expenses is a key factor in determining the benefit of SS thyroidectomy, with a cost difference of $7000 and $22,000 for outpatient and inpatient thyroidectomy, respectively.7,20 When examining the literature, it has been difficult to differentiate between SS (same-day discharge) and 23-h observation.7 We thus attempted to evaluate if there was a financial advantage to discharging patients within a 6-h period compared with IO. In a cost analysis for 2012, we found that the TPC for SS thyroidectomy was higher when compared with IO, while the DCC was lower, resulting in a significantly higher contribution to margin per case in the SS group and a net loss for the IO group. Lower expenditures in the SS group are likely attributable to saving the cost of a hospital bed overnight, as well as lower nursing and pharmacy costs.21
Conclusions
SS thyroidectomy is safe and cost effective. The risk of acute airway compromise from obstructing hematomas is low, but close monitoring in the postoperative area as well as appropriate patient selection is important in determining which patients should have IO versus those who may be safely discharged after a 6-h period. Emphasis must also be placed on thorough education prior to discharge.
References
Lo Gerfo P, Gates R, Gazetas P Outpatient and short-stay thyroid surgery. Head Neck. 1991;13:97–101.
Leyre P, Desurmont T, Lacoste L et al. Does the risk of compressive hematoma after thyroidectomy authorize 1-day surgery? Langenbecks Arch Surg. 2008;393:733–37.
Snyder SK, Hamid KS, Roberson CR et al. Outpatient thyroidectomy is safe and reasonable: experience with more than 1,000 planned outpatient procedures. J Am Coll Surg. 2010;210:575–582, 582–584.
Burkey SH, van Heerden JA, Thompson GB et al. Reexploration for symptomatic hematomas after cervical exploration. Surgery. 2001;130:914–20.
Weiss A, Lee KC, Brumund KT et al. Risk factors for hematoma after thyroidectomy: results from the nationwide inpatient sample. Surgery. 2014;156:399–404.
Dehal A, Abbas A, Hussain F, Johna S. Risk factors for neck hematoma after thyroid or parathyroid surgery: ten-year analysis of the nationwide inpatient sample database. Perm J. 2015;19:22–8.
Steward DL. The pros and cons of outpatient thyroidectomy. JAMA Otolaryngol Head Neck Surg. 2014;140:1074–76.
Calo PG, Erdas E, Medas F et al. Late bleeding after total thyroidectomy: report of two cases occurring 13 days after operation. Clin Med Insights Case Rep. 2013;6:165–70.
Campbell MJ, McCoy KL, Shen WT et al. A multi-institutional international study of risk factors for hematoma after thyroidectomy. Surgery. 2013;154:1283–89, discussion 1289–1291
Morton RP, Mak V, Moss D, Ahmad Z, Sevao J. Risk of bleeding after thyroid surgery: matched pairs analysis. J Laryngol Otol. 2012;126:285–88.
Hardman JC, Smith JA, Nankivell P, Sharma N, Watkinson JC. Re-operative thyroid surgery: a 20-year prospective cohort study at a tertiary referral centre. Eur Arch Otorhinolaryngol. 2015;272:1503–08.
Promberger R, Ott J, Kober F. Risk factors for postoperative bleeding after thyroid surgery. Br J Surg. 2012;99:373–79.
Dixon JL, Snyder SK, Lairmore TC et al. A novel method for the management of post-thyroidectomy or parathyroidectomy hematoma: a single-institution experience after over 4,000 central neck operations. World J Surg. 2014;38:1262–67.
Bircan HY, Inal A, Ozcelik U et al. LigaSure® versus clamp tie technique for thyroid surgery; decreased operative time versus increased inflammatory effect: a prospective randomized study. Eur Rev Med Pharmacol Sci. 2014;18:1997–2005.
Seybt MW, Terris DJ. Outpatient thyroidectomy: experience in over 200 patients. Laryngoscope. 2010;120:959–63.
Fama F, Linard C, Patti R et al. Short-stay hospitalisation for benign thyroid surgery: a prospective study. Eur Arch Otorhinolaryngol. 2013;270:301–04.
Orosco RK, Lin HW, Bhattacharyya N. Ambulatory thyroidectomy: a multistate study of revisits and complications. Otolaryngol Head Neck Surg. 2015;152(6):1017–23.
Doran HE, Palazzo F. Ambulatory thyroid surgery: do the risks overcome the benefits? Presse Med. 2014;43:291–96.
Trottier DC, Barron P, Moonje V, Tadros S. Outpatient thyroid surgery: should patients be discharged on the day of their procedures? Can J Surg. 2009;52:182–6.
Sun GH, DeMonner S, Davis MM. Epidemiological and economic trends in inpatient and outpatient thyroidectomy in the United States, 1996–2006. Thyroid. 2013;23:727–33.
Vrabec S, Oltmann SC, Clark N, Chen H, Sippel RS. A short-stay unit for thyroidectomy patients increases discharge efficiency. J Surg Res. 2013;184:204–08.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Narayanan, S., Arumugam, D., Mennona, S. et al. An Evaluation of Postoperative Complications and Cost After Short-Stay Thyroid Operations. Ann Surg Oncol 23, 1440–1445 (2016). https://doi.org/10.1245/s10434-015-5004-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-5004-3