Abstract
Supracondylar humeral fractures are the most common elbow fractures in children and represent 3 % of all paediatric fractures. The most common cause is a fall onto an outstretched hand with the elbow in extension, resulting in an extension-type fracture (97–99 % of cases). Currently, the Gartland classification is used, which has treatment implications. Diagnosis is based on plain radiographs, but accurate imaging could be limited due to patient pain. Based on fracture type, the definitive treatment could be either non-operative (type I) or operative (type III/IV); however, when handling type II fractures controversy remains. Neither pin configuration have shown higher efficacy over the other. Complications are ~1 %, the most common being pin migration, with compartment syndrome as the most devastating. Overall, functional outcomes are good, and physical therapy does not appear to be necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Supracondylar humeral fractures (SCHF) are the most common elbow fractures in children, representing 3 % of all paediatric fractures. The incidence between genders is similar due to the increased involvement of girls in sport activities, and children with such injuries have a peak age between five and six years. The annual incidence of these fractures is estimated to be 177.3 per 100,000 children; they have seasonal distribution, being more frequent in the summer months, and occur more often in the left elbow [1]. This article reviews the relevant literature on management, complications and prognosis of SCHF in children.
Anatomy and biomechanics
The elbow is a hinge joint formed by the distal humerus, radial head and the proximal ulna. The distal humerus has two surfaces that articulate with both forearm bones: the capitellum with the radial head, and the trochlea with the articular surface of the olecranon. The elbow is a very complex anatomical area where many structures are related, and they must be well understood by the paediatric orthopaedic surgeon for proper supracondylar fracture management (Fig. 1). Displacements of the proximal and/or distal fracture fragment may compromise any of the elbow structures due to their close anatomical relationship.
Anatomical relationships of neurovascular bundles and supracondylar region. The brachial artery descends superficially by the anteromedial aspect of the brachial muscle, providing deep collateral arteries that run down the anterior aspect of the humerus. The median nerve descends with the brachial artery, the radial nerve runs down the lateral aspect of the humerus between brachialis and brachioradialis and the ulnar nerve runs down the posteromedial aspect through the cubital tunnel of the medial epicondyle
Bone remodelling in the humerus of children between five and eight years of age generates a decrease in the anteroposterior diameter of the supracondylar region, increasing the risk of injury in that region. This region coincides with the two fossae of the distal humerus: olecranon fossa and coronoid fossa. The anterior capsule of the elbow is thicker and stronger than the posterior capsule, and its fibres are under tension during extension, maintaining the olecranon within the olecranon fossa. A collision of the olecranon against the roof of the olecranon fossa and the supracondylar region as a consequence of a fall on an outstretched hand with a hyperextended elbow will result in a fracture in that area [2].
Classification
According to the mechanism of injury, SCHF are classified into two types: extension type (98 %) [3] and flexion type (2 %). In extension fractures, Gartland classification is used to describe the severity of the injury and focus therapeutic management. Such fractures are divided into four types according to the degree of fracture displacement measured in the lateral view on a plain radiograph:
-
Type I:
Fracture is nondisplaced (subtype Ia) or minimally displaced (<2 mm) (subtype Ib) and is associated with an intact anterior humeral line. Because of the intact periosteum circumferentially, these fractures are very stable. The sign of the posterior and/or anterior fat pad may be the only sign of bone injury.
-
Type II:
Fracture presents slight displacement (>2 mm) with a posterior angulation of the distal fragment maintaining the posterior cortex intact (subtype IIa) or when the fracture presents a straight or rotatory displacement with contact between the two fragments (subtype IIb). The anterior humeral line does not cross through the middle third of the capitellum, but there is no rotational instability because the posterior cortex is intact. It is important to pay attention to the disruption of the medial column of the humerus because it can produce varus malalignment. It is important to remember that in comminuted and impacted fractures of the medial column, malrotation can occur in the frontal plane without being appreciated in the lateral plane.
-
Type III:
Fractures have a posteromedial (IIIa) or posterolateral displacement (IIIb) associated with a loss of integrity of the posterior cortex, resulting in extension of the distal fragment on the sagittal plane and rotation in the transverse plane. This creates loss of relationship between anterior humeral line and capitellum and increased risk of neurovascular and soft tissue injury.
-
Type IV:
Fractures with multidirectional instability characterised by complete circumferential tear of the periosteum and instability in flexion and extension [11]. This is not diagnosed by imaging studies but during manoeuvres in the operating room to reduce the fracture. These types of injury can be iatrogenic as a result of reduction of a supracondylar fracture (Fig. 2).
Diagnosis
Physical examination
Pain, swelling, refusal to be examined and—in many cases—an obvious deformity are common symptoms that help in the diagnosis. It is very important to explore the entire extremity to look for other injuries that may go unnoticed; forearm fractures are often associated, increasing the risk for compartment syndrome. Any punctate wound should be considered an open fracture until proven otherwise [3]. During the initial assessment, a thorough vascular examination checking pulses and vascular filling should be performed and repeated after any manipulation of the elbow, because mobilising an elbow with deformity and/or swelling in the antecubital fossa can compromise neurovascular status [2]. A complete neurological exam is important because of the high incidence of nerve injury, the most common being neurapraxia of the anterior interosseous nerve branch of the median nerve, which disables thumb opposition to the second finger (OK sign). If there is severe swelling, uncontrollable pain, bruising or absence of pulses, compartment syndrome should be suspected.
Imaging studies
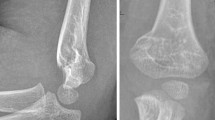
Initial imaging study to diagnose this injury is a plain anteroposterior view of the distal humerus and elbow lateral views. It is very important to radiograph the entire limb, including the ipsilateral wrist and shoulder, as well as the uninjured contralateral extremity in order to compare the two and look for other lesions that may go unnoticed. In many cases, the fracture may go unnoticed, and the fat pad (Fig. 3) could be the only indirect sign [2], which can also be observed in two regions: (i) posterior or olecranon, and (ii) anterior, formed by the coronoid and the supinating pad [2]. Skaggs et al. [4] reported on 35 cases with fat-pad signs, finding that 18 cases (53 %) were supracondylar fractures and the remaining 17 were proximal ulna (26 %), lateral condyle (12 %) or radial-neck (9 %) fractures. In the lateral view of the elbow at 90°, the first thing that should be assessed is the anterior humeral line (Fig. 4a). In extension-type fractures, this line passes through the anterior third of the capitellum. However, this line has no significance in children <four years because it can pass through the anterior third (31 %), middle third (52 %) or posterior third (18 %) of the capitellum without any pathological correlation [5]. Other radiographic measurements are humeral tear, diaphyseal–condylar angle and coronoid line (Fig. 4b, c, d).
Radiographic measurements: a anterior humeral line: an imaginary line running through the anterior cortex of the humerus and must pass through the middle third of the capitellum; b humeral tear: radiologic shadow formed by coronoid fossa, olecranon fossa and upper edge of ossification nucleus with the humeral shaft; c diaphyseal–condylar angle: angle between humeral and humeral condyle axes, which normal value is 30–45°; d coronoid line: imaginary line that continues tangentially, joining the anterior coronoid edge with the front edge of the lateral condyle
Angular relationships measurable on anteroposterior view are Baumann angle [6], metaphyseal–diaphyseal angle and humeroulnar angle (Fig. 5a, b, c).
a Baumann angle: angle that forms the middle diaphyseal humeral line with the epiphyseal line of the lateral condyle; normal values are between 9 and 26°, with the same value for both elbows, and if <9°, indicates varus angulated supracondylar fracture with possible comminution of the medial column; b metaphyseal–diaphyseal angle: angle between midline of the humeral shaft and the line formed between the two furthest points of the widest area of the distal humerus; c humeroulnar angle: formed by two imaginary lines that run through both shafts
Cases in which pain makes it difficult to realise anteroposterior plain radiographs, a Jones projection, where the radiographic beam is directed through the forearm with the elbow in maximal flexion, should be used.
Management
Treatment options for SCHF in children are based on the Gartland classification (Table 1).
Non-operative treatment
Type I fractures are ideal for conservative treatment and are treated with a brachioantebrachial cast at 90° flexion in neutral forearm rotation for three to four weeks. Monitoring is done by serial radiographs on an outpatient basis, paying particular attention to radiographs taken the first week to assess for redisplacement [7, 2, 5]. This treatment is also recommended for patients in whom there is not a clear fracture line but there is a fat-pad sign. Treatment of type II fractures is controversial: Some authors defend a conservative approach to stable type IIA fractures without malrotation and displacement [5, 8]; in this case, parents should be informed about the possibility of surgery if there is redisplacement on subsequent radiographic follow-up. Other authors include all type II fractures in surgical treatment; according to the American Academy of Orthopaedic Surgeons (AAOS) recommendations, surgical treatment for these fractures is consider a moderate recommendation [9].
Operative treatment
General indications
-
Type II:
If such fractures meet any of the characteristics that make them unstable (malrotation, displacement or instability), it is safer to proceed with surgical intervention. The ideal treatment for these fractures is closed reduction and pinning with K wires [2, 5].
-
Type III:
There is a clear consensus that initial treatment should be closed reduction and fixation with K wires [7]. A semisterile technique can be used, implying time savings in the operating room and cost savings [2]. Iobst et al. [10] reported no superficial or deep pin-tract infections requiring treatment in their study of 304 cases managed with this technique.
-
Type IV:
Although these fractures require the most complex management due to instability, initial management must be the same as for types II and III, i.e. closed reduction and pinning with K wires. Leitch et al. recommended preplacement of K wires into the distal fragment before reduction [11].
Operative techniques
The gold standard technique is closed reduction and percutaneous pinning (Fig. 6a, b, c, d) as soon as possible. Acceptable rotation is achieve once the medial and lateral columns are well aligned. The anterior humeral line should pass through the middle third of the capitellum, and the Baumann angle must be restored. Some degree of malrotation can be tolerated, but no varus deformity. In unstable cases, two fluoroscopic machines can be used to maintain fracture reduction [12].
A six year-old boy who fell onto his left outstretched hand resulting in pain and swelling of his left elbow. In the emergency room, plain radiographs showed a Gartland type III fracture: a anteroposterior view; b lateral view. After initial evaluation, the patient underwent closed reduction and pinning using a lateral divergent configuration: c anteroposterior intra-operative fluoroscopic view showing three divergent pins on the lateral aspect of the left distal humerus; d lateral intra-operative fluoroscopic view showing slight flexion of the distal fragment, but with good pin positions
Different pin configurations have been described: two crossed pins; two lateral pins and one crossed pin; only one side pin (usually two or three are used). From a biomechanical standpoint, the greatest resistance to rotation is achieved through a mediolateral crossed-pinning configuration [13]. However, other authors described equivalent torsional rigidity and/or fixation between either three or two lateral pins and crossed pins [14–17]. According to Carter et al. [18] who conducted a survey of 309 paediatric orthopaedic surgeons, the preferred method of percutaneous fixation was fairly evenly distributed between crossed-pin configuration (30 %), two lateral pins (33 %) and three lateral pins (37 %).
Babal et al. conducted a meta-analysis and reported on 5148 patients with 5154 fractures. Overall, incidence rates of iatrogenic ulnar nerve injury ranged from 0 to 6 % [5]. In a systematic review by Slobogean et al. [19], results suggested that there is one iatrogenic ulnar nerve injury for every 28 patients treated with the crossed -pinning configuration compared with lateral pinning. Similarly, Zhao et al. [20] concluded that the crossed-pin fixation carries a higher risk for iatrogenic ulnar nerve injury than the lateral pinning technique. On the other hand, Krusche-Mandl et al. conducted a retrospective study on 78 SCHF and found no ulnar injuries but one iatrogenic radial nerve palsy with crossed pinning. Those authors also found that based on primary nerve injury, there was a significant influence revealing that older patients had a significantly higher risk of such injuries (p = 0.02) [21]. On the basis of these data, it may be suggested that percutaneous crossed pinning carries an increased risk for injury of the ulnar nerve and that lateral pinning should be recommended when suitable.
As medial fixation may be inevitable for certain fracture patterns, several operative techniques have been described to reduce the risk of ulnar nerve injury. Green et al. [22] reported on 62 patients with displaced SCHF who underwent a mini-incision technique to prevent ulnar nerve injury and found no ulnar nerve injuries. This technique demonstrates that crossed-pin configuration can be performed safely and reliably and is an appropriate treatment option for unstable SCHF.
Historically K wires have been used for internal fixation, but due to the potential danger of infection and the need for a second procedure to remove them, alternative options have been described. Fu et al. reported the use of absorbable poly-D,L-lactic-acid pins on 56 cases with irreducible Gartland III fractures through an open approach and found excellent functional and radiologic results, avoiding a second procedure to remove the implants [23]. Even though these results are promising, implant cost is a consideration, as pin removal can be done in the office; the procedure also has a low morbidity rate
Other techniques for stabilising a displaced SCHF have been described, including elastic stable intramedullary nails [24] and external fixator [25, 26], with good functional outcomes. For open reduction, the anterior approach is recommended because it can often be done via a cosmetic incision in the antecubital crease [2, 27] and allows visualisation of the brachial artery and median nerve, if needed.
Evolving operative management concepts
Timing of surgical intervention
Historically, an SCHF continues to be treated as an emergency, even though the outcomes reported in the literature no longer support this practice. Several authors have studied this practice using different cutoff times, such as eight hours [28], 12 h [29] and 21 hours [30]. No differences have been noted regarding perioperative complications [28–30], need for open reduction [28, 30], superficial pin-tract infections [28] or iatrogenic nerve injury [28]. Carter et al. [18] reported that 81 % of respondents preferred to initially splint type III fractures and plan fixation the following morning.
Open fractures: general management principles and surgical approaches
Open SCHF are uncommon. The number of studies on paediatric open fractures in the upper extremity is limited, although it seems clear that they are less frequent than open forearm fractures and usually presented as type I and II, with type III being very infrequently [31], according to Gustilo’s classification [32]. Initial management does not vary from other open fractures in children.
Assessing for the presence of associated injuries (mechanism of injury), status of soft tissues and neurovascular involvement should be the first step when dealing with these type of fractures. Once this is done, tetanus prophylaxis and antibiotic treatment must be administered in the emergency room and radiographs taken. The patient must be taken to the operating room, where under general anaesthesia, wound irrigation and debridement is be performed [33]. The next step is to proceed with closed reduction and fracture fixation, if feasible; however, if this is not possible, an external fixator or open reduction through an anterior approach should be performed [2].
The most common and feared complication of open fractures is infection. The incidence of infection after upper-extremity open fractures is reported to be 0–2.5 %, whereas after type 1 open fractures in children, it is reported as being 1.9 % [31]. A direct correlation of infection rate and patient age has been reported, especially after the age of 12 years [34]. There is no defined antibiotic protocol for such fractures, but usually, a third-generation cephalosporin is used for type I and II open fractures, adding an aminoglycoside for type III open fractures. Vascular and nerve injuries are relatively common in open supracondylar fractures, with an incidence of ~12–20 % [35]. In the case of vascular involvement, quick fracture reduction is mandatory, and if it does not recover, an open approach is required to look for vascular injury. However, nerve injuries recover spontaneously in ~86–100 % of cases [35–37]. Ozkül et al. [38] reported on 26 open supracondylar fractures, finding 15 % (4/26) vascular involvement but vascular repair necessary in only one patient and nerve injury in 34 % (9/26) of cases; complete recovery was seen in all cases. Contrary to other fractures, the rate of wound infection, osteomyelitis, compartment syndrome or Volkman’s ischaemic contracture is considerably lower. An increase in length of hospitalization has also been reported, with a mean duration of 5.4 days (range 3–8) which is longer than in closed fractures (mean 2 days). This could be explained by differences in antibiotic treatment, wound care and additional injuries requiring close monitoring. Regardless of differences in presentation and treatment between open and closed fractures, functional outcome reported in the literature is similar [38].
Pink, pulseless hand
A pink, pulseless hand is one with capillary refill present but radial pulse absent. This situation is one of the most feared by all orthopaedic surgeons due to urgency of treatment, difficulty in managing the vascular injury and lack of a appropriate treatment protocol. In the operating room, the fracture should be reduced with the usual technique and percutaneous pinning, and after 15–20 minutes, neurovascular status should be reassessed. Two different situations may arise depending on the presence or absence of pulse [39, 40]:
-
(1)
If the hand has a good capillary refill (pink), an elbow plaster in 40–60° of flexion should be applied and the elbow monitored intensively.
-
(2)
If the hand does not have good capillary refill, then a vascular examination must be performed, and repair of a damaged vessel is a possible scenario (Fig. 7a, b). In this case, fasciotomies should be considered.
Fig. 7 A seven year-old girl fell on her outstretched left hand resulting in pain and swelling of the left elbow. in the emergency room, plain radiographs were taken showing a a Gartland type III fracture. Because she presented with a pulseless arm, she was was taken to the operating room where closed reduction was performed unsuccessfully, and the hand became pale. b An anterior open approach for reduction was performed; the brachial artery was entrapped within the fracture and was removed successfully, with a subsequent return of pulse
In any case, arteriography should not be performed because it delays fracture reduction and can also cause vasospasm [29]. Although this algorithm is accepted by many authors, other studies promote urgent vascular exploration [41].
Complications
A 1 % complication rate has been reported following SCHF treatment; complications can appear prior to or arising from surgical treatment, with good long-term outcomes [42].
Pin migration/loss of reduction
Pin migration is the most common post-operative complication, reported in up to 2 % of cases [43]; loss of reduction has been reported in 20–30 % of Gartland type II and type III fractures when treated nonoperatively [44, 45]. When surgical treatment has been performed, a 2.9 % of loss of reduction can be expected [46]. Sankar et al. [46] identified three potential technical errors causing loss of reduction: (1) failure to achieve bicortical fixation with two or more pins; (2) failure to achieve adequate pin separation (>2 mm) at the fracture site; (3) failure to pass through both fragments with two or more pins, but no failures were noted when three pins were used [46].
Infection
Few data exist with regard to the incidence of infection associated with sterile or semisterile conditions during which percutaneous pinning of SCHF is performed; however, rates of up to 1 % of superficial infections [10, 43] and 0.2 % of deep infections [43] have been reported. This suggests that an operative approach is safe, and administration of perioperative antibiotics is not indicated [43].
Compartment syndrome
Compartment syndrome is a rare complication that occurs in approximately one to three per 1000 fractures [47] but with very serious consequences. Pain, limb pallor, paresthesia, paralysis and pulselessness are unreliable signs and symptoms of compartment syndrome in children. An increasing analgaesia requirement in combination with other clinical signs, such as agitation and anxiety, is a more sensitive indicator [48]. Ramachandra et al. reported on 11 patients who developed compartment syndrome (all forearm) in association with SCHF. Although theirs was an uncontrolled study, they suggested that delay in initial treatment may have been contributory [37]. If the diagnosis of compartment syndrome has been made, emergent fasciotomy should be performed. Very good results were reported by Bae et al. when fasciotomy was performed within 30.5 hours of injury [48].
Cubitus varus
Cubitus varus is a triplanar deformity consisting of varus angulation in the coronal plane, internal rotation in the axial plane and extension in the sagittal plane. Although cubitus varus has been conventionally described as a cosmetic deformity with little functional significance, there is growing awareness of long-term complications, including chronic pain, ulnar-nerve palsy [49, 50], tardy posterolateral rotatory instability [51], snapping elbow [43] and increased risk of lateral condyle and other secondary fractures [51, 52]. O’Driscoll et al. [51] reported on 22 patients with lateral elbow pain and recurrent posterolateral instability. They observed tardy posterolateral rotatory instability of the elbow that developed approximately two to three decades after SCHF occurred. Mechanical axis, olecranon and triceps line of pull are all displaced medially causing subsequent repetitive external rotation torque on the ulna, which stretches the lateral collateral ligament complex and leads to posterolateral rotatory instability. Reconstruction of the lateral collateral ligament and valgus osteotomy can relieve symptoms of instability. Even in the absence of functional problems, which are mostly late sequelae, parents are often dissatisfied with the appearance of their child’s arm and request treatment. In a meta-analysis conducted by Spencer et al. [53], all surgical treatments performed to correct this deformity, including lateral closing wedge, dome, complex (multiplanar) and distraction osteogenesis, were analysed. The authors found an overall rate of 87.8 % to be good to excellent, but none of the techniques proved to be the safest or most effective. Nerve injury, residual varus and unsightly scarring could be potential complications.
Outcomes
Functional and radiological assessment
Flynn’s criteria are probably the most frequently used tools for assessing functional and cosmetic outcomes in patients with SCHF (Table 2). These criteria allow for clinical evaluation to differentiate between functional outcomes and cosmetic results, since patients with great deformity can have good function and vice versa [8, 54, 55]. However, this scale have some limitations: a loss >15° of motion may be considered as not clinical significant, and elbow hyperextension is a concern for many patients and parents [45, 56]. Alternatively, other scales—such as the Mayo Elbow Performance Score (MEPS) assessing pain, range of motion, stability and ability to perform daily activities [23]; and the Activities Scale for Kids–performance (ASK-p) evaluating functional limitations in daily living activities of patients between 5 and 15 years secondary to musculoskeletal disorders [57]—have been used.
Pain has also been assessed using the visual analogue scale (VAS) of 0–10 to describe minimum and maximum severity of pain, respectively. However, using an 100-point scale is more precise, with less chance of error. This is a generally accepted fact; however, in the paediatric population, children can better handle a “4” or “5” much better than a “42” or “47” difference [58, 59]. With regards to radiological assessment, different measurements have been used, such as Baumann’s angle, diaphyseal–condylar angle and anterior humeral line, all of which are compared pre- and postreduction [15, 55, 21]; however, there is no current consensus that determines the final radiological outcome.
Results
Krusche-Mandl et al. [21] reported on 78 SCHF and found 93.5 % of cases with a satisfactory outcome according to Flynn’s criteria. Similarly, Fu et al. [23] conducted a retrospective study on 56 cases and described a 94.6 % rate of excellent and good outcome according to the MEPS and excellent cosmetic results except for one based on Flynn’s criteria. Based on these results, we can expect a positive outcome when treating SCHF. Spencer et al. [53] performed the largest prospective longitudinal study addressing the recovery of elbow motion in children and found that the highest increases in flexion, extension and absolute and relative arcs of motion were observed early after cast removal, with progressive improvement over time for up to 48 weeks after the original injury. No physical therapy was used in any of patients in that study.
The efficacy of physical therapy in restoring elbow motion after either closed reduction and pinning [57] or open reduction and pinning [60] has been addressed by randomised studies, and they show no benefit.
References
Sutton WR, Greene WB, Georgopoulos G, Dameron TB Jr (1992) Displaced supracondylar humeral fractures in children. A comparison of results and costs in patients treated by skeletal traction versus percutaneous pinning. Clin Orthop Relat Res 278:81–87
Abzug JM, Herman MJ (2012) Management of supracondylar humerus fractures in children: current concepts. J Am Acad Orthop Surg 20(2):69–77. doi:10.5435/JAAOS-20-02-069
Omid R, Choi PD, Skaggs DL (2008) Supracondylar humeral fractures in children. J Bone Joint Surg Am 90(5):1121–1132. doi:10.2106/JBJS.G.01354
Skaggs DL, Mirzayan R (1999) The posterior fat pad sign in association with occult fracture of the elbow in children. J Bone Joint Surg Am 81(10):1429–1433
Ladenhauf HN, Schaffert M, Bauer J (2014) The displaced supracondylar humerus fracture: indications for surgery and surgical options: a 2014 update. Curr Opin Pediatr 26(1):64–69. doi:10.1097/MOP.0000000000000044
Camp J, Ishizue K, Gomez M, Gelberman R, Akeson W (1993) Alteration of Baumann’s angle by humeral position: implications for treatment of supracondylar humerus fractures. J Pediatr Orthop 13(4):521–525
Howard A, Mulpuri K, Abel MF, Braun S, Bueche M, Epps H, Hosalkar H, Mehlman CT, Scherl S, Goldberg M, Turkelson CM, Wies JL, Boyer K, American Academy of Orthopaedic S (2012) The treatment of pediatric supracondylar humerus fractures. J Am Acad Orthop Surg 20(5):320–327. doi:10.5435/JAAOS-20-05-320
Moraleda L, Valencia M, Barco R, Gonzalez-Moran G (2013) Natural history of unreduced Gartland type-II supracondylar fractures of the humerus in children: a two to thirteen-year follow-up study. J Bone Joint Surg Am 95(1):28–34
Mulpuri K, Hosalkar H, Howard A (2012) AAOS clinical practice guideline: the treatment of pediatric supracondylar humerus fractures. J Am Acad Orthop Surg 20(5):328–330. doi:10.5435/JAAOS-20-05-328
Iobst CA, Spurdle C, King WF, Lopez M (2007) Percutaneous pinning of pediatric supracondylar humerus fractures with the semisterile technique: the Miami experience. J Pediatr Orthop 27(1):17–22. doi:10.1097/bpo.0b013e31802b68dc
Leitch KK, Kay RM, Femino JD, Tolo VT, Storer SK, Skaggs DL (2006) Treatment of multidirectionally unstable supracondylar humeral fractures in children. A modified Gartland type-IV fracture. J Bone Joint Surg Am 88(5):980–985. doi:10.2106/JBJS.D.02956
Baratz M, Micucci C, Sangimino M (2006) Pediatric supracondylar humerus fractures. Hand Clin 22(1):69–75. doi:10.1016/j.hcl.2005.11.002
Zionts LE, McKellop HA, Hathaway R (1994) Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. J Bone Joint Surg Am 76(2):253–256
Larson L, Firoozbakhsh K, Passarelli R, Bosch P (2006) Biomechanical analysis of pinning techniques for pediatric supracondylar humerus fractures. J Pediatr Orthop 26(5):573–578. doi:10.1097/01.bpo.0000230336.26652.1c
Lee SS, Mahar AT, Miesen D, Newton PO (2002) Displaced pediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop 22(4):440–443
Hamdi A, Poitras P, Louati H, Dagenais S, Masquijo JJ, Kontio K (2010) Biomechanical analysis of lateral pin placements for pediatric supracondylar humerus fractures. J Pediatr Orthop 30(2):135–139. doi:10.1097/BPO.0b013e3181cfcd14
Kocher MS, Kasser JR, Waters PM, Bae D, Snyder BD, Hresko MT, Hedequist D, Karlin L, Kim YJ, Murray MM, Millis MB, Emans JB, Dichtel L, Matheney T, Lee BM (2007) Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. A randomized clinical trial. J Bone Joint Surg Am 89(4):706–712. doi:10.2106/JBJS.F.00379
Carter CT, Bertrand SL, Cearley DM (2013) Management of pediatric type III supracondylar humerus fractures in the United States: results of a national survey of pediatric orthopaedic surgeons. J Pediatr Orthop 33(7):750–754. doi:10.1097/BPO.0b013e31829f92f3
Slobogean BL, Jackman H, Tennant S, Slobogean GP, Mulpuri K (2010) Iatrogenic ulnar nerve injury after the surgical treatment of displaced supracondylar fractures of the humerus: number needed to harm, a systematic review. J Pediatr Orthop 30(5):430–436. doi:10.1097/BPO.0b013e3181e00c0d
Zhao JG, Wang J, Zhang P (2013) Is lateral pin fixation for displaced supracondylar fractures of the humerus better than crossed pins in children? Clin Orthop Relat Res 471(9):2942–2953. doi:10.1007/s11999-013-3025-4
Krusche-Mandl I, Aldrian S, Kottstorfer J, Seis A, Thalhammer G, Egkher A (2012) Crossed pinning in paediatric supracondylar humerus fractures: a retrospective cohort analysis. Int Orthop 36(9):1893–1898. doi:10.1007/s00264-012-1582-x
Green DW, Widmann RF, Frank JS, Gardner MJ (2005) Low incidence of ulnar nerve injury with crossed pin placement for pediatric supracondylar humerus fractures using a mini-open technique. J Orthop Trauma 19(3):158–163
Fu D, Xiao B, Yang S, Li J (2011) Open reduction and bioabsorbable pin fixation for late presenting irreducible supracondylar humeral fracture in children. Int Orthop 35(5):725–730. doi:10.1007/s00264-010-1018-4
Lacher M, Schaeffer K, Boehm R, Dietz HG (2011) The treatment of supracondylar humeral fractures with elastic stable intramedullary nailing (ESIN) in children. J Pediatr Orthop 31(1):33–38. doi:10.1097/BPO.0b013e3181ff64c0
Slongo T (2014) Radial external fixator for closed treatment of type III and IV supracondylar humerus fractures in children. A new surgical technique. Oper Orthop Traumatol 26(1):75–96. doi:10.1007/s00064-013-0291-y, quiz 97
Slongo T, Schmid T, Wilkins K, Joeris A (2008) Lateral external fixation—a new surgical technique for displaced unreducible supracondylar humeral fractures in children. J Bone Joint Surg Am 90(8):1690–1697. doi:10.2106/JBJS.G.00528
Pretell Mazzini J, Rodriguez Martin J, Andres Esteban EM (2010) Surgical approaches for open reduction and pinning in severely displaced supracondylar humerus fractures in children: a systematic review. J Child Orthop 4(2):143–152. doi:10.1007/s11832-010-0242-1
Mehlman CT, Strub WM, Roy DR, Wall EJ, Crawford AH (2001) The effect of surgical timing on the perioperative complications of treatment of supracondylar humeral fractures in children. J Bone Joint Surg Am 83-A(3):323–327
Gupta N, Kay RM, Leitch K, Femino JD, Tolo VT, Skaggs DL (2004) Effect of surgical delay on perioperative complications and need for open reduction in supracondylar humerus fractures in children. J Pediatr Orthop 24(3):245–248
Bales JG, Spencer HT, Wong MA, Fong YJ, Zionts LE, Silva M (2010) The effects of surgical delay on the outcome of pediatric supracondylar humeral fractures. J Pediatr Orthop 30(8):785–791. doi:10.1097/BPO.0b013e3181f9fc03
Haasbeek JF, Cole WG (1995) Open fractures of the arm in children. J Bone Joint Surg Br 77(4):576–581
Gustilo RB, Anderson JT (1976) Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am 58(4):453–458
Jorge-Mora A, Rodriguez-Martin J, Pretell-Mazzini J (2013) Timing issue in open fractures debridement: a review article. Eur J Orthop Surg Traumatol Orthop Traumatol 23(2):125–129. doi:10.1007/s00590-012-0970-7
Blasier RD, Barnes CL (1996) Age as a prognostic factor in open tibial fractures in children. Clin Orthop Relat Res 331:261–264
Campbell CC, Waters PM, Emans JB, Kasser JR, Millis MB (1995) Neurovascular injury and displacement in type III supracondylar humerus fractures. J Pediatr Orthop 15(1):47–52
Brown IC, Zinar DM (1995) Traumatic and iatrogenic neurological complications after supracondylar humerus fractures in children. J Pediatr Orthop 15(4):440–443
Ramachandran M, Birch R, Eastwood DM (2006) Clinical outcome of nerve injuries associated with supracondylar fractures of the humerus in children: the experience of a specialist referral centre. J Bone Joint Surg Br 88(1):90–94. doi:10.1302/0301-620X.88B1.16869
Ozkul E, Gem M, Arslan H, Alemdar C, Demirtas A, Kisin B (2013) Surgical treatment outcome for open supracondylar humerus fractures in children. Acta Orthop Belg 79(5):509–513
Gillingham BL, Rang M (1995) Advances in children’s elbow fractures. J Pediatr Orthop 15(4):419–421
Sabharwal S, Tredwell SJ, Beauchamp RD, Mackenzie WG, Jakubec DM, Cairns R, LeBlanc JG (1997) Management of pulseless pink hand in pediatric supracondylar fractures of humerus. J Pediatr Orthop 17(3):303–310
Blakey CM, Biant LC, Birch R (2009) Ischaemia and the pink, pulseless hand complicating supracondylar fractures of the humerus in childhood: long-term follow-up. J Bone Joint Surg Br 91(11):1487–1492. doi:10.1302/0301-620X.91B11.22170
Vallila N, Sommarhem A, Paavola M, Nietosvaara Y (2015) Pediatric distal humeral fractures and complications of treatment in Finland: a review of compensation claims from 1990 through 2010. J Bone Joint Surg Am 97(6):494–499. doi:10.2106/JBJS.N.00758
Bashyal RK, Chu JY, Schoenecker PL, Dobbs MB, Luhmann SJ, Gordon JE (2009) Complications after pinning of supracondylar distal humerus fractures. J Pediatr Orthop 29(7):704–708. doi:10.1097/BPO.0b013e3181b768ac
Hadlow AT, Devane P, Nicol RO (1996) A selective treatment approach to supracondylar fracture of the humerus in children. J Pediatr Orthop 16(1):104–106
Parikh SN, Wall EJ, Foad S, Wiersema B, Nolte B (2004) Displaced type II extension supracondylar humerus fractures: do they all need pinning? J Pediatr Orthop 24(4):380–384
Sankar WN, Hebela NM, Skaggs DL, Flynn JM (2007) Loss of pin fixation in displaced supracondylar humeral fractures in children: causes and prevention. J Bone Joint Surg Am 89(4):713–717. doi:10.2106/JBJS.F.00076
Battaglia TC, Armstrong DG, Schwend RM (2002) Factors affecting forearm compartment pressures in children with supracondylar fractures of the humerus. J Pediatr Orthop 22(4):431–439
Bae DS, Kadiyala RK, Waters PM (2001) Acute compartment syndrome in children: contemporary diagnosis, treatment, and outcome. J Pediatr Orthop 21(5):680–688
Abe M, Ishizu T, Morikawa J (1997) Posterolateral rotatory instability of the elbow after posttraumatic cubitus varus. J Shoulder Elb Surg Am Shoulder Elb Surg 6(4):405–409
Mitsunari A, Muneshige H, Ikuta Y, Murakami T (1995) Internal rotation deformity and tardy ulnar nerve palsy after supracondylar humeral fracture. J Shoulder Elb Surg Am Shoulder Elb Surg 4(1 Pt 1):23–29
O’Driscoll SW, Spinner RJ, McKee MD, Kibler WB, Hastings H 2nd, Morrey BF, Kato H, Takayama S, Imatani J, Toh S, Graham HK (2001) Tardy posterolateral rotatory instability of the elbow due to cubitus varus. J Bone Joint Surg Am 83-A(9):1358–1369
Davids JR, Maguire MF, Mubarak SJ, Wenger DR (1994) Lateral condylar fracture of the humerus following posttraumatic cubitus varus. J Pediatr Orthop 14(4):466–470
Spencer HT, Wong M, Fong YJ, Penman A, Silva M (2010) Prospective longitudinal evaluation of elbow motion following pediatric supracondylar humeral fractures. J Bone Joint Surg Am 92(4):904–910. doi:10.2106/JBJS.I.00736
Flynn JC, Matthews JG, Benoit RL (1974) Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J Bone Joint Surg Am 56(2):263–272
Madjar-Simic I, Talic-Tanovic A, Hadziahmetovic Z, Sarac-Hadzihalilovic A (2012) Radiographic assessment in the treatment of supracondylar humerus fractures in children. Acta Inform Med AIM J Soc Med Inform Bosnia & Herzegovina Cas Drustva Med Inform BiH 20(3):154–159. doi:10.5455/aim.2012.20.154-159
de las Heras J, Duran D, de la Cerda J, Romanillos O, Martinez-Miranda J, Rodriguez-Merchan EC (2005) Supracondylar fractures of the humerus in children. Clin Orthop Relat Res 432:57–64
Schmale GA, Mazor S, Mercer LD, Bompadre V (2014) Lack of benefit of physical therapy on function following supracondylar humeral fracture: a randomized controlled trial. J Bone Joint Surg Am 96(11):944–950. doi:10.2106/JBJS.L.01696
Sament R, Bachhal V, Jeph S (2013) Comment on Krusche-Mandl et al.: crossed pinning in paediatric supracondylar humerus fractures: a retrospective cohort analysis. Int Orthop 37(3):557. doi:10.1007/s00264-013-1783-y
Krusche-Mandl I, Aldrian S, Kottstorfer J, Seis A, Thalhammer G, Egkher A (2013) Reply to comment on Irena Krusche-Mandl et al. Crossed pinning in paediatric supracondylar humerus fractures: a retrospective cohort analysis. Int Orthop 37(3):559. doi:10.1007/s00264-013-1784-x
Keppler P, Salem K, Schwarting B, Kinzl L (2005) The effectiveness of physiotherapy after operative treatment of supracondylar humeral fractures in children. J Pediatr Orthop 25(3):314–316
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zorrilla S. de Neira, J., Prada-Cañizares, A., Marti-Ciruelos, R. et al. Supracondylar humeral fractures in children: current concepts for management and prognosis. International Orthopaedics (SICOT) 39, 2287–2296 (2015). https://doi.org/10.1007/s00264-015-2975-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2975-4