Abstract
Purpose
Paediatric long-bone fractures are commonly seen in the emergency department, and diagnosis is usually confirmed by conventional radiographs. This entails exposure to ionizing radiation with its attendant possible carcinogenic and teratogenic effects. Ultrasonography provides a potentially safer diagnostic alternative and may be cheaper, more readily available, and user-friendly. This study aimed to establish the applicability of ultrasound scanning compared with plain radiography in fracture diagnosis.
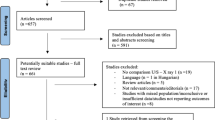
Methods
This prospective observational study documented fracture characteristics using plain radiographs and compared these with findings on ultrasound assessment of same fractures at the time of injury. Scans were repeated at week three and week six to monitor treatment in those whom the mode of treatment did not preclude scanning. Outcome measures were compared for relationships including sensitivity and specificity as well as overall predictive values.
Results
The age range of the 62 subjects enrolled was one to 15 years and the male to female ratio was 1.8:1. Plain radiographs diagnosed 52 fractures and 50 of these were recognized on ultrasound. The two false-negative ultrasound scans were noted in metaphyseal humeral fractures. Overall sensitivity, specificity, and positive and negative predictive values for ultrasonography were 96.2%, 100%, 100%, and 83.3% respectively. Ultrasound scans were also noted to identify callus formation significantly earlier than plain radiographs.
Conclusion
Ultrasound shows potential as a tool in diagnosis of paediatric fractures but may be limited in fractures around metaphyseal bone. Due to the ability to detect callus formation much earlier, ultrasonography may be very useful in monitoring of fracture healing.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Paediatric fractures are a common presentation in the Orthopaedic Emergency Department [1]. Indeed, trauma is the commonest cause of injury and disability in children and young adults worldwide [2, 3]. Diagnosis is typically based on conventional orthogonal radiographs. The World Health Organization estimates that over 75% of the global population have no access to diagnostic imaging services [4]. Plain radiography entails exposure to ionizing radiation which has been proven to be carcinogenic and teratogenic [5] especially in children’s rapidly dividing cells which may be more sensitive to such deleterious effects [6].
Alzen et al. [7] retrospectively studied 2006 radiographs of 1386 children with suspected fractures and found fractures in only 354 of them (17.4%). A review by Bentohami et al. [8] showed that only 50% of injured upper limbs subjected to radiographs had actual fractures. And of the lower limbs, Heyworth et al. [9] showed that radiographs of the ankle were negative for fractures 75% of the time. This high rate of needless exposure to ionizing radiation may be stemmed by the use of ultrasonography in the diagnosis of paediatric fractures. It has also led to the design of several so called “clinical decision rules” (CDRs) [10] which were made to avoid unnecessary radiographs. These CDRs have found application in the ankle as the Ottawa ankle rules and the knee as the Ottawa knee rules [9, 11].
The foregoing has led several investigators to study the applicability of diagnostic ultrasound in the detection of fractures [12, 13]. The reflective acoustic properties of bone improve cortical visualization and make ultrasound imaging highly specific for identifying fractures as small as 1 mm [14]. Ultrasound scanning gives off high-frequency sound waves which have not been found to have deleterious effects to the patient [6]. It is cheaper, portable, less time consuming, and more readily available. Multiple views of the fracture can be derived without additional risk. Point of care scanning can also be made available by a clinician with basic experience in musculoskeletal ultrasound scanning [15] thus eliminating the need for patient transportation to the radiology department. Indeed, there is increasing use and proficiency of ultrasonography in multiple specialties outside radiology [16]. This study aimed to assess the applicability and accuracy of ultrasound scanning in detection of fractures in comparison with plain radiographs.
Materials and methods
This was a prospective observational study conducted between September 2016 and June 2017. Ethical approval was obtained from the Ethics and Research Committee of the institution.
Paediatric subjects aged 16 years and below presenting with acute extremity injuries were recruited and the study population was derived from a convenience sample of subjects. Those who had open or life/limb-threatening injuries were excluded.
Following routine rapid assessment of subjects with suspected fractures using standard algorithms including history, examination, and provisional splintage, those meeting the selection criteria had written informed consent taken from their caregivers. An emergency scan was then carried out on the subject by the radiologist using a standard ultrasound scan machine (TOSHIBA Real-time scanner Model TUS-F30) equipped with a 5-MHz linear probe and with the aid of a water-based, hypoallergenic ultrasound gel. The region of the limb with a suspected fracture was examined longitudinally looking out for the primary outcome measures including, the presence of a fracture seen as soft tissue changes, haematoma collections, periosteal lesions, or break in bone continuity; location of fracture and mal-alignment as well as need for reduction. Findings were documented in a proforma and if multiple bones belonging to the same subject were examined, each bone was considered individually and recorded on a separate form.
The subject thereafter underwent standard radiographic imaging to check for fracture lines, displacement, and angulation if present. A radiologist who was blinded to the ultrasound findings studied the radiographs and recorded the findings. The subjects’ pain scores were assessed and recorded during both procedures using the Wong-Baker FACES pain scale [17]. The duration of both studies was also recorded. Clinical decisions taken thereafter were based on the diagnosis derived from the radiographic assessment. Ultrasound findings were then compared with radiographic images obtained afterwards to determine the sensitivity, specificity, and false-positive and false-negative rates. Subjects thereafter had standard treatment as appropriate for the detected injury. Repeat scans were carried out at three weeks and at six weeks post injury. The data obtained from the study was subjected to statistical analysis using the Statistical Package for Social Sciences (SPSS) software for windows version 21 (SPSS Inc., Chicago, IL, USA).
Results
A total of 62 subjects were recruited for this study with a mean age of 5.62 ± 1.61 years and a male to female ratio of 1.8:1. Only 52 fractures were diagnosed on plain radiographs, giving a fracture prevalence of 83.9%. The most frequently injured bone was the humerus in 19 (30.6%) cases; however, the most injured limb segment was the forearm with both the radius and ulna contributing 20 (32.3%) cases. Majority of the injuries were as a result of falls during play activities 28 (45%), while the sporting injuries accounted for the least number of limb injuries with seven (11%) cases.
Of the 52 fractures seen on plain radiography, 50 were diagnosed on ultrasound. Both missed fractures were in the humerus. Identification of fracture location was equal in the other bones for both imaging modalities. Mean fracture displacement, angulation, investigation duration, and pain scores for both imaging modalities are shown in Table 1. There is significant agreement between plain radiographs and ultrasound in detecting the location of fractures as either diaphyseal or metaphyseal using the Fischer’s exact test (p = 0.001). There were however false-negative ultrasound results for two metaphyseal humeral fractures. Of the 62 bones imaged, plain radiographs identified 14 fractures requiring reduction while ultrasound identified 23 of such fractures (p = 0.000).
This study found an overall sensitivity of 96.2% and a specificity of 100% for ultrasonography in fracture diagnosis. The overall positive and negative predictive values were 100% and 83.3% respectively. Values for individual bones were also tested and are displayed in Table 2. Sensitivity was lower in the diagnosis of metaphyseal humeral fractures (85%) and the negative predictive value was 75%.
Follow-up imaging at week three, demonstrated ultrasound superiority in early detection of callus with visible callus in 30 out of 31 scanned bones, while plain radiography was only able to detect callus in 13 of 31 bones. Other characteristics are displayed in Table 3.
Figure 1a, b depicts the lateral and antero-posterior plain radiographic images of a 7-year-old boy with a supracondylar humeral fracture seen as an oblique cortical discontinuity (solid arrow) with displacement on the day of injury. Figure 1c shows the ultrasonographic image of the fracture seen as a cortical disruption (solid arrow) with displacement. Also seen is a peri-articular hypoechoic collection suggestive of a lipohaemarthrosis (line arrow) with elevation of the posterior fat pad. Figure 1d is the follow-up plain radiograph of the same fracture done at three weeks in a splint, while Figure 1e is the corresponding ultrasonographic image. Gradual obliteration of the fracture line is seen in both images (arrows). Figure 1f, g is the follow-up radiographs done following splint removal at six weeks. Fracture is seen to have united with sclerosis at previous fracture site and no visible fracture line. Figure 1h demonstrates the ultrasound findings at week six with bridging callus demonstrated as cortical expansion across fracture site (line arrow). The growth plate is now visible (solid arrow) following resolution of the surrounding lipohaemarthrosis.
a, b Lateral and antero-posterior plain radiographic images with a supracondylar humeral fracture seen as an oblique cortical discontinuity (solid arrow). c Same fracture seen as a cortical disruption (solid arrow) on ultrasound. d Follow-up plain radiograph at 3 weeks. e Corresponding ultrasonographic image. f, g Follow-up radiographs done following splint removal at 6 weeks. h Ultrasound findings at week 6 with bridging callus demonstrated as cortical expansion across fracture site (line arrow); growth plate (solid arrow)
Figure 2a shows the plain radiographic image of a radius and ulnar fracture in a nine year-old boy taken on the day of injury. Fracture appears as a cortical discontinuity (arrow) with antero-medial angulation. Figure 2b shows the ultrasonographic image of the same fracture taken on the day of injury. Fracture depicted as a cortical disruption with axial deviation (arrow). Figure 2c is the plain radiograph of the same fracture taken at three weeks in a splint. It shows a reduced fracture with a hazy residual fracture line (arrow) representative of progressive healing. Figure 2d shows the ultrasonographic image derived at week three with callus formation seen as area of cortical expansion across the fracture site (solid arrow). Residual fracture line also noted (line arrow). Figure 2e, f is plain radiographs of the forearm fracture at six weeks with the splint still in place. Callus formation is noted (opacity depicted by arrow) around the hazy fracture line. Figure 2g demonstrates the ultrasound image of the same fracture at six weeks with clear bridging callus (arrow) and no residual fracture line.
a Forearm fracture on the day of injury; cortical discontinuity (arrow) with antero-medial angulation. b Corresponding ultrasound image. Cortical disruption with axial deviation (arrow). c Plain radiograph of the same fracture taken at 3 weeks in a splint. d Ultrasonographic image derived at week 3 with callus formation seen as area of cortical expansion across the fracture site (solid arrow); residual fracture line also noted (line arrow). e, f Forearm fracture at 6 weeks with the splint still in place. g At 6 weeks with clear bridging callus (arrow) and no residual fracture line
Figure 3a shows a distal tibia fracture on lateral and antero-posterior plain radiographs taken for an 11-year-old girl on the day of her injury. Cortical discontinuity is depicted by an arrow. Figure 3b shows the ultrasound image of the fracture on the same day, seen as a cortical breach with mal-alignment (arrow). Figure 3c shows the follow-up radiographic image of the same fracture taken in a splint after six weeks. Attempt at healing as evidenced by blunting of the fracture line and relative sclerosis (arrow) is seen. However, fracture line still persists. Figure 3d on the other hand shows bridging of the fracture by callus after six weeks of injury on the ultrasonographic image.
a Distal tibia fracture on lateral and antero-posterior plain radiographs on the day of her injury. b Cortical breach with mal-alignment (arrow). c Follow-up radiographic image of the same fracture taken in a splint after 6 weeks. d Bridging of the fracture by callus after 6 weeks of injury on the ultrasonographic image
Clinical and radiographic outcomes assessed using indices of healing noted during follow-up including absence of pain, full weight bearing, range of motion, callus formation, and restoration of alignment demonstrated satisfactory healing in all the subjects admitted into this study.
Discussion
Childhood trauma remains a global challenge estimated by the World Health Organization to be the commonest cause of injury and disability in children and young adults worldwide [2, 3]. Rapid and safe diagnosis allows for early institution of management to prevent untoward life or limb-threatening complications especially in the paediatric age group with their known peculiarities. Findings from this study suggest that ultrasound scans may provide such an option in fracture diagnosis. Comparison between ultrasound scans and conventional radiographs as a reference also shows significant agreement between both modes of imaging.
Injuries in the humerus, fibula, and tibia accounted for all the negative radiographs in this study. Injuries around the elbow and ankle present a diagnostic challenge during assessment and imaging. Mechanism of injury as well as clinical findings of pain and swelling may strongly suggest a fracture even in the absence of a fracture [8, 9]. This may result in higher negative radiographs being ordered as demonstrated by this study. The need to avoid unnecessary radiographs and ensure uniformity of treatment has led to the development of several workable evidence-based clinical decision rules (CDRs) and appropriate use criteria (AUCs) [18].
Humeral metaphyseal fractures accounted for the two false-negative ultrasound scans. Sinikumpu et al. [19] noted difficulties in the diagnosis of distal humeral fractures, particularly lateral condylar fractures using plain radiographs. This was attributed to the largely cartilaginous nature of the region and the postero-lateral orientation of the fracture line. Metaphyseal fractures are known to be difficult to diagnose on ultrasound because the curved and irregular contour at the bone ends as well as the presence of growth plates may distort the acoustic waves and generate a blurred reflected signal [20]. False negatives may also occur when interpreting cortical irregularities at places with tuberosities, bends, or reactive degenerative changes [21]. All these may obscure the image produced. Rabiner et al. [22] utilized the elevation of the posterior fat pad or lipohaemarthrosis as demonstrated on ultrasonography as a pointer to distal humeral fracture diagnosis. They recorded a sensitivity and specificity of 98% and 70%, respectively, for ultrasound diagnosis of fractures. Fat pad elevation is better seen on ultrasound than in plain radiographs where it can be observed in two regions: (i) posterior or olecranon and (ii) anterior, formed by the coronoid and the supinating pad [23] (Fig. 1c). It can be looked out for during scans of the distal humerus as a pointer to fractures. Shaft fractures appear easier to diagnose as evidenced by the excellent agreement recorded between ultrasound and plain radiographs in diagnosis of diaphyseal fractures [24]. Fractures appear as steps, cortical gaps or interruptions, axial deviations, periosteal lesions or irregularities, haematomas, and soft tissue changes. Ultrasonography can also be useful in the identification of persistently entrapped intra-articular fragments within the elbow joint which may induce articular surface damage, and tend to be associated with poorer clinical and functional outcomes as noted by Canavese et al. [25]. The use of ultrasound scans has also been applied to relatively rare fractures such as those affecting the sternum. Schulzdorst et al. [26] noted that the mechanism of such fractures should prompt immediate examination of the mediastinal structures for associated injuries. Some of these potentially life-threatening associated injuries may be detected on ultrasound.
There was some discordance between values obtained in measurement of fracture displacement and angulation. Williamson et al. [13] suggested that the degree of cortical disruption was more apparent on ultrasound than on plain radiographs. This agrees with what was noted in this study with displacement by ultrasound being almost twice that measured by plain radiographs. Reasons for this may include the fact that conventional plain radiographs are two-dimensional studies which are prone to errors resulting from bone overlap in the frontal plane. The ultrasound scans are able to see bone fragments as distinct from each other with the mobility of the probe giving a more representative view in different planes. However, ultrasound may overestimate fracture displacement and angulation due to the limited view of the entire length of the bone during scanning. On the other hand, plain radiographs give access to the entire length of the bone and thus a more objective assessment of these variables. Accurate assessment of displacement is especially important in areas where prognosis is directly affected, as noted in recent studies on treatment outcomes of pediatric femoral neck fractures [27, 28] which observed an increased risk of developing avascular necrosis of the femoral head with increasing degrees of displacement. Ultimately, a clearer view of displacement will aid satisfactory fracture.
Inter-observer accuracy between experienced and novice sonologists may also be responsible for discrepancies. In this study, all the scans were performed by trained sonologists. Several studies have compared variations in reports by different cadres of sonologists and found no significant difference in their output [21, 29]. Waterbrook et al. [21] used sonologists ranging from a fourth-year medical student to an attending physician during their study. All the sonologists received a 15-minute in-service briefing on point of care ultrasound scans. The inter-observer accuracy at the end of the study was 96.4%. This suggests that the experience of the sonologist is not an overwhelmingly important factor in identification of fractures.
Several studies have noted that ultrasonography is well tolerated in children [6, 30]. Marin et al. [30] noted that ultrasound is the “ideal diagnostic tool in children”. Anxiety of both the patient and the caregiver is an issue in management of childhood injuries. In this study, the application of the gel and the visual distraction provided by the images on the monitor seemed to calm the children down.
The interpretation of the finding in this study of an overall sensitivity of 96.2% and a specificity of 100% as well as an overall positive and negative predictive values were 100% and 83.3%, respectively; in fracture, diagnosis could be that ultrasound scans are better to rule out fractures rather than to “rule in” fractures. This was corroborated by Rabiner et al. [22] in their study of accuracy of point of care ultrasonography in the diagnosis of elbow fractures in children where they found a sensitivity of 70% and a specificity of 93%. Ability to detect the presence of fractures is reduced at the metaphyseal ends of bones. This is clearly demonstrated in this study by the fact that both false-negative ultrasound scans occurred with elbow injuries. Curved and irregular bones give off distorted reflected echoes and confusing images which may lead to low sensitivity in those areas. However, in studies that focused mainly on diaphyseal fracture diagnosis, much higher specificities were noted. Waterbrook et al. [21] noted a sensitivity of 90.2% and a specificity of 96.1% while Williamson [13] in his study had a 100% agreement between plain radiographs and ultrasound. A systemic review by Joshi et al. [31] concluded that compared with radiography, ultrasound is an accurate diagnostic test to rule in or rule out extremity fractures while conceding that the anatomical location of the injury affects the accuracy of the operating characteristics of ultrasound.
Thirty-one patients were found to be suitable for week three and week six follow-up imaging. Ultrasonography was noted to identify the presence of callus earlier than plain radiographs. A significant number of patients at three weeks had no visible callus on plain radiographs with clear fracture lines when compared with ultrasound where attempts at healing were noted earlier. This adds to the possible applications of ultrasonography in fracture monitoring. This property has already been described in the study by Moed et al. [32] which was done in adults. As such, ultrasonography can be employed even in monitoring of adult fractures to determine the need for early intervention in terms of dynamization, autogenous bone grafting, or exchange nailing. It can also assist in decision making regarding early weight bearing and progression to graded activities. Ultrasonography will be used as a screening tool in the emergency room as well as during follow-up without the use of radiographs.
Conclusion
Overall, ultrasound shows promise as a useful, cheap, portable, and versatile alternative to plain radiography in the diagnosis of paediatric long-bone fractures. Ultrasonography will be used as a screening tool in the emergency room as well as during follow-up without the use of radiographs. Protocols will also be developed to incorporate ultrasonography in the initial assessment of childhood trauma. This will lead to a drastic reduction of unnecessary plain radiograph requests. The value of ultrasonography in the diagnosis and monitoring of fracture treatment should be studied further.
References
Adesunkanmi AK, Oginni LM, Oyelami AO, Badru OS (1998) Epidemiology of childhood injury. J Trauma Acute Care Surg 44(3):506–511
Alpern ER, Stanley RM, Gorelick MH, Donaldson A, Knight S, Teach SJ et al (2006) Epidemiology of a pediatric emergency medicine research network: the PECARN Core Data Project. Pediatr Emerg Care 22(10):689–699
Marshburn TH, Legome E, Sargsyan A, Li SM, Noble VA, Dulchavsky SA et al (2004) Goal-directed ultrasound in the detection of long-bone fractures. J Trauma Acute Care Surg 57(2):329–332
World Health Organization Report. Essential health technologies strategy 2004–2007; (2003). http://www.who.int/eht/en/EHT_strategy_2004-2007.pdf
Hill CK, Kumar P (2011) Radiation carcinogenesis. In: Encyclopedia of Cancer, pp 3134–3137
Barata I, Spencer R, Suppiah A, Raio C, Ward MF, Sama A (2012) Emergency ultrasound in the detection of pediatric long-bone fractures. Pediatr Emerg Care 28(11):1154–1157
Alzen G, Duque-Reina D, Urhahn R, Solbach G (1992) Radiographic examination of injuries in children. Clinical and legal considerations about indications. Dtsch Med Wochensch 117(10):363–367
Bentohami A, Walenkamp MM, Slaar A, Beerekamp MS et al (2011) Amsterdam wrist rules: a clinical decision aid. BMC Musculoskelet Disord 12(1):238
Heyworth J (2003) Ottawa ankle rules for the injured ankle. Br J Sports Med 37(3):194–194
McGinn TG, Guyatt GH, Wyer PC, Naylor CD et al (2000) Evidence-based medicine working group. Users’ guides to the medical literature: XXII: how to use articles about clinical decision rules. JAMA 284(1):79–84
Stiell IG, Greenberg GH, Wells GA, McDowell I et al (1996) Prospective validation of a decision rule for the use of radiography in acute knee injuries. JAMA 75(8):611–615
Hubner U, Schlicht W, Outzen S, Barthel M et al (2000) Ultrasound in the diagnosis of fractures in children. JBJS(Br) 82(8):1170–1173
Williamson D, Watura R, Cobby M (2000) Ultrasound imaging of forearm fractures in children: a viable alternative? J Accid Emerg Med 17(1):22–24
Grechenig W, Clement HG, Fellinger M, Seggl W (1998) Scope and limitations of ultrasonography in the documentation of fractures–an experimental study. Arch Orthop Trauma Surg 117(6–7):368–371
Weinberg ER, Tunik MG, Tsung JW (2010) Accuracy of clinician-performed point-of-care ultrasound for the diagnosis of fractures in children and young adults. Injury 41(8):862–868
Levin DC, Rao VM, Maitino AJ, Parker L, Sunshine JH (2004) Comparative increases in utilization rates of ultrasound examinations among radiologists, cardiologists, and other physicians from 1993 to 2001. J Am Coll Radiol 1(8):549–552
Garra G, Singer AJ, Taira BR, Chohan J et al (2010) Validation of the Wong-Baker FACES pain rating scale in pediatric emergency department patients. Acad Emerg Med 17(1):50–54
Ibrahim T, Aldahamsheh OM, Hegazy A, Ghomrawi HM (2018) Applicability of the AAOS appropriate-use criteria for distal radius fractures in surgical practice. Int Orthop 42(1):197–202
Sinikumpu JJ, Pokka T, Victorzon S, Lindholm EL, Serlo W (2017) Paediatric lateral humeral condylar fracture outcomes at twelve years follow-up as compared with age and sex matched paired controls. Int Orthop 41(7):1453–1461
Swischuk LE, Hernandez JA (2004) Frequently missed fractures in children (value of comparative views). Emerg Radiol 11(1):22–28
Waterbrook AL, Adhikari S, Stolz U, Adrion C (2013) The accuracy of point-of-care ultrasound to diagnose long bone fractures in the ED. Am J Emerg Med 31(9):1352–1356
Rabiner JE, Khine H, Avner JR, Friedman LM, Tsung JW (2013) Accuracy of point-of-care ultrasonography for diagnosis of elbow fractures in children. Ann Emerg Med 61(1):9–17
de Neira JZ, Prada-Cañizares A, Marti-Ciruelos R, Pretell-Mazzini J (2015) Supracondylar humeral fractures in children: current concepts for management and prognosis. Int Orthop 39(11):2287–2296
Tsung JW, Blaivas M (2010) Rapid screening for the posterior fat pad sign in suspected pediatric elbow fractures using point-of-care ultrasound a “FAST exam” for the traumatized elbow. Crit Ultrasound J 1(3):111–116
Canavese F, Marengo L, Tiris A, Mansour M et al (2017) Radiological, clinical and functional evaluation using the quick disabilities of the arm, shoulder and hand questionnaire of children with medial epicondyle fractures treated surgically. Int Orthop 41(7):1447–1452
Schulz-Drost S, Oppel P, Grupp S, Taylor D et al (2016) The oblique fracture of the manubrium sterni caused by a seatbelt—a rare injury? Treatment options based on the experiences gained in a level I trauma centre. Int Orthop 40(4):791–798
AlKhatib N, Younis MH, Hegazy A, Ibrahim T (2018) Early versus late treatment of paediatric femoral neck fractures: a systematic review and meta-analysis. Int Orthop:p1–p9. https://doi.org/10.1007/s00264-018-3998-4
Panigrahi R, Sahu B, Mahapatra AK, Palo N (2015) Treatment analysis of paediatric femoral neck fractures: a prospective multicenter theraupetic study in Indian scenario. Int Orthop 39(6):1121–1127
Drakonaki EE, Garbi A (2010) Metatarsal stress fracture diagnosed with high-resolution sonography. J Ultrasound Med 29(3):473–476
Marin JR, Zuckerbraun NS, Kahn JM (2012) Use of emergency ultrasound in United States pediatric emergency medicine fellowship programs in 2011. J Ultrasound Med (9):1357–1363
Joshi N, Lira A, Mehta N, Paladino L, Sinert R (2013) Diagnostic accuracy of history, physical examination, and bedside ultrasound for diagnosis of extremity fractures in the emergency department: a systematic review. Acad Emerg Med 20(1):1–5
Moed BR, Subramanian S, van Holsbeeck M, Watson JT (1998) Ultrasound for the early diagnosis of tibial fracture healing after static interlocked nailing without reaming: clinical results. J Orthop Trauma 1998 12(3):206–213
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval was obtained from the Ethics and Research Committee of the institution.
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Akinmade, A., Ikem, I., Ayoola, O. et al. Comparing ultrasonography with plain radiography in the diagnosis of paediatric long-bone fractures. International Orthopaedics (SICOT) 43, 1143–1153 (2019). https://doi.org/10.1007/s00264-018-4133-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4133-2