Abstract
Purpose
Patellar dislocation is a serious complication leading to patient morbidity following total knee arthroplasty (TKA). The cause can be multifactorial. Extensor mechanism imbalance may be present and result from technical errors such as malrotation of the implants. We sought to understand the reasons for post-arthroplasty patellar dislocation and the clinical outcomes of patients in whom it occurs.
Methods
This is a retrospective cohort study assessing the outcomes of revision surgery for patellar dislocation in patients with component malrotation in both primary and revision TKAs. Patient demographics, dislocation etiology, presurgical deformity, intraoperation component position, complications, reoperation, and Knee Society Scores (KSS) were collected.
Results
Twenty patients (21 knees) were identified. The average time from primary arthroplasty to onset of dislocation was 33.6 months (SD 44.4), and the average time from dislocation to revision was 3.38 months (SD 2.81). Seventeen knees (80.9%) had internal rotation of the tibial component and seven knees (33.3%) had combined internal rotation of both the femoral and tibial components. Fifteen knees (71.4%) were treated with a condylar constrained implant at the time of revision, and five knees were converted to a hinged prosthesis. The average follow-up time was 56 months. During this time, one patient (4.54%) had a recurrent dislocation episode, requiring further surgery. At final follow up, the mean KSS was 86.2.
Conclusion
Revision TKA following patellar dislocation for patients with malrotated components was associated with high success rates. After revision surgery, patients had a low recurrence of patellar dislocation, low complication rates, and excellent functional outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) has become one of the most successful operations of the past 2 decades with prosthetic survivorship in excess of 95% at 10-year follow-up [1]. Despite long-term survivorship and improved outcomes, with the increasing number of primary TKAs being performed, there has consequently been an increase in the absolute requirements for revision TKA [2]. A serious complications after TKA is patellar dislocation which is commonly a result of technical error [3] and with reported rates of up to 2% [4]. Several etiologies may lead to this undesirable outcome. Broadly speaking, the potential risk factors for patello-femoral (PF) dislocation can be categorized as follows: component malrotation, improper patellar preparation (button malposition or asymmetric bone resection), soft tissue imbalance (medial retinacular insufficiency, vastus medialis oblique weakness, quadriceps contracture, and iliotibial band tightness), limb valgus malalignment leading to abnormal extensor mechanism line of pull (affecting the Q angle), deficiencies in prosthetic design, and trauma [3, 5]. Rotation of both the femoral and tibial components play an important role in patellar tracking; therefore, malrotation of the femoral and tibial components may contribute to patellar dislocation [6].
In general, excessive internal rotation of the femoral component shifts the trochlear groove medially, placing it more distant from the patella, which then tracks laterally. This increases tension on the lateral retinaculum and exacerbates any tendency of the patella to subluxate or dislocate laterally [7]. On the other hand, excessive internal rotational of the tibial component causes the tibia to rotate externally during knee flexion, driving the tubercle laterally. This also leads to lateral patellar tracking and may cause the patella to subluxate or dislocate laterally [8]. Finally, a computerized tomography study by Planckaert et al. has shown that combined component internal rotation was associated with painful TKA [9].
The diagnosis of patellar dislocation is often apparent on clinical examination, and is usually confirmed radiographically on a merchant view. Although CT is considered the most accurate method to quantify the degree of rotational malalignment [6], several methods to assess for component malrotation utilizing plain radiographs have been described [10, 11] Furthermore, radiographically suspected component malrotation can be confirmed intraoperatively using pre-determined landmarks such as the trans-epicondylar axis and the femoral anterior tangent line [12, 13].
In patients with patellar dislocation, revision surgery is often necessary to regain the ability to ambulate. For those who experience component malrotation, several treatment options exist, such as medial patello-femoral ligament augmentation [14] or reconstruction [15] and tibial tuberosity osteotomy [16]. Prosthesis exchange may be curative [17]. Few studies have examined the outcomes of revision surgery for patellar dislocation following TKA and most studies have consisted of patient populations with heterogeneous etiologies. Furthermore, the treatment modalities utilized in these studies were mixed [3, 4, 18].
This study questions whether patients with dislocated patella resulting from malrotation would demonstrate improved functional outcomes (range of motion and Knee Society Score) after undergoing complete revision surgery of both the femoral and tibial components.
Materials and methods
Institutional research ethics board approval was obtained for this retrospective study.
The study group consisted of patients undergoing revision total knee arthroplasty for patellar dislocation at our tertiary care center between 2001 and 2018. Revisions were included in the study if they experienced PF dislocation, and at the time of revision, component malrotation was confirmed as the root cause. The tibial component was considered internally rotated if the rotational axis was directed medial to the medial third of the tibial tubercle. Excessive malrotation was defined in accordance with Drexler et al. [19], who demonstrated that alignment of the tibial component at the medial border of the tibial tuberosity would cause 6 ° of tibial internal rotation. The femoral component was considered internally rotated if it was found to be internally rotated relative to the trans-epicondylar axis. Patients with infection or aseptic loosening of components were excluded from the study. Data were gathered from the patients’ electronic medical records and included gender, age, body mass index (BMI), American Society of Anesthesiologists score (ASA), the etiology for primary arthroplasty, time from primary arthroplasty to instability, time to dislocation, and dislocation etiology. At the time of revision surgery, component fixation, rotation, and soft tissue status were assessed. The components utilized at the time of revision and details regarding soft tissue releases and plication were noted. Additionally, complications and reoperation rates were collected.
Preoperative and postoperative radiographs including long leg standing films, knee anteroposterior (AP), lateral, and merchant views were reviewed. Patellar dislocation was confirmed on the merchant view, whereas long leg standing radiographs were evaluated for limb axial alignment and Q angle. Furthermore, vertical patellar position was measured on lateral plain radiographs using the Insall–Salvati ratio [20]. Patella baja and alta were considered if the ratio was < 0.8 or > 1.2, respectively. When CT scans were performed at outside institutions prior to transfer for revision surgery, these were reviewed for tibial and femoral implant rotation. Routine practice at our center has consisted of a preliminary screening radiographic assessment for component malrotation. Lateral X-rays are assessed for suspected femoral component malrotation. Anteroposterior films are then screened for suspected tibial component malrotation. This is confirmed intraoperatively at the time of revision surgery utilizing the trans-epicondylar axis [13]. Range of motion was documented in all patients by an advanced practice physiotherapist using a standard goniometer. At final follow-up, we collected patient Knee Society Scores (KSS) [21].
Statistical analysis was performed with SPSS software, version 25 (IBM, Armonk, NY). Descriptive analyses were performed for both continuous and categorical variables. Continuous variables were presented as means with associated standard deviations (SD). Categorical variables were presented as absolute and relative frequencies. A P value less than or equal to 0.05 was treated as statistically significant. Information regarding missing data is stated below each table.
Results
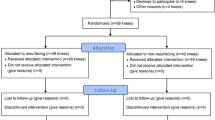
Between November 2001 and September 2018, 787 total knee revisions were performed at our institute by the senior author. Thirty-six cases underwent revision TKA surgery for patellar dislocation. Out of this group, 20 patients (21 knees) were found to have malrotated components during surgery (Fig. 1). All patients were referred to our academic, tertiary care center from outside hospitals. There were 13 females and 7 males (Table 1). The average age at the time of revision surgery was 67 years (SD 8.6; range 49–78 years). The pre-arthroplasty diagnoses included osteoarthritis in 18 patients, rheumatoid arthritis in 2 patients and post-traumatic osteoarthritis in 1 patient. The average number of surgeries performed prior to revision at our center was 2.1 ± 1.4 (range 1–7). Eight knees (38%) underwent an attempt at management with a soft tissue repair (lateral retinacular release, medial patellar plication, patellar tendon reconstruction, and irrigation and drainage) at the referring center prior to revision surgery at our institution. The average time from primary arthroplasty to the onset of instability was 17.3 months (SD 41.3; range 0–168 months), and the average time to dislocation was 33.6 months (SD 44.4; range 1–180 months). The average time from dislocation to revision was 3.38 months (SD 2.81; range 0.5–12 months). The etiology of dislocation was non-traumatic in 12 knees (57%) and secondary to an inciting traumatic event in 9 knees (43%).
Assessment of preoperative four foot standing alignment views identified 11 knees (52.4%) with valgus alignment and 8 in varus alignment. Furthermore, 12 knees (57.1%) were found to have a patella alta. The mean Insall–Salvati ratio for this subset of patients was 1.47 ± 0.27 (range 1.25–2.08) whereas the mean Insall–Salvati ratio for the entire cohort was 1.3 ± 0.32 (range 0.77–2.08). The average Q angle for the cohort was 15.8 ° (SD 44.4; range range 6.7–31.6); 12.7 ° for males and 20.6 ° females.
At the time of surgery, no patients were found to have implant loosening. Seventeen knees (80.9%) had an internally rotated tibial component, 11 knees (52.3%) had an internally rotated femoral component and 7 knees (33.3%) had internal rotation of both components. The average patellar thickness was 15.4 ± 4.06 mm (range 8–25 mm) and eight patellar buttons (38%) were found to be placed laterally. Revision components used were unlinked condylar constrained in 15 knees (71.4%), hinged prosthesis in 5 knees and a posterior stabilized revision implant in 1 knee. Lateral release was performed in 14 knees (66.7%) and medial plication in 4 knees (19%). Intra operative data are summarized in Table 2.
The average follow-up time was 56 ± 33.1 months (range 5–145 months). Two patients (9.5%) had complications following revision surgery. One patient had a recurrent dislocation episode secondary to repeat falls that eventually led to patellectomy (Fig. 2). The second patient had a tibial tuberosity fracture as a result of a fall 5 months post-revision surgery, which was fixed and healed uneventfully. The mean Knee Society Score, at final follow-up, for the patient cohort was 86.2. The mean range of motion at final follow-up was from full extension to 115 ° of flexion.
Discussion
Patellar dislocation, although rare, is a serious complication following total knee arthroplasty that is associated with decreased functional outcomes and revision surgery. Malrotation of the femoral and tibial components are important contributors to patellar dislocation. Berger et al. demonstrated that combined excessive internal component rotation correlated directly with the severity of the patello-femoral complication. In their study, malrotation between 7 and 17 ° resulted in patellar dislocation [6]. In the current study, most of the patients (80.9%) had an excessive internal rotation of the tibial implant, whereas a smaller percentage (33.3%) had both femoral and tibial component malrotation. Our results support those of Figgie et al. who stated that excessive tibial component rotation had the highest influence on patellar dislocation rates compared with femoral component malrotation [22].
In our cohort, 9 patients (42.9%) experienced patellar dislocation following a traumatic episode, all of whom were found to have malrotated components intra-operatively. We propose that in such cases, it is possible that component malrotation may have been the culprit for PF dislocation and that trauma may have resulted secondarily (i.e. a fall).
Interestingly, 9 patients (45%) who presented with patellar dislocation experienced a sense of patellar instability in the early post-operative period after their primary TKA but only dislocated their patella at an average of 26 months post-operatively. We postulate that in asymptomatic patients with component malrotation, the onset of pain and instability may present in a delayed fashion through two mechanisms. First, component malrotation may, over time, lead to attrition of the ligamentous checkrein mechanisms eventually leading to PF dislocation. Second, failure of PF soft tissue supports may be accelerated or caused by an inciting traumatic event leading to PF dislocation. According to Motsis et al., in the context of patellar dislocation, a history of persistent pain immediately following the index TKA procedure is more likely to be related to the surgical technique; whereas a sudden onset of instability after an asymptomatic period is more likely related to failure of the component or soft tissues [23]. However, in our study, six patients who were asymptomatic after their primary arthroplasty procedure experienced a sense of instability for a duration of 7–168 months post-operatively. These patients were also all found to have malrotated components during the revision surgery. Surprisingly, these patients initially tolerated the malrotation and were largely asymptomatic.
Furthermore, five patients out of the eight who underwent an attempt with soft tissue repair prior to the complete revision at our center were treated with lateral retinacular release. According to Arnd et al., a lateral retinacular release reduces internal rotation of the tibia [24]; we assume that this procedure might have delayed the dislocation of the patella in these patients.
Lastly, all patients in this study’s cohort sustained additional technical errors besides the malrotated components (Table 3). This suggests that patellar dislocation is a multifactorial entity requiring a thorough preoperative evaluation, including a detailed clinical and radiographic evaluation. In addition, further workup for infection and osteolysis should be considered when appropriate.
The current study demonstrates that patients undergoing revision total knee following patellar dislocation achieve satisfactory KSS following revision. Kingsley et al. evaluated the functional outcomes of 39 patients undergoing revision TKA due to patellar dislocations. In their cohort, two-thirds of the patients had residual disability and pain. The average Knee Society Score improved by only 42 points, reaching a score of 77 points [3]. However, Kingsley had several limitations that we controlled for in our study. First, their cohort was not homogeneous with regard to component alignment and methods of treatment. Only nine patients (23%) from the Kingsley’s cohort had malrotation of the components, whereas the current study group patients all had malrotation diagnosed. Second, in contrast to Kingsley et al., all the patients in our study underwent revision of both the femoral and tibial components. Therefore, we believe that full-component revision leads to better clinical results compared to partial revision [25]. Lastly, in contrast to Kingsley et al., patients with infection or aseptic loosening were excluded from our study. These conditions may contribute to dislocation and, therefore, confound the clinical utility of that study’s results.
There are several limitations to the current study. First, the study is retrospective in nature which has the potential to bias the findings. Second, data regarding the precise magnitude of malrotation were not measured intra-operatively which prevents precise quantitative assessment of the degree of malrotation which may be clinically relevant. Assessment with preoperative CT scans in the study patients may have improved the ability to quantify the degree of malrotation and further compliment intraoperative assessment. Furthermore, there was variation in re-operations performed at other centers prior to being transferred to our care. This led to differences in the total number and types of procedures performed on patients which may have affected final outcomes overall. Lastly, although the KSS score was utilized to assess post-operative outcomes, we were unable to assess pre-operative scores because of severe impairments in patient function.
In conclusion, revision surgery of both the femur and tibia for patellar dislocation in patients with malrotated TKA components appears to be beneficial. Complete component revision led to excellent results in the current study, and should be considered over soft tissue procedure or partial revision for patients with patello-femoral instability and confirmed component malrotation.
References
Jauregui JJ, Cherian JJ et al (2015) Long-term survivorship and clinical outcomes following total knee arthroplasty. J Arthroplast 30:2164–2166. https://doi.org/10.1016/j.arth.2015.05.052
Sharkey PF, Lichstein PM, Shen C et al (2013) Why are total knee arthroplasties failing today-has anything changed after 10 years? J Arthroplast 29:1774–1778. https://doi.org/10.1016/j.arth.2013.07.024
Chin KR, Bae DS, Lonner JH, Scott RD (2004) Revision surgery for patellar dislocation after primary total knee arthroplasty. J Arthroplast 19:956–961. https://doi.org/10.1016/j.arth.2004.03.018
Kirk P, Rorabeck CH, Bourne RB et al (1992) Management of recurrent dislocation of the patella following total knee arthroplasty. J Arthroplast 7:229–233. https://doi.org/10.1016/0883-5403(92)90041-N
Malo M, Vince KG (2003) The unstable patella after total knee arthroplasty: etiology, prevention, and management. J Am Acad Orthop Surg 11:364–371
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199811000-00021
Rahman WA, Vial TA, Backstein DJ (2016) Distal femoral arthroplasty for management of periprosthetic supracondylar fractures of the femur. J Arthroplast 31:676–679. https://doi.org/10.1016/j.arth.2015.09.042
Motsis EK, Paschos N, Pakos EE, Georgoulis AD (2009) Review article: Patellar instability after total knee arthroplasty. J Orthop Surg 17:351–357. https://doi.org/10.1177/230949900901700322
Planckaert C, Larose G, Ranger P et al (2018) Total knee arthroplasty with unexplained pain: new insights from kinematics. Arch Orthop Trauma Surg 138:553–561. https://doi.org/10.1007/s00402-018-2873-5
Takai S, Yoshino N, Isshiki T, Hirasawa Y (2003) Kneeling view: a new roentgenographic technique to assess rotational deformity and alignment of the distal femur. J Arthroplast 18:478–483. https://doi.org/10.1016/S0883-5403(03)00065-2
Qin CH, Pei GX, Luo JW (2007) Axial radiography of the distal femur to access rotational alignment in total knee arthroplasty. J Clin Rehabil Tissue Eng Res 11:3124–3126. https://doi.org/10.1097/01.blo.0000156819.24866.8b
Watanabe H, Gejo R, Matsuda Y et al (2011) Femoral anterior tangent line of the osteoarthritic knee for determining rotational alignment of the femoral component in total knee arthroplasty. J Arthroplast 26:268–273. https://doi.org/10.1016/j.arth.2009.12.011
Berger R, Rubash HE, Seel MJ et al (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199301000-00008
Lamotte A, Neri T, Kawaye A et al (2016) Medial patellofemoral ligament reconstruction for patellar instability following total knee arthroplasty: a review of 6 cases. Orthop Traumatol Surg Res 102:607–610. https://doi.org/10.1016/j.otsr.2016.03.018
van Gennip S, Schimmel JJP, van Hellemondt GG et al (2014) Medial patellofemoral ligament reconstruction for patellar maltracking following total knee arthroplasty is effective. Knee Surg Sports Traumatol Arthrosc 22:2569–2573. https://doi.org/10.1007/s00167-012-2269-y
Whiteside LA (1997) Distal realignment of the patellar tendon to correct abnormal patellar tracking. Clin Orthop Relat Res 344:284–289
Putman S, Boureau F, Girard J et al (2018) Patellar complications after total knee arthroplasty. Orthop Traumatol Surg Res. https://doi.org/10.1016/j.otsr.2018.04.028
Simmons E Jr, Cameron JC (1992) Patella alta and recurrent dislocation of the patella. Clin Orthop Relat Res. https://doi.org/10.1097/01241398-199207000-00054
Drexler M, Backstein D, Studler U et al (2017) The medial border of the tibial tuberosity as an auxiliary tool for tibial component rotational alignment during total knee arthroplasty (TKA). Knee Surg Sports Traumatol Arthrosc 25:1736–1742. https://doi.org/10.1007/s00167-016-4072-7
Insall J, Salvati E (1971) Patella position in the normal knee joint. Radiology 101:101–104. https://doi.org/10.2320/jinstmet.J2015027
Ewald F (1989) Roentgenographic evaluation and scoring system. Clncal Orthop Relat Res. https://doi.org/10.1016/j.otsr.2010.06.008
Figgie HE 3rd, Goldberg VM, Figgie MP et al (1989) The effect of alignment of the implant on fractures of the patella after condylar total knee arthroplasty. J Bone Jt Surg Am 71:1031–1039
Motsis EK, Paschos N, Pakos EE, Georgoulis AD (2009) Review article: patellar instability after total knee arthroplasty. J Orthop Surg 17:351–357. https://doi.org/10.1177/230949900901700322
Steinbruck A, Schroder C, Woiczinski M et al (2018) A lateral retinacular release during total knee arthroplasty changes femorotibial kinematics: an in vitro study. Arch Orthop Trauma Surg 138:401–407. https://doi.org/10.1007/s00402-017-2843-3
Fehring TK, Odum S, Griffin WL, Mason JB (2005) Outcome comparison of partial and full component revision TKA. Clin Orthop Relat Res. https://doi.org/10.1097/01.blo.0000186560.70566.dc
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Warschawski, Y., Garceau, S., Frenkel Rutenberg, T. et al. Revision total knee arthroplasty for patellar dislocation in patients with malrotated TKA components. Arch Orthop Trauma Surg 140, 777–783 (2020). https://doi.org/10.1007/s00402-020-03468-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03468-6