Abstract
Purpose
Utilizing ultrasound for the detection of distal forearm fractures in children presents a potential safe and radiation-free alternative compared to X-ray.
Methods
A systematic review was undertaken to compare the diagnostic accuracy of ultrasound in detecting distal forearm fractures in children with X-ray imaging within the period spanning January 2010 to August 2023. The electronic databases MEDLINE and Cochrane CENTRAL were utilized for data retrieval. The QUADAS-2 tool was employed to assess the quality of the included studies. Subsequent statistical analysis was performed to calculate pooled sensitivity and specificity, positive and negative likelihood ratios, as well as the diagnostic odds ratio.
Results
Our meta-analysis included seventeen studies, encompassing a total of 2003 patients, 2546 ultrasound scans, and 1203 fracture cases as identified by the reference test (X-ray). The pooled sensitivity and specificity were 0.96 (95% CI: 0.93–0.98) and 0.96 (95% CI: 0.89–0.98), respectively. The positive likelihood ratio was 13.40 (95% CI: 7.97–21.50), the negative likelihood ratio was 0.06 (95% CI: 0.04–0.1), and the pooled diagnostic odds ratio was 209 (95% CI: 92.20–412.00). Our statistical analysis revealed low heterogeneity within our studied cohort.
Conclusions
Our study indicates that ultrasound exhibits exceptionally high accuracy in the detection of distal forearm fractures in children and adolescents. It can be employed safely to either confirm or rule out a fracture, thus circumventing the need for potentially harmful radiation exposure in this vulnerable population. Future research endeavors should focus on establishing a universally accepted protocol for training and scanning methods to standardize practices and eliminate disparities in diagnostic procedures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
It is well known that distal forearm fractures are the most common fractures in childhood, accounting for 74% of all fractures in the upper limb [1]. The incidence of these fractures has increased in recent years due to increased participation in different and competitive sports, rising rates of overweight children and adolescents, and decreased bone mineral density [2, 3]. Antero-posterior and lateral X-ray views of the injured bone remain the gold standard for the diagnosis of a fracture.
In the last years, there has been growing concern about children’s exposure to ionizing radiation and its potential adverse effects in the future [4]. A correct diagnosis of a fracture typically requires at least two radiographic examinations of the injured area (f + profile views). The number of X-rays may need to be increased if the clinical examination alone is insufficient, especially in young children [5, 6]. Furthermore, radiography has limitations in visualizing unossified and cartilaginous parts of bones in the pediatric population, and alternative diagnostic modalities like MRI or CT scans are either expensive, not always available, or entail additional radiation exposure [7,8,9]. It is also worth noting that only a small fraction of children who present in the emergency room due to accidental injuries will actually have a fracture [10].
The use of ultrasound for diagnosing fractures in children has gained significant attention over the past decade, emerging as a viable alternative [11,12,13]. Moreover, published reviews and studies on the diagnostic accuracy of ultrasound in detecting bone fractures have consistently demonstrated high levels of sensitivity and specificity [14,15,16,17]. Additionally, ultrasound offers several advantages, including real-time assessment at the bedside and the capability to examine multiple planes [18, 19].
As distal forearm injuries are the most common in children, this systematic review focuses exclusively on assessing the diagnostic accuracy of ultrasound for distal wrist fractures in children. By narrowing our scope in this way, we aim to avoid the variability that comes with reviewing diagnostic accuracy across different bone types and mixed populations. We will also collect and analyze information regarding the operator’s training, the ultrasound machine, the type of probe used, the age and gender of the patients, and the scanning method employed for the forearm. Additionally, we will discuss the advantages of using ultrasonography in pediatric orthopedic trauma cases.
Patients and methods
Study design–search strategy–data source
We conducted a systematic literature review to assess the diagnostic accuracy of ultrasound in detecting distal forearm fractures in children, comparing it with conventional X-ray. We utilized the electronic databases Pubmed and Cochrane CENTRAL for our search. This review followed the guidelines and recommendations outlined in PRISMA (Supplemental Material 1) [20]. The terms “ultrasound OR ultrasonography OR diagnostic imaging OR ultrasonics” AND “forearm fracture/injury OR radius fracture/injury OR wrist fracture/injury” AND “children OR child OR pediatric OR juvenile OR adolescent” were scanned. Full details of the search strategy are reported in Supplemental Material 2.
The research aimed to investigate whether ultrasound (index test) is both suitable and accurate in detecting fractures in children and adolescents when compared with X-ray (reference test). The focus was on the distal forearm, as it represents the most common location for fractures in this age group. The title and abstract of potential articles were reviewed for possible inclusion in our analysis. Subsequently, full-text reviews were conducted on articles deemed potentially suitable. Additionally, the bibliographies of the included studies and other systematic reviews were also screened. The initial study selection was carried out by a single author (I.D.). Full-text screening, final decision on inclusion/exclusion, data extraction, quality assessment, and risk of bias assessment were conducted by two authors (I.D. and V.B.). The study protocol was not registered.
Our inclusion and exclusion criteria were as follows:
-
a)
Studies published between January 2010 to August 2023 (to focus on current trends and enhance result reliability).
-
b)
Studies published exclusively in English or German.
-
c)
Studies comparing the diagnostic accuracy of ultrasound (index test) with X-ray (reference test), for distal forearm fractures in children/adolescents. Studies using ultrasound for purposes other than fracture diagnosis (e.g., reduction, treatment without X-ray) were excluded.
-
d)
Studies comparing ultrasound with X-ray in both children and adults were included only if over 50% of the patients were under 18 years old.
-
e)
Studies comparing ultrasound with X-ray in multiple long bones in children were included only if they reported the number of forearm fractures detected by both ultrasound and X-ray.
-
f)
Studies with fewer than 5 patients and case reports were excluded.
-
g)
Editorials, comments, and studies not conducted on humans were excluded.
-
h)
Studies sharing the same population in different journals were excluded.
Data extraction–quality assessment of studies–risk of bias assessment
Data extraction, quality assessment, and risk of bias assessment were conducted by two authors (I.D. and V.B.). From each included study, we gathered the following data: (1) year of publication and the country where the study was conducted, (2) study design, (3) specialty of the sonographer (e.g., emergency doctor, pediatrician, trauma surgeon), (4) sonographer’s training level (untrained, trained, type of training), (5) ultrasound machine used, (6) type of transducer and frequency used, (7) protocol for scanning the forearm (e.g., 6-view, 4-view, longitudinal, transverse planes), (8) sample size, (9) number of ultrasound scans performed, (10) age of the patients, (11) male-to-female ratio, (12) total number of fractures identified, and (13) fractures detected via ultrasound and X-ray (true positive, false positive, true negative, and false negative).
To evaluate the methodological quality of the included studies, we employed the QUADAS-2 tool, designed specifically for assessing the quality of diagnostic accuracy studies [21]. This tool comprises four domains: patient selection, index test, reference standard, and flow and timing. Each domain is evaluated to determine the risk of bias. When it comes to applicability, only the first three domains are considered. For assessing the risk of bias, judgements are categorized as “low,” “high,” or “unclear” based on the responses “yes,” “no,” or “unclear” to the signaling questions (Supplemental Material 3) [21].
Effect measures and synthesis methods
In order to examine the accuracy of ultrasound for the detection of fractures in the distal forearm in children, the authors extracted data in the form of frequencies regarding the four vectors of true positive (TP), true negative (TN), false positive (FP), and false negative (FN) and recorded outcomes in a 2 × 2 table. We thereafter calculated the sensitivity and specificity as TP/(TP + FN) and TN/(FN + FP) and pooled the effect estimates utilizing the logistic-normal bivariate random-effects meta-analysis model (BRMA) and presented outcomes as percentages with their corresponding 95% confidence intervals (CIs) [22]. A formal test for heterogeneity utilizing the I2 statistic by Zhou and Dendukuri was implemented. Outcomes were visualized through forest plots and summary receiver operating characteristics (SROC) plots [23].
Pooled diagnostic odds ratios, defined as the ratio of the odds of a positive test result in subjects with a fracture to the odds of a positive test result in subjects without a fracture, pooled positive likelihood ratios, calculated as the probability of a positive test result in individuals with a fracture divided by the probability of a positive test result in individuals without a fracture, and pooled negative likelihood ratios, computed as the probability of a negative test result in individuals with a fracture divided by the probability of a negative test result in individuals without a fracture, were determined using the sampling-based approach proposed by Zwinderman and Bossuyt [24]. The results were presented as the mean with a 95% CI.
We conducted all statistical analyses using R software (version 4.2.0, R Foundation for Statistical Computing, Vienna, Austria) and STATA statistical software (version 18, Stata Corp LP, College Station, Texas).
Results
Literature search
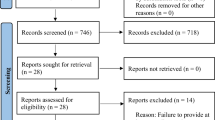
The flow diagram of our study is illustrated in Fig. 1. Initially, 724 studies were identified. After removing duplicates, 657 studies were screened for eligibility. Among the potentially suitable studies, there were 66. Following a thorough review and screening process, 16 studies were included. An additional study was incorporated based on references found within the included studies [32]. In total, our systematic review encompassed 17 studies [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41]. One study was excluded due to insufficient data, making it impossible to construct a 2 × 2 table [42].
Characteristics of the included studies
Within the studies incorporated into our review, a total of 2003 patients presented to the emergency department with potential (distal) forearm fractures. In cases where multiple different long bones were scanned (such as the fibula, tibia, humerus, hand, feet, skull), we considered only the number of patients with distal forearm injuries [25, 29]. In total, 2546 ultrasound scans were conducted. Some studies performed separate ultrasound scans for the radius and ulna [26, 30, 31, 39], while two studies also conducted ultrasound scans on the uninjured forearm [33, 41]. Our systematic review identified 1203 cases of distal forearm fractures, confirmed using X-ray as the gold standard (reference index).
Out of seventeen studies included in our analysis, sixteen are prospective studies, and one is a cross-sectional study [36]. Five studies were conducted in North America (three in the USA and two in Canada) [25, 28, 33, 36, 41], eight in Europe [26, 27, 30, 31, 34, 37,38,39], two in Asia [29, 32], and two in Australia [35, 40]. All of these studies were focused on children with a mean age of 9.8 years (ranging from 2 to 16 years). Only two studies included adults older than 18 years: the first study involved a sub-group of skeletally mature patients aged 18 to 24 years, and another sub-group, where the patients were under 18 years [25]. The second study included patients up to 55 years old, with over 70% of them being under 18 years [32]. Male patients constituted 56% of the study population, while female patients accounted for 44%. Detailed characteristics of each study are summarized in Table 1 and 2.
In all the studies, medium to high-frequency linear transducers (ranging from 7.5 to 15 MHz) were employed, regardless of the varying ultrasound machine types. Furthermore, nearly all studies adhered to a standardized scanning protocol, commonly referred to as the “6-views” of the distal forearm. This protocol includes dorsal, lateral, and palmar views of the radius, along with dorsal, medial, and palmar views of the ulna, as originally described by Ackermann et al. [26]. Only 3 studies did not specify their ultrasound scanning method [27, 29].
Quality assessment of the included studies (QUADAS-2)
We assessed the quality of the included studies using the QUADAS-2 tool, and the results are presented in Fig. 2. There was a moderate to low risk of bias and applicability concerns regarding patient selection, index test, reference test, and flow and timing. It is worth noting that many of the studies were convenience studies, which implies a potential bias in patient selection [25, 28, 29, 35, 36, 38,39,40,41]. All patients enrolled in the studies would normally undergo X-ray evaluation for diagnosing distal forearm fractures. With the exception of one study that used either X-ray or computed tomography as the reference standard [25], all other studies relied on conventional X-ray as the reference standard.
In almost all studies, the sonographers and the radiologists were blinded to each other results. However, in three studies, it remained unclear whether the sonographer was blinded to the X-ray findings, indicating a potential risk of bias [27, 31, 33]. Both examinations were typically performed on the same day or within a short period, typically 2–3 days. Most ultrasound scans were carried out by emergency physicians or pediatric physicians. In three studies, it was unclear who performed the ultrasound examination [26, 27, 30], in one study it was performed by sports medicine doctors [33], in one study (which was finally excluded due to insufficient data, making it impossible to construct 2 × 2 table) by radiologists [42], in another one by nurses [40], and one study had medical students performing the examinations [41]. The level of training across most studies was relatively modest, typically consisting of 30-min to 1 or 2-h lecture training combined with hands-on training (see Table 1). However, in three studies, details regarding the sonographer’s training remained unclear [26, 27, 30].
Among the seventeen studies, fifteen defined ultrasound findings indicative of a fracture, which typically included (i) the presence of any cortical disruption, gap, or displacement and (ii) the presence of any cortical irregularities such as torus formation or bulging. However, 2 studies clearly mentioned that the presence of (subperiosteal) hematoma in most ultrasound views was also considered as an indicator of a fracture [28, 31].
Overall analysis of the diagnostic accuracy of ultrasound for distal forearm fractures in children
In our systematic review, we analyzed 17 studies that compared the diagnostic accuracy of ultrasound in detecting distal forearm fractures in children with X-ray. Figure 3 illustrates the forest plots for sensitivity and specificity. The pooled sensitivity and specificity were 0.96 (95% CI: 0.93–0.98) and 0.96 (95% CI: 0.89–0.98), respectively. Figure 4 presents the HSROC curve, demonstrating the high accuracy of the ultrasound in detecting distal forearm fractures in children when compared to X-ray. The pooled positive likelihood ratio was 13.40 (95% CI: 7.97–21.50), the pooled negative likelihood ratio was 0.06 (95% CI: 0.04–0.1) and the pooled diagnostic odds ratio was 209 (95% CI: 92.20–412.00). Since our systematic review focused on (distal) forearm fractures in children, we expected low heterogeneity. Indeed, we calculated I2 values to assess heterogeneity among the included studies, and they were found to be 38.38% for sensitivity and 39.22% for specificity, indicating low to moderate heterogeneity. The observed heterogeneity can be attributed to various factors. Two studies compared ultrasound to X-ray in pediatric patients, encompassing multiple injury sites [25, 29]. Another study focused on evaluating the efficacy of ultrasound in diagnosing distal radius fractures across all age groups [32]. Additionally, it is well established that ultrasound, as an imaging modality, is highly operator-dependent.
Discussion
This study systematically reviewed the diagnostic accuracy of ultrasound for detecting distal forearm fractures in children. The findings clearly indicate that ultrasound scans of the distal forearm in children following acute trauma can safely serve as the primary diagnostic method.
Advantages of ultrasound in pediatric orthopedic trauma cases
As previously mentioned, there is a growing concern regarding radiation exposure in young children during X-ray examinations. Conducting a clinical examination in young children after trauma is often challenging, and pinpointing the exact location of maximum pain can be particularly difficult [43]. The standard approach involves a minimum of two radiological examinations (f + profile views of the injured area), and in cases of clinical ambiguity, additional bones may need radiographic evaluation [6, 43]. The use of ultrasound as a viable alternative has been proposed in the literature. Ultrasonography offers advantages such as speed, real-time information, bedside applicability, the ability to scan the contralateral limb, and, notably, it is radiation-free [19, 44].
In addition, ultrasound imaging has been found to be less painful when compared to X-rays [28]. The need to reposition the injured limb for X-ray imaging often causes more discomfort for the patient [13]. Furthermore, sonography provides valuable insights into soft-tissue injuries and the condition of unossified bones [7, 45]. One study conducted a cost analysis comparing ultrasound and X-ray [46]. It found that fracture treatment involving ultrasound costs €20.54, whereas treatment involving an X-ray examination costs €26.60, thus concluding that ultrasound usage can result in cost savings [46].
Above all, it is crucial to minimize unnecessary radiation exposure. Child tissues are more radio-sensitive due to their increased mitotic rate, and children have a long life expectancy during which malignancies can develop following irradiation [35, 47, 48]. Ackermann et al. conducted a study on the efficacy of the Wrist SAFE Algorithm in fracture sonography of distal forearm fractures in children and found that 81% of X-rays could be avoided, which translates to a significant reduction of 2.8 million X-ray exposures in G10 member states [49].
Literature regarding the diagnostic accuracy of ultrasound in detecting fractures
Our findings align with previously published reviews. In a meta-analysis by Tsou PY et al., which assessed the diagnostic accuracy of ultrasound for upper extremity fractures in children, a sensitivity of 0.95 (95% CI: 0.93–0.97) and a specificity of 0.95 (95% CI: 0.91–0.98) were reported [14]. It should be mentioned that this meta-analysis encompassed studies involving elbow, humerus, and forearm fractures, not limited to forearm injuries alone [14]. Another systematic review of Schmid GL et al. compared ultrasound with conventional imaging and reported a pooled sensitivity of 0.91 (95% CI: 0.90; 0.92) and specificity of 0.94 (95% CI: 0.93; 0.95) [15]. However, the analyzed studies displayed marked heterogeneity, including adults and various bone types [15]. In a literature review focusing on ultrasound as a triage tool for diagnosing fractures in children (clavicle, metacarpals, metatarsals, forearm, etc.), ultrasound demonstrated a sensitivity of nearly 100% when combined with clinical suspicion of fracture [16].
Douma-den Hamer et al. published a diagnostic meta-analysis on ultrasound for distal forearm fractures, encompassing all age groups [50]. Their findings revealed a sensitivity of 97% (CI 95%, 93–99%) and a specificity of 95% (CI 95%, 89–98%) [50]. In a recent large, prospective, multi-center study focused on the accuracy of ultrasound in detecting fractures in children, high-skill providers (with 18 months of training and at least 200 examinations) demonstrated a sensitivity of 91.67% (95% CI, 76.41–97.82%) and a specificity of 88.89% (95% CI, 73.00–96.34%) [17]. Standard-skill providers (with 6 months training and 50 examinations) exhibited a sensitivity of 71.50% (95% CI, 64.75–77.43%) and a specificity of 82.91% (95% CI, 77.82–87.06%) [17]. It is worth noting that this study introduced heterogeneity to the results, as it examined multiple bone types, including long bones, hands, feet, and the skull [17]. Similarly, another systematic review included heterogeneous studies and concluded that their results do not support replacing radiography with ultrasound for diagnosing extremity fractures (encompassing all extremity fractures) [51]. However, it did acknowledge that ultrasound can be a valid alternative under specific conditions [51].
The previously mentioned reviews are characterized by the inclusion of studies that compared ultrasound’s diagnostic accuracy either across multiple (long) bones within similar age groups or within a specific “injured area” but across different age groups, and sometimes both. In our study, our aim was to minimize heterogeneity as much as possible. Given that distal forearm fractures are the most prevalent in childhood, we sought to include studies that specifically compared the diagnostic accuracy of ultrasound for fractures within this “area” and within this age group (0–16 years old). Under these criteria, we found only one review in the literature, which included just 8 studies [46]. It reported a sensitivity ranging from 64 to 100% and a specificity between 73 and 100%, suggesting indications of comparable diagnostic accuracy between X-ray and ultrasound. However, it emphasized the need for more studies with adequate sample size calculation [46]. Conversely, a review addressing ultrasound in diagnosing pediatric distal radius fractures concluded that ultrasound cannot adequately replace conventional X-rays [52]. It is important to note that this review included only a few studies, lacked statistical analysis, and primarily provided an orthopedic perspective on treatment policy [52].
Methods of scanning–definition of fracture–training
While most studies employ a consistent ultrasound examination protocol for the distal forearm, some variations exist (see Table 1). The six-view method, as described by Ackermann et al., appears to be the most accurate approach [26]. This method involves examining the radius and ulna from the dorsal, lateral, and palmar sides, resulting in a total of six images (2 bones × 3 scans = 6 images) [26]. Some studies focus on scanning the radius only (which increases the risk of overlooking an isolated ulna fracture), and some other studies do not describe the exact method of ultrasound examination or perform the 4-view method instead of the six-view method [27, 34, 41, 53]
Furthermore, there is no unanimous consensus regarding the ultrasound definition of a fracture. While most studies agree that the presence of cortical irregularity or disruption on ultrasound indicates a fracture, some studies also consider the presence of subperiosteal hematoma [28, 31]. Additionally, recent research has explored specific ultrasound signs. For example, a recent study assessed the ultrasound pronator quadratus hematoma sign and found that it effectively distinguished children with and without cortical breach fractures [54]. Another recent study, which evaluated the diagnostic accuracy of ultrasound in children diagnosed with a distal radius fracture on X-ray, measured the fracture-physis distance and suggested that a cutoff of 1 cm differentiated Salter-Harris II fractures from other cortical breach fractures, though not buckle fractures [55].
In nearly all studies, sonographer training comprises a combination of a lecture-based training and hands-on practice. This training duration varies widely, from as short as a 4-min training video [36] to 30-min sessions [31], 1-h sessions [37, 38], or an 80-min online learning module with quiz [35]. These variations indicate minimal emphasis on theoretical training. Hands-on training is similarly minimal, ranging from 30-min practical training [32] to 2-h hands-on training sessions [35] or the requirement to perform at least 20–25 supervised scans [29, 39]. A meta-analysis revealed no significant difference in diagnostic accuracy between trained and untrained personnel, suggesting that ultrasound can be effectively conducted after minimal training [50]. Conversely, in a prospective, multi-center study on the accuracy of ultrasound in detecting fractures in children, high-skill providers (with 18 months training period and at least 200 examinations) demonstrated higher sensitivity and specificity, while standard-skill providers (with 6 months training period and 50 examinations) exhibited lower sensitivity [17]. A recent study described a learning curve for diagnosing pediatric distal forearm fractures using ultrasound [56]. This concluded that a brief training course, coupled with approximately 15 scans, was sufficient [56].
The variations in results among different studies can be attributed to several factors: (a) differences in the definition of fracture, (b) variances in the ultrasound scanning method (whether the six-view or 4-view method was employed), and (c) disparities in sonographer training.
Nevertheless, it is imperative to establish a universal consensus regarding the definition of a fracture based on ultrasound findings, an agreed-upon scanning protocol, and a standardized sonographer training. Future studies should aim to develop globally accepted protocols and guidelines encompassing the aforementioned aspects: fracture definition, scanning methods, and sonographer training. Furthermore, these protocols should undergo critical evaluation for their applicability to different joints or bones. For instance, the complex anatomy of the elbow joint and the variation in ossification centers in children may necessitate distinct ultrasound scanning protocols and methods [14].
It is important to note that the ultimate decision regarding a child’s treatment is contingent upon a combination of clinical assessment and the findings from a diagnostic modality (such as X-ray, ultrasound, or computed tomography). This means that the sonographer may not have the final decision on patients’ treatment. Our study investigates the possibility that the ultrasound may replace the X-ray (under certain circumstances) and should not replace the final judgement of the treating physician.
Strengths and limitations
To the best of our knowledge, our systematic review encompasses the most extensive collection of studies dedicated to assessing the diagnostic accuracy of ultrasound for distal forearm injuries in the pediatric population, totaling 17 studies. Our intention was to minimize heterogeneity in our results to the greatest extent possible, a goal that is evident in Fig. 2 (QUADAS-2-quality assessment of included studies). Our review’s strengths lie in the substantial number of included studies and our efforts to mitigate heterogeneity in the results.
One limitation of our review (which can paradoxically be regarded as a strength) is the exclusion of certain studies that examined the distal forearm with ultrasound across all age groups (including adults) or as part of assessing the diagnostic accuracy of ultrasound in various anatomical regions (such as tibia, fibula, humerus, metacarpals, metatarsals, skull, ribs). Among the seventeen studies, two studies compared ultrasound to X-ray in pediatric patients across multiple injury sites, but they were included in our systematic review because they clearly reported the number of fractures detected by ultrasound and X-ray in the radius and ulna [25, 29]. Additionally, one study assessed the efficacy of ultrasound in diagnosing distal radius fractures across all age groups but was included in our study due to the substantial proportion (72%) of patients under 18 years [32]. That being said, we excluded studies that evaluated the ultrasound’s ability to detect fractures when they did not precisely specify the number of distal forearm fractures found or when the study population consisted of over 50% adults [57,58,59]. This decision may have resulted in the omission of some pediatric distal forearm fractures and introduced a selection bias. However, it likely had a positive impact on the overall quality of our meta-analysis.
Another limitation of our study pertains to the varying levels of experience and training among sonographers, disparities in the definition of a fracture using ultrasound, and differences in scanning methods, all of which have been thoroughly discussed previously. Consequently, the widespread applicability of ultrasound for detecting distal forearm fractures cannot be universally assumed until a consensus is achieved in these areas.
Another limitation to consider is that our study did not investigate the efficacy of ultrasound in diagnosing fractures in other bones or joints. As a result, the findings of our study are specifically relevant to distal forearm injuries in children and adolescents.
Furthermore, we have to acknowledge that all studies included in our analysis focused on patients who arrived at the emergency department with a reported history of distal forearm injury. This introduces the possibility of selection bias since only those patients with a conventional history of injury were included across all studies.
Finally, our exclusion criteria encompassed studies in which patients did not undergo both ultrasound and conventional X-ray examinations, and we restricted our analysis to studies available in English or German. As a result, there is the potential for the omission of relevant studies that did not meet these criteria.
Although full-text screening, final decisions regarding inclusion/exclusion, and quality assessment were conducted collaboratively by two authors (I.D. and V.B.), the initial study selection was performed by a single author (I.D.). The initial screening may have led to some studies being overlooked.
Conclusions
Our systematic review concludes that ultrasonography can safely contribute to the detection of distal forearm fractures in children and adolescents. While it is not intended to entirely replace conventional X-ray examinations, ultrasonography holds the potential to effectively rule in or rule out a fracture. This capability can significantly reduce unnecessary radiation exposure for a considerable number of children who present in the emergency department with potential distal forearm fracture.
Future studies should focus on two critical objectives: (a) establishing a universally accepted protocol for training and scanning methods to eliminate disparities and (b) evaluating the long-term functional outcomes and arm function of children who were treated based on ultrasound findings alone.
Data availability
The dataset used or analyzed during the current study is available from the corresponding author on reasonable request.
References
Korup LR, Larsen P, Nanthan KR, Arildsen M, Warming N, Sorensen S, et al. Children’s distal forearm fractures: a population-based epidemiology study of 4,316 fractures. Bone Jt Open. 2022;3(6):448–54. https://doi.org/10.1302/2633-1462.36.BJO-2022-0040.R1.
Dua K, Abzug JM, Sesko Bauer A, Cornwall R, Wyrick TO. Pediatric distal radius fractures. Instr Course Lect. 2017;66:447–60.
Hedström EM, Svensson O, Bergström U, Michno P. Epidemiology of fractures in children and adolescents. Acta Orthop. 2010;81(1):148–53. https://doi.org/10.3109/17453671003628780.
Linet MS, Kim KP, Rajaraman P. Children’s exposure to diagnostic medical radiation and cancer risk: epidemiologic and dosimetric considerations. Pediatr Radiol. 2009;39(S1):4–26. https://doi.org/10.1007/s00247-008-1026-3.
Metz VM, Gilula LA. Imaging techniques for distal radius fractures and related injuries. Orthop Clin North Am. 1993;24(2):217–28.
Thukral BB. Problems and preferences in pediatric imaging. Indian J Radiol Imaging. 2015;25(4):359–64. https://doi.org/10.4103/0971-3026.169466.
Cho KH, Lee SM, Lee YH, Suh KJ. Ultrasound diagnosis of either an occult or missed fracture of an extremity in pediatric-aged children. Korean J Radiol. 2010;11(1):84–94. https://doi.org/10.3348/kjr.2010.11.1.84.
Mazrani W, McHugh K, Marsden PJ. The radiation burden of radiological investigations. Arch Dis Child. 2007;92(12):1127–31. https://doi.org/10.1136/adc.2006.101782.
Beltrame V, Stramare R, Rebellato N, et al. Sonographic evaluation of bone fractures: a reliable alternative in clinical practice? Clin Imaging. 2012;36(3):203–8. https://doi.org/10.1016/j.clinimag.2011.08.013.
Wolfe JA, Wolfe H, Banaag A, Tintle S, Perez KT. Early pediatric fractures in a universally insured population within the United States. BMC Pediatr. 2019;19(1):343. https://doi.org/10.1186/s12887-019-1725-y.
Schulte-Uentrop L, Goepfert MS. Anaesthesia or sedation for MRI in children. Curr Opin Anaesthesiol. 2010;23(4):513–7. https://doi.org/10.1097/ACO.0b013e32833bb524.
Avci M, Kozaci N, Tulubas G, Caliskan G, Yuksel A, Karaca A, et al. Comparison of Point-of-Care Ultrasonography and radiography in the diagnosis of long bone fractures. Medicina (Kaunas). 2019;55(7):355. https://doi.org/10.3390/medicina55070355.
Cross KP, Warkentine FH, Kim IK, Gracely E, Paul RI. Bedside ultrasound diagnosis of clavicle fractures in the pediatric emergency department. Acad Emerg Med. 2010;17(7):687–93. https://doi.org/10.1111/j.1553-2712.2010.00788.x.
Tsou PY, Ma YK, Wang YH, Gillon JT, Rafael J, Deanehan JK. Diagnostic accuracy of ultrasound for upper extremity fractures in children: a systematic review and meta-analysis. Am J Emerg Med. 2021;44:383–94. https://doi.org/10.1016/j.ajem.2020.04.071.
Schmid GL, Lippmann S, Unverzagt S, Hofmann C, Deutsch T, Frese T. The investigation of suspected fracture – a comparison of ultrasound with conventional imaging. Dtsch Arztebl Int. 2017;114(45):757–64. https://doi.org/10.3238/arztebl.2017.0757.
Iacob R, Stoicescu ER, Cerbu S, Iacob D, Amaricai E, Catan L, et al. Could ultrasound be used as a triage tool in diagnosing fractures in children? A literature review. Healthcare. 2022;10(5):823. https://doi.org/10.3390/healthcare10050823.
Caroselli C, Raffaldi I, Norbedo S, Parri N, Poma F, Blaivas M, et al. Accuracy of point-of-care ultrasound in detecting fractures in children: a validation study. Ultrasound Med Biol. 2021;47(1):68–75. https://doi.org/10.1016/j.ultrasmedbio.2020.09.012.
Javadzadeh HR, Davoudi A, Davoudi F, Ghane MR, Khajepoor H, Goodarzi H, et al. Diagnostic value of “bedside ultrasonography” and the “water bath technique” in distal forearm, wrist and hand bone fractures. Emerg Radio. 2014;21(1):1–4. https://doi.org/10.1007/s10140-013-1161-5.
Azizkhani R, Hosseini Yazdi Z, Heydari F. Diagnostic accuracy of ultrasonography for diagnosis of elbow fractures in children. Eur J Trauma Emerg Surg. 2022;48(5):3777–84. https://doi.org/10.1007/s00068-021-01648-6.
McInnes MDF, Moher D, Thombs BD, McGrath TA, Bossuyt PM; and the PRISMA-DTA Group. Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA. 2018;319(4):388–96.
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–36. https://doi.org/10.7326/0003-4819-155-8-201110180-00009.
Chu H, Cole SR. Bivariate meta-analysis of sensitivity and specificity with sparse data: a generalized linear mixed model approach. J Clin Epidemiol. 2006;59(12):1331–2. https://doi.org/10.1016/j.jclinepi.2006.06.011.
Zhou Y, Dendukuri N. Statistics for quantifying heterogeneity in univariate and bivariate meta-analyses of binary data: the case of meta-analyses of diagnostic accuracy. Stat Med. 2014;33(16):2701–17. https://doi.org/10.1002/sim.6115.
Zwinderman AH, Bossuyt PM. We should not pool diagnostic likelihood ratios in systematic reviews. Stat Med. 2008;27(5):687–97. https://doi.org/10.1002/sim.2992.
Weinberg ER, Tunik MG, Tsung JW. Accuracy of clinician performed point-of-care ultrasound for the diagnosis of fractures in children and young adults. Injury. 2010;41(8):862–8. https://doi.org/10.1016/j.injury.2010.04.020.
Ackermann O, Liedgens P, Eckert K, Chelangattucheryy E, Ruelander C, Emmanouilidis I, et al. Ultrasound diagnosis of juvenile fractures. J Med Ultrason. 2010;37(3):123–7. https://doi.org/10.1007/s10396-010-0263-x.
Pountos I, Clegg J, Siddiqui A. Diagnosis and treatment of greenstick and torus fractures of the distal radius in children: a prospective randomized single blind study. J Child Orthop. 2010;4(4):321–6. https://doi.org/10.1007/s11832-010-0269-3.
Chaar-Alvarez FM, Warkentine F, Cross K, Herr S, Paul RI. Bedside ultrasound diagnosis of nonangulated distal forearm fractures in the pediatric emergency department. Pediatr Emerg Care. 2011;27(11):1027–32. https://doi.org/10.1097/PEC.0b013e318235e228.
Sinha TP, Bhoi S, Kumar S, Ramchandani R, Goswami A, Kurrey L, et al. Diagnostic accuracy of bedside emergency ultrasound screening for fractures in pediatric trauma patients. J Emerg Trauma Shock. 2011;4(4):443–5. https://doi.org/10.4103/0974-2700.86625.
Eckert K, Ackermann O, Schweiger B, Radeloff E, Liedgens P. Ultrasound as a viable alternative to standard X-rays for the diagnosis of distal forearm fractures in children. Z Orthop Unfall. 2012;150(4):409–14. https://doi.org/10.1055/s-0032-1314974.
Herren C, Sobottke R, Ringe MJ, Visel D, Graf M, Müller D, et al. Ultrasound guided diagnosis of fractures of the distal forearm in children. Orthop Traumatol Surg Res. 2015;101(4):501–5. https://doi.org/10.1016/j.otsr.2015.02.010.
Kozaci N, Ay MO, Acimen M, Turhan G, Sasmaz I, Turhan S, et al. Evaluation of the effectiveness of bedside point of care ultrasound in the diagnosis and management of distal radius fractures. Am J Emerg Med. 2015;33(1):67–71. https://doi.org/10.1016/j.ajem.2014.10.022.
Ko C, Baird M, Close M, Cassas KJ. The diagnostic accuracy of ultrasound in detecting distal radius fractures in a pediatric population. Clin J Sport Med. 2019;29(5):426–9. https://doi.org/10.1097/JSM.0000000000000547.
Hedelin H, Tingström C, Hebelka H, Karlsson J. Minimal training sufficient to diagnose pediatric wrist fractures with ultrasound. Crit Ultrasound J. 2017;9(1):11.
Rowlands R, Rippey J, Tie S, Flynn J. Bedside ultrasound vs X-ray for the diagnosis of forearm fractures in children. J Emerg Med. 2017;52(2):208–15. https://doi.org/10.1186/s13089-017-0066-z.
Poonai N, Myslik F, Joubert G, Fan J, Misir A, Istasy V, et al. Point of care ultrasound for nonangulated distal forearm fractures in children: test performance characteristics and patient-centered outcomes. Acad Emerg Med. 2017;24(5):607–16. https://doi.org/10.1111/acem.13146.
Ahmed AS, Abdelhady AE, McNicholl MB. Ultrasound as a diagnostic tool in pediatric distal forearm fractures. Ir Med J. 2018;111(10):836.
Epema AC, Spanjer MJB, Ras L, Kelder JC, Sanders M. Point of care ultrasound compared with conventional radiographic evaluation in children with suspected distal forearm fractures in the Netherlands: a diagnostic accuracy study. Emerg Med J. 2019;36(10):613–6. https://doi.org/10.1136/emermed-2018-208380.
Galletebeitia Laka I, Samson F, Gorostiza I, Gonzalez A, Gonzalez C. The utility of clinical ultrasonography in identifying distal forearm fractures in the pediatric emergency department. Eur J Emerg Med. 2019;26(2):118–22. https://doi.org/10.1097/MEJ.0000000000000509.
Snelling PJ, Jones P, Keijzers G, Bade D, Herd DW, Ware RS. Nurse practitioner administered point of care ultrasound compared with X-ray for children with clinically non-angulated distal forearm fractures in the ED: a diagnostic study. Emerg Med J. 2021;38(2):139–45. https://doi.org/10.1136/emermed-2020-209689.
Zhang J, Boora N, Melendez S, Rakkunedeth Hareendranathan A, Jaremko J. Diagnostic accuracy of 3D ultrasound and artificial intelligence for detection of pediatric wrist injuries. Children. 2021;8(6):431. https://doi.org/10.3390/children8060431.
Akinmade A, Ikem I, Ayoola O, Orimolade E. Adeyeye Comparing ultrasonography with plain radiography in the diagnosis of paediatric long bone fractures. Int Orthop. 2019;43(5):1143–53. https://doi.org/10.1007/s00264-018-4133-2.
Moritz JD. Sonographic fracture diagnosis in children and adolescents. Rofo. 2023;195(9):790–6. https://doi.org/10.1055/a-2042-2161.
Litrenta J, Masrouha K, Wasterlain A, Castaneda P. Ultrasound evaluation of pediatric orthopaedic patients. J Am Acad Orthop Surg. 2020;28(16):e696–705. https://doi.org/10.5435/JAAOS-D-17-00895.
Keller MS. Musculoskeletal sonography in the neonate and infant. Pediatr Radiol. 2005;35(12):1167–73. https://doi.org/10.1007/s00247-005-1550-3.
Katzer C, Wasem J, Eckert K, Ackermann O, Buchberger B. Ultrasound in the diagnostics of metaphyseal forearm fractures in children: a systematic review and cost calculation. Pediatr Emerg Care. 2016;32(6):401–7. https://doi.org/10.1097/PEC.0000000000000446.
Kraus R, Dresing K. Rational usage of fracture imaging in children and adolescents. Diagnostics. 2023;13(3):538. https://doi.org/10.3390/diagnostics13030538.
Little MP, Wakeford R, Borrego D, French B, Zablotska LB, Adams MJ, et al. Leukaemia and myeloid malignancy among people exposed to low doses (<100 mSv) of ionising radiation during childhood: a pooled analysis of nine historical cohort studies. Lancet Haematol. 2018;5(8):e346–58. https://doi.org/10.1016/S2352-3026(18)30092-9.
Ackermann O, Wojciechowski P, Dzierzega M, Grosser K, Schmitz-Franken A, Rudolf H, et al. Sokrat II - an international, prospective, multicenter, phase IV diagnostic trial to evaluate the efficacy of the wrist SAFE algorithm in fracture sonography of distal forearm fractures in children. Ultraschall Med. 2019;40(3):349–58. https://doi.org/10.1055/a-0825-6284.
Douma-den Hamer D, Blanker MH, Edens MA, Buijteweg LN, Boomsna MF, van Helden Sh, et al. Ultrasound for distal forearm fracture: a systematic review and diagnostic meta-analysis. PLoS ONE. 2016;11(5):e0155659. https://doi.org/10.1371/journal.pone.0155659.
Joshi N, Lira A, Mehta N, Paladino L, Sinert R. Diagnostic accuracy of history, physical examination, and bedside ultrasound for diagnosis of extremity fractures in the emergency department: a systematic review. Acad Emerg Med. 2013;20(1):1–15. https://doi.org/10.1111/acem.12058.
Mobasseri A, Noorifard P. Ultrasound in the diagnosis of pediatric distal radius fractures: does it really change the treatment policy? An orthopedic view. J Ultrason. 2022;22(90):e179–82. https://doi.org/10.15557/jou.2022.0029.
Hübner U, Schlicht W, Outzen S, Barthel M, Halsband H. Ultrasound in the diagnosis of fractures in children. J Bone Joint Surg Br. 2000;82(8):1170–3. https://doi.org/10.1302/0301-620x.82b8.10087.
Snelling PJ, Keijzers G, Ware RS. Point of care ultrasound pronator quadratus hematoma sign for detection of clinically non angulated pediatric distal forearm fractures: a prospective cohort study. J Ultrasound Med. 2022;41(1):193–205. https://doi.org/10.1002/jum.15695.
Snelling PJ, Jones P, Gillespie A, Bade D, Keijzers G, Ware RS. Point of care ultrasound fracture-physis distance association with Salter-Harris II fractures of the distal radius in children: the “POCUS 1-cm rule.” Ultrasound Med Biol. 2023;49(2):520–6. https://doi.org/10.1016/j.ultrasmedbio.2022.10.002.
Snelling PJ, Jones P, Moore M, Gimpel P, Rogers R, Liew K, et al. Describing the learning curve of novices for the diagnosis of paediatric distal forearm fractures using point of care ultrasound. Australas J Ultrasound Med. 2022;25(2):66–73. https://doi.org/10.1002/ajum.12291.
Barata I, Spencer R, Suppiah A, Raio C, Ward MF, Sama A. Emergency ultrasound in the detection pediatric long bone fractures. Pediatr Emerg Care. 2012;28(11):1154–7. https://doi.org/10.1097/PEC.0b013e3182716fb7.
Troxler D, Sanchez C, de Trey T, Mayr J, Walther M. Non-inferiority of point-of-care ultrasound compared to radiography to diagnose upper extremity fractures in children. Children. 2022;9(10):1496. https://doi.org/10.3390/children9101496.
Musa S, Wilson P. Ultrasonography and radiography. A comparison Emerg Nurse. 2015;23(2):34–7. https://doi.org/10.7748/en.23.2.34.e1416.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. ID: conception of the work, study design, manuscript preparation, literature research, interpretation of data. VB: interpretation of data, statistical analysis. KK: critically revised the work and final approval of the version to be published. ED: conception of the work, interpretation of data, revising critically, and final approval of the version to be published. NG: final approval of the version to be published. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Delniotis, I., Bontinis, V., Ktenidis, K. et al. Diagnostic accuracy of ultrasound versus X-ray for distal forearm fractures in children and adolescents: a systematic review and meta-analysis. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-024-02451-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-024-02451-9