Abstract
Background
Eyebrow tail ptosis is usually associated with dermatochalasis of the upper eyelid, and it is necessary to treat them together. For these associated procedures to be incorporated as a routine in upper eyelid surgeries, they should preferably be less invasive with consequent fewer complications.
Objective
We describe a minimally invasive technique for the correction of mild-to-moderate eyebrow tail ptosis corrected together with superior dermatochalasis through the blepharoplasty incision.
Methods
A phase 2 clinical trial was conducted from February 2020 to December 2021. A total of 50 patients underwent conventional upper blepharoplasty surgery associated with the proposed eyebrow lift technique: internal pexia in the periosteum, dissection, and posterior fixation of the orbicularis muscle to the arcus marginalis, removal of the lateral part of the orbicularis muscle, and loosening of the orbital retention ligament. Evaluation of the height of the eyebrow tail was performed with digital photography in the initial consultation and at 30–90 days postoperatively and analyzed with ImageJ software.
Results
Mean difference in brow height at 1-month and 3-month postoperative evaluations compared to the preoperative period was 3.45–3.33 mm, respectively.
Conclusion
Our study demonstrated a minimally invasive surgical technique for the treatment of mild-to-moderate eyebrow ptosis with significant eyebrow tail lift results that remained stable during the study period.
Level of Evidence II
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Eyebrow tail ptosis is commonly seen by oculoplastic surgeons and can be explained by the aging of the skin and muscles, with an approximate drop of 2.5 mm every 20 years beginning at 30 years of age [1]. The forces that cause the lateral eyebrow to droop, leading to ptosis of the tail of the brow, include the action of the orbicularis muscle and the mass effect of the eyelid, the forehead fat pad, and the soft tissues of the temporal forehead [2]. Eyebrow ptosis, according to the classification by Real et al. [3], ranges from grade I to grade IV. Each degree is correlated with a numerical interval of height from the most lateral point of the eyebrow to the Frankfurt plane in cm, where > 1.8 cm represents normality; 1.7–1.5 cm grade I ptosis (minimum); 1.4–1.2 cm grade II ptosis (mild); 1.1–0.9 cm grade III ptosis (moderate); and < 0.8 cm grade IV ptosis (severe).
Currently, it is considered that the eyebrow and upper eyelid should be evaluated as a single esthetic unit. Knowing that temporal brow ptosis is a common aging alteration that can increase upper lid fill in upper dermatochalasis (excess eyelid skin), it is of paramount importance to stabilize or lift the brow to complement esthetic upper blepharoplasty [4, 5].
A common frustration expressed by patients after upper blepharoplasty surgery (surgery to correct dermatochalasis) without correction of mild-to-moderate eyebrow ptosis is the feeling that there is still redundant skin on the eyelids, as well as the expressionless esthetics of the gaze. In an attempt to correct this, many surgeons make the mistake of excising eyelid skin beyond the limit, resulting in an out-of-place palpebral crease [6] and shortening the distance between the eyelid and eyebrow, causing both esthetic and functional concerns [7, 8]. However, the existing literature lacks any consensus in regard to whether isolated blepharoplasty results in a change in eyebrow height [9,10,11,12,13], although these studies vary significantly in their methodology.
Eyebrow elevation can be performed using techniques with incisions above or below the eyebrow, with the most effective being those with an incision above the eyebrow, such as direct or endoscopic elevation. These techniques are more costly in terms of time and money, with more scars and potential complications; for these reasons, they are reserved for moderate-to-severe ptosis [4].
For mild-to-moderate eyebrow ptosis, minimally invasive techniques are preferred, ranging from outpatient application of a neurotoxin to surgery through the blepharoplasty incision [14]. The techniques that use the blepharoplasty incision have been gaining popularity for being simpler to perform with good efficacy for lifting or at least stabilizing the eyebrow [15]. Among these, we highlight the internal pexia, where non-absorbable sutures fix the subcutaneous tissue of the eyebrow to the periosteum above the orbital rim. A technique with good results, fixation of the fat pad of the eyebrow, both to improve volume of the brow as well as contour and delineation of the eyelid crease, is the variation of the brassiere fixation suture technique of the brow fat pad published by Briceño et al. [16]. This technique proceeds with the division of the orbicularis muscle into superior and inferior equal parts; then, two sutures are used to secure the inferior edge of the superior portion of the orbicularis muscle to the periosteum of the lateral orbital rim (arcus marginalis) [16]. A complementary technique is the removal of the orbicularis muscle through an inferior lateral excision, weakening the orbicularis muscle [14, 17], and the contraction of which is responsible for lowering the tail of the eyebrow [2].
Some studies noted the importance of releasing the orbital ligament for lateral eyebrow rejuvenation, which can be easily achieved through a transpalpebral approach. The release of this ligament, which is a fibrous band connecting the superficial temporal fascia to the orbital rim, leads to the release of head movement with consequent suspension of the lateral segment of the eyebrow [2, 18]. The major problem seen with these techniques has been inconsistent results. These may be related to the surgeon’s experience, the technique itself, weakness of the procedure, or some combination of these [16].
The aim of this study was to demonstrate a reproducible and safe surgical technique for brow lift through a combination of internal pexy, brassiere fixation suture, weakening of the orbicularis muscle, and release of the orbital ligament with satisfactory functional and esthetic results.
Methods
A prospective clinical study was conducted by the Oculoplastic Department of the Santa Luzia Foundation, Recife, Pernambuco, Brazil, from February 2020 to December 2021.
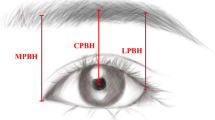
The main outcome was the difference in eyebrow height in mm between the preoperative and 90-day postoperative assessments. With a Nikon b500 professional camera (Japan), full-face digital photographs in PPO were taken of all patients in the frontal plane on the same set at 1.5 m at the initial visit and at the 30-day and 90-day postoperative visits. The three photographs were merged as one photo showing only the periocular area through the Photo Grid application [19]. These photos of patients were then analyzed without masking by the main researcher with the ImageJ software version 1.50c4, developed by the National Institutes of Health (NIH) [20]. To measure the height of the eyebrow, a line was drawn between the medial corners and extended laterally. The vertical distance at the level of the outer corner between this line and the lower edge of the eyebrow was measured and recorded as the temporal eyebrow height (AST), taken bilaterally. Measurements were standardized using a ruler as a parameter that was photographed and analyzed by the program to transform pixels into millimeters, with the interlimbar distance of the cornea in each photograph being the reference point. Care was taken to ensure that the frontalis muscle was relaxed during image-taking by asking patients to close their eyes and gently open them before the photograph was taken.
To calculate the sample, a difference of 3 mm in eyebrow height between the preoperative and 90-day postoperative assessments was considered, with a margin of error of 1% and power of 99%. The calculated minimum sample size was seven patients.
Measurement results were expressed as means and standard deviations. For the comparison between the sides, the paired Student's t-test was used. For the comparisons between evaluations by the F-test (ANOVA) for repeated measures and in case of significant differences according to the F-test (ANOVA), Bonferroni's multiple comparison tests were used. As a way of estimating the population mean for each variable and each assessment, confidence intervals were obtained for the mean of the measurements and the differences between assessments in the variable mean of the sides.
The choice of statistical tests was due to verification of data normality assessed by the Shapiro–Wilk test.
The tests were selected based on the 5% significance level, and the intervals were obtained with 95% confidence. The data were entered into an Excel spreadsheet, and the program used to obtain the statistical calculations was the IMB SPSS version 23.
Surgical Technique
The blepharoplasty incision markings were tailored based on each patients’ individual clinical examination. There was no difference in marking or amount of skin removed when we only perform upper blepharoplasty. Markings were drawn with the patient in the upright position leaving approximately 20 mm of skin between the lower edge of the eyebrow and the lid margin [21].
The brow surgical marking took place with the patient in the primary gaze position. An imaginary line was drawn with a ruler that went from the wing of the nose and passed through the mid-pupillary line to the lower edge of the eyebrow, where a point was marked, and from this point, another point was marked 10-mm laterally. Anesthesia was subcutaneous anesthetic infiltration with 2.0% lidocaine hydrochloride with vasoconstrictor (adrenaline 1:200,000). After excising the skin to expose the orbicularis muscle, the visible portion of this muscle extending from the most lateral aspect of the incision to the lateral limbus (an area approximately 2-cm wide by 1-cm high) was excised with scissors, leaving behind a residual cuff of orbicularis muscle measuring 2–3 mm in height at the upper edge of the wound. A dissection in the plane just deep to the orbicularis oculi muscle was further extended temporally to release the orbital retention ligament, sectioned in its most inferior extension between the lateral canthal tendon and the zygomatic frontal suture. A cephalic dissection with Stevens scissors was performed in a plane below the orbicularis cuff to disinsert the anterior and posterior leafs of the deep galea from their attachment at the arcus marginalis. Scissors were inserted in the plane between the periosteum and the posterior galea leaf, and a vertical spreading motion was used to lift the ROOF pad and associated deep galea off the periosteum, thus avoiding sectioning the motor nerves [4]. A suture with 5-0 nylon thread was placed from the skin through the entire plane of the dissection flap at the level of the marking point of the lower edge of the eyebrow. This thread was then fixed in the periosteum and adjacent tissue 10 mm above the orbital rim as measured with a caliper. The suture was then passed through the subcutaneous plane of the eyebrow at the level of the previously passed transcutaneous suture. This transcutaneous suture was withdrawn, and the remaining suture knot approximated the subcutaneous tissue to the periosteum above the orbital rim. The same procedure was repeated at the other point marked on the eyebrow. The technique was completed with two sutures on the lower border of the superior division of the temporal orbicularis muscle in the orbital rim (arcus marginalis) with 5-0 Vicryl, known as brassiere's sutures. This procedure ended with the usual suture of the blepharoplasty skin with 6-0 nylon. Figure 1 demonstrates the illustration scheme with the surgical technique and Fig. 2 intraoperative photographs highlighting the principal steps of the technique.
Surgical technique illustration. a Surgical marking. b Marking the orbicular muscle to be removed. c Extirpation of the temporal brow depressor muscle (lateral orbital orbicularis oculi—green arrow), leaving behind a residual cuff of orbicularis muscle (white arrow). d Release of deep retaining ligaments of the brow. e Cephalic dissection approaching the orbital rim and the frontal bone. f Periosteum marking 10 mm above the orbital rim. g A suture with 5-0 nylon thread placed from the skin through the entire plane of the dissection flap at the level of the marking point of the lower edge of the eyebrow. h Fixation of the thread in the periosteum and adjacent tissue. i Suture passed through the subcutaneous. j Withdrawn of the transcutaneous suture and knot approximating the subcutaneous tissue to the periosteum. k Fixation of orbicularis cuff to rim with Vicryl suture. l Skin suture
Intraoperative external photographs demonstrating surgical technique. a Extirpation of the temporal brow depressor muscle (lateral orbicularis oculi—green arrow), leaving behind a residual cuff of orbicularis muscle (white arrow). b Release of deep retaining ligaments of the brow. c A suture with 5-0 nylon thread placed from the skin through the entire plane of the dissection flap at the level of the marking point of the eyebrow. d Fixation of the thread in the periosteum and adjacent tissue. e Passed the suture through the subcutaneous at the level of the transcutaneous suture and withdrawned this (transcutaneous) suture afterwards. f Fixation of orbicularis cuff to rim highlighting the principal steps
Results
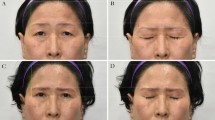
Table 1 shows the means and standard deviations of the eyebrow height measurements. A significant difference between the evaluations is proved, with differences between each pair of evaluations being verified. The highest elevation value was 4.1 mm, and the lowest value was 1.7 mm at the 3-month postoperative period. The height difference between the sides in the same patient did not exceed 1 mm at the 3-month postoperative evaluation (Fig. 3).
There was no dissatisfaction of the patients in relation to the appearance and contour of the eyebrows. One patient experienced mild lagophthalmos (2 mm) in one eye during the immediate postoperative period, and this resolved within 2 days. Figure 4 shows preoperative and 30-day and 90-day postoperative photos of patients with mild (a) and moderate (b) eyebrow ptosis.
Discussion
This study presents the results of the combination of minimally invasive techniques of internal pexy, fixation of the fat pad of the eyebrow, weakening of the orbicularis muscle, and release of the orbital ligament in a single surgical procedure.
In our study, the average lateral eyebrow elevation (3.33 mm) was significant and, moreover, apparently higher than the average eyebrow elevation in studies that evaluated minimally invasive techniques separately. Baker et al. [13] showed that the internal suture of the eyebrow pexy prevented eyebrow drooping, with a lateral elevation of 1.3 mm (right eye) and 0.9 mm (left eye). Authors such as Armstrong et al. [4], using the technique of internal eyebrow pexy, achieved an average lateral elevation of the eyebrow of 2.29 mm, while Broadbent et al. [15] achieved an average of 2.54 mm.
In the eyebrow fat pad fixation technique, the main focus is to elevate and suspend this pad, creating a barrier for the brow fat to descend, projecting it anteriorly (a form of volume increase) [16]. One of these well-known techniques is the brassiere suture. There is no consensus in the literature on the amount of brow lift in this technique. It is most often used to add a fuller, more youthful contour to the lateral brow [16].
Armstrong et al. [14], studying the weakening of the lateral orbicularis muscle associated with the internal pexy technique, achieved an average elevation of the eyebrow tail of 2.42 mm with improvement in symmetry, volume, and eyebrow contour [4]. This removal of the orbicularis muscle will reduce crow’s feet [17] and is kept in an area considered safe to avoid injury to frontal branch innervation, which according to de Bonnecaze et al. [22] is found up to 15.64–16.20 mm behind the lateral orbital rim.
Several authors have noted the importance of releasing the orbital ligament for lateral eyebrow rejuvenation [23]. This ligament works as a retainer, preventing the frontal temporal muscle from raising the eyebrow. For this reason, its release will provide greater mobility of the area, thereby resulting in a greater elevation effect in the technique employed [17].
When we compared the position of the eyebrow in patients who underwent isolated upper blepharoplasty, we found that authors demonstrated contradictory results. Several papers reported no change in eyebrow position after isolated blepharoplasty [24,25,26], while more recent works reported a change in the position of the eyebrow following the same procedure. Lee et al. [9] demonstrated that the distance between the margin of the upper eyelid and the eyebrow was shortened after upper blepharoplasty, which could cause depression of the eyebrow [9], while Prado et al. [10] demonstrated that the correction of redundant tissues in the upper eyelid can accentuate the tendency for the eyebrow to descend, especially in its lateral portion [10].
External brow lift, which is another comparison technique for eyebrow lift, has had lateral lift averages of 2.97 mm [27]. However, this technique has the disadvantage of leaving an apparent scar that, in some cases, can be unsightly, leading to patient dissatisfaction.
A major concern that must be mentioned in regard to the results of eyebrow lift surgeries, whether minimally invasive or not, is the duration of the results. In our work, we were able to verify that there was a decrease in the height of the eyebrow when comparing the postoperative period of 1 month with that of 3 months, which remained at 0.12 mm, still an acceptable value that can be considered stable. This may be due to the decrease in edema, which is still present during the 1-month postoperative period but will have subsided during the 3-month postoperative period, thus reducing the anterior projection of the eyebrow tail and also its elevation. The long-term effectiveness of these techniques remains a concern [28].
Our observations showed that there was symmetry in the height of the eyebrow tail when comparing the two sides of each patient’s face (measurements did not exceed a difference of 1 mm between sides of the same patient) in all cases studied. This is due to the fact that all patients already had symmetry in the height of the eyebrows in the preoperative evaluation, as one of the inclusion criteria was a difference in height of the eyebrows not greater than 1 mm in the same patient, as well as the internal fixation of the eyebrow to be performed at a position 10 mm above the orbital rim as carefully measured with a compass. This eyebrow symmetry is necessary given the importance of facial symmetry in defining beauty [29]. Additionally, eyelid asymmetry caused by asymmetrical eyebrows will tend to be more evident postoperatively if the eyebrow level is not corrected [30].
According to the modern concept of the ideal eyebrow contour, the apex of the eyebrow should be in a vertical line directly above the lateral limb, while the medial and lateral ends of the eyebrow are in approximately the same horizontal plane [31]. This contour proportion was observed in the postoperative results of the eyebrows in our study. The tail was held level with the head and just below the peak of the brow lift. No patient dissatisfaction was identified regarding these issues. We know that, in the brassiere technique, the eyebrow becomes more projected and voluminous in its lateral portion and, therefore, adds to a more youthful appearance [16].
The lagophthalmos observed in a patient in the immediate postoperative period occurred only in one eye and measured 2 mm; thus, there were no symptoms of discomfort or ocular irritation. The condition resolved in 2 days without the need for specific treatment. This lagophthalmos can be found in the immediate postoperative period of conventional upper blepharoplasty and can be explained by the swelling of the area caused by anesthetic infiltration and hematoma, which are temporary and fleeting.
This technique proved to be easy to perform, a priori not adding a time-consuming learning curve for surgeons who are not yet familiar with the techniques described separately. For surgeons who already practice these techniques, it will be easier to adapt to a combination of them. The execution time for the technique will depend on the surgeon's practice and is not likely to be high.
Our study had the limitation of a non-extended follow-up, being 90 days. We know that the vast majority of eyelid healing is achieved within the first 3 months after surgery, although a small percentage of this healing may continue for the 1st year. Later studies with a longer follow-up period may confirm whether our findings are persistent. Morphometric studies of the eyebrow will also be important to better assess the contour and aspect of these eyebrows.
Conclusion
This study demonstrated a surgical technique for lifting the tail of the eyebrow through the blepharoplasty incision for the treatment of mild-to-moderate eyebrow ptosis, with significant results in raising the tail of the eyebrow, which remained stable during the study period. This technique minimizes risks, complications, time, and surgical costs, making it an alternative to improve surgical acceptance and esthetic satisfaction in appropriately selected patients, thus facilitating its incorporation into the daily routine of surgeons.
References
Glass LRG, Lira J, Enkhbold E et al (2014) The lateral brow: position in relation to age, gender, and ethnicity. Ophthal Plast Reconstr Surg 30(4):295–300
Knize DM (1996) An anatomically based study of the mechanism of eyebrow ptosis. Plast Reconstr Surg 97(7):1321–33
Real DSS, Reis RP, Feitosa RGF, Garcia EB, Ferreira LM (2016) Clinical classification of brow ptosis. Rev Bras Cir Plást 31(3):354–361
Georgescu D, Anderson RL, McCann JD (2010) Brow ptosis correction: a comparison of five techniques. Facial Plast Surg 26(3):186–92
McCord CD, Doxanas MT (1990) Browplasty and brow-pexy: an adjunct to blepharoplasty. Plast Reconstr Surg 86(2):248–54
Harvey A, Zarem MD (2004) Browpexy. Aesthetic Surg J 24(4):368–72
Massry GG (2012) The external browpexy. Ophthal Plast Reconstr Surg 28(2):90–95
Cohen BD, Reiffel AJ, Spinelli HM (2011) Browpexy through the upper lid (BUL): a new technique of lifting the brow with a standard blepharoplasty incision. Aesthet Surg J 31(2):163–169
Lee JM, Lee TE, Lee H et al (2012) Change in brow position after upper blepharoplasty or levator advancement. J Craniofac Surg 23(2):434–436
Prado RB, Silva-Junior DE, Padovani CR et al (2012) Assessment of eyebrow position before and after upper eyelid blepharoplasty. Orbit Amst Neth 31(4):222–226
Nakra T, Modjtahedi S, Vrcek I et al (2016) The effect of upper eyelid blepharoplasty on eyelid and brow position. Orbit 35(6):324–327
Hassanpour SE, Khajouei Kermani H (2016) Brow ptosis after upper blepharoplasty: findings in 70 patients. World J Plast Surg 5(1):58–61
Baker MS, Shams PN, Allen RC (2016) The quantitated internal suture browpexy: comparison of two brow-lifting techniques in patients undergoing upper blepharoplasty. Ophthal Plast Reconstr Surg 32(3):204–206
Armstrong BK, Sobti D, Mancini R (2016) Partial orbicularis resection for the augmentation of traditional internal brow pexy: the “tuck and rise.” Ophthal Plast Reconstr Surg 32(6):473–6
Broadbent T, Mohktarzadeh A, Harrison A (2017) Minimally invasive brow lifting techniques. Curr Opin Ophthalmol 28(5):539–43
Briceño CA, Zhang-Nunes SX, Massry GG (2015) Minimally invasive surgical adjuncts to upper blepharoplasty. Facial Plast Surg Clin North Am 23(2):137–51
Burroughs JR, Bearden WH, Anderson RL, McCann JD (2006) Internal brow elevation at blepharoplasty. Arch Facial Plast Surg 8(1):36–41
Knize DM (1995) Transpalpebral approach to the corrugator supercilii and procerus muscles. Plast Reconstr Surg 95(1):52–60
Photogrid app. Grade, (2021) Photo app. Available in: www.photogrid.app. Access at: 20 dez. 2021
Rasband WS, Image J. US National Institutes of Health [Internet] (1997) [cited 2019 May 1]. Available from: http://imagej.nih.gov/ij/
Ramella V, Stocco C, Facchin F, Troisi L, Papa G, Arnez ZM (2018) How to make your life easier: blepharoplasty markings with microsurgical clamps. Plastic Reconstr Surg Global Open 6(8):e1873. https://doi.org/10.1097/GOX.0000000000001873
Bonnecaze G, Chaput B, Filleron T, Al Hawat A, Vergez S, Chaynes P (2015) The frontal branch of the facial nerve: can we define a safety zone? Surg Radiol Anat 37(5):499–506
Cook BE, Lucarelli MJ, Lemke BN (2001) Depressor supercilii muscles: anatomy, histology, and cosmetic implications. Am J Surg 17(6):404–411
Starck WJ, Griffin JE Jr, Epker BN (1996) Objective evalua-tion of the eyelids and eyebrows after blepharoplasty. J Oral Maxillofac Surg 54(3):297–302
Frankel AS, Kamer FM (1997) The effect of blepharoplasty on eyebrow position. Arch Otolaryngol Head Neck Surg 123(4):393–396
Fagien S (1992) Eyebrow analysis after blepharoplasty in patients with brow ptosis. Ophthal Plast Reconstr Surg 8(3):210–214
Mokhtarzadeh A, Massry GG, Bitrian E et al (2017) Quantitative efficacy of external and internal browpexy performed in conjunction with blepharoplasty. Orbit 36(2):102–109
Tyers AG (2006) Brow lift via the direct and trans-blepharoplasty approaches. Orbit 25(4):261–5
Mealey L, Bridgstock R, Townsend GC (1999) Symmetry and perceived facial attractiveness: a monozygotic co-twin comparison. J Pers Soc Psychol 76(1):151–158
Mühlbauer W, Holm C (1998) Eyebrow asymmetry: ways of correction. Aesthetic Plast Surg 22(5):366–371
Yalc¸inkaya E, Cingi C, So¨ken H, et al (2016) Aesthetic analysis of the ideal eyebrow shape and position. Eur Arch Oto-Rhino-Laryngology 273(2):305–310
Funding
The authors received no financial support for the research and authorship of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no conflicts of interest with respect to the authorship and publication of this article.
Informed Consent
Consent for publication of the work was received by all authors and co-authors.
Informed Consent
Informed consent regarding the use of patient images.
Human Rights
The study was approved by the Research Ethics Committee, CAAE no. 26796819.5.0000.5532, and registered in the Brazilian Clinical Trials Registry (REBEC) under no. RBR-75n8453 https://ensaiosclinicos.gov.br/rg/RBR-75n8453.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Silva, J.J.X., Vaz, R.T., Ohmuro, M.l. et al. Brow Lift Through The Upper Blepharoplasty Incision: Prospective Clinical Study. Aesth Plast Surg 47, 1851–1858 (2023). https://doi.org/10.1007/s00266-023-03548-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-023-03548-z